Mechanic's hands (MH) is a clinical sign associated with various rheumatological diseases, with antisynthetase syndrome being the most commonly described. This finding is widely defined as the presence of hyperkeratosis, scaling, and non-pruritic fissuring on the ulnar side of the thumb and the radial side of the other fingers. However, histological examination is essential for diagnostic confirmation.1
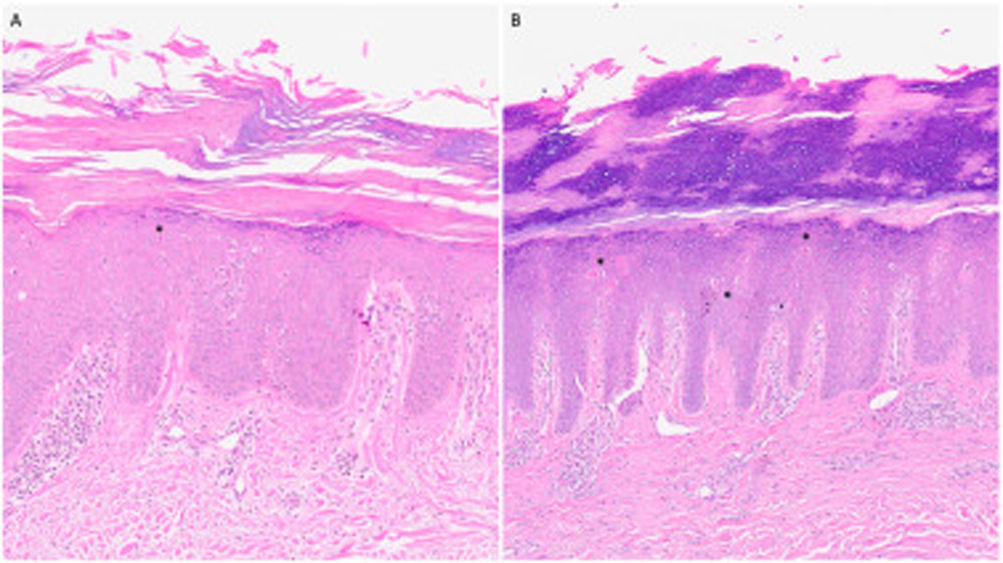
A 65-year-old man, with a past medical history of nonspecific arthralgias, was referred from the Rheumatology department for evaluation of psoriasiform lesions. Physical examination revealed the presence of hyperkeratotic, scaling, and fissured plaques on the ulnar side of the thumbs, the radial side of the other fingers, on the pads of all fingers, as well as on the knees, elbows, and the soles of the feet (Fig. 1A-D). Autoimmune testing showed no relevant findings, and the diagnosis of vulgar psoriasis was established with topical treatment using corticosteroids and calcipotriol, which led to minimal improvement. Due to the persistence of skin and joint symptoms, methotrexate was initiated, resulting in modest improvement. At the follow-up, the patient developed respiratory symptoms including dry cough and dyspnea, and was referred to Pulmonology, where he was finally diagnosed with nonspecific interstitial pneumonia (NIP). In this context, the diagnosis of psoriasis was reconsidered, and a skin biopsy was performed on both hand and elbow lesions. Histological examination revealed alternating checkerboard hyperkeratosis with regular acanthosis, along with the presence of apoptotic keratinocytes in the form of colloid bodies (eosinophilic homogeneous structures located in the epidermis) (Fig. 2), consistent with the diagnosis of MH. A histochemical study with PAS did not show mucin deposits. Once the diagnosis was confirmed, a new autoimmunity serology test was performed, which turned out positive for anti-PM-Scl antibodies. With the diagnosis of MH in the context of overlap syndrome, the patient was treated with mycophenolate mofetil, achieving remission of skin lesions and stability of pulmonary involvement in functional tests and imaging.
MH represents a clinical finding associated with different clinical and immunological phenotypes, which causes significant confusion on its meaning and prognostic value. Generally, MH is associated with antisynthetase syndrome and the presence of related antibodies (anti-JO, anti-OJ, anti-PL 7, or anti-PL 12).2 However, we should mention that it can also appear alongside antibodies characteristic of other autoimmune diseases, such as scleroderma, dermatomyositis, lupus, or rheumatoid arthritis.3 Additionally, we should mention that this sign may precede the positivity of antibodies, so antibody negativity does not rule out diagnosis requiring the monitoring of these patients. Moreover, despite being commonly described on the hands, this sign has also been described on the soles (referred to in the literature as “walker's feet”) and other locations such as knees or elbows, as it was the case with our patient.4 This makes diagnosis easily confused with other desquamative processes and should be suspected in patients with psoriasis resistant to various lines of therapy. Although the diagnosis of MH requires a high clinical suspicion, and it frequently appears as an isolated skin sign in the context of antisynthetase syndrome, other skin signs suggestive of dermatomyositis should be ruled out, such as Gottron's sign, Gottron's papules, periungual telangiectasias, heliotrope rash, or rashes in sun-exposed areas and other less widely associated connective tissue diseases, such as systemic lupus erythematosus or scleroderma.3 Although histological findings are not completely pathognomonic, the observation of a checkerboard pattern of hyperkeratosis or the presence of colloid bodies is essential to distinguish it from other skin diseases, such as chronic hand eczema or psoriasis2 (Table 1). Regarding anti-PM-Scl antibodies, they are frequently associated with overlap syndromes of scleroderma and dermatomyositis. Breillat et al. conducted a retrospective observational study with 142 patients and observed that patients with MH and anti-PM-Scl antibodies are expected to have a better prognosis for pulmonary disease vs those with the same antibody profile but a predominant scleroderma phenotype without MdM.5
Differential diagnosis of the most common histological features of psoriasis, chronic hand eczema, and mechanic's hands.
| Feature | Psoriasis | Mechanic's hands | Chronic eczema |
|---|---|---|---|
| Epidermis | Hyperkeratosis with parakeratosisHypogranulosisAcanthosisNeutrophils | Checkerboard hyperkeratosis, alternating orthokeratosis and parakeratosisColloid bodiesAcanthosisMucin deposits | Hyperkeratosis with occasional small foci of parakeratosisHypergranulosisAcanthosisPsoriasiform hyperplasia |
| D-E Junction | Dilated vessels | Interface dermatitis | |
| Dermis | Edema | Mucin deposits | Vertically oriented collagen |
In conclusion, it is crucial to recognize that clinical suspicion of MH is essential for the early diagnosis of some rheumatological diseases, as it may precede antibody positivity and predict potential development of pulmonary disease. Therefore, it is essential to be aware of the possible locations of this entity beyond the hands and its histological characteristics.
Conflicts of interestNone declared.