In 2017, the Spanish Academy of Dermatology and Venereology Psoriasis Working Group (PWG) designed the Minimal Disease Activity (MDA) criteria to determine the level of disease activity. We hereby present the results of an observational, cross-sectional, multicenter study of the nationwide application of these criteria.
Material and methodsWe conducted a non-randomized sampling, stratified to achieve autonomic and provincial representation of consecutive patients with psoriasis (Ps) vulgaris without active arthritis. A total of 830 patients were included: 493 men (59.5%), with a mean age of 51.4 years (SD, 14.2), from all autonomous regions of Spain (except for Ceuta and Melilla) and 44 (88%) out of the 50 provinces. A questionnaire was obtained with demographic data, DLQI, subjective assessment—on a scale from 0 to 10—of itching, erythema, desquamation, visibility, and the patients’ PASI and BSA.
ResultsMore than 50% failed to meet the MDA criteria (491; 59.2%), with significant differences being reported by region, sex, and age. Additionally, significant differences were reported based on the therapy used (P<.001). The use of biological therapies was associated with higher MDA compliance compared to other therapies (59.4% vs 23.3%). No differences were reported among various biological therapies.
ConclusionsThe overall rate of MDA compliance is low, with differences being based on geographic location, sex, age, and drug used, yet none of these factors separately justify them.
El Grupo de Psoriasis de la Academia Española de Dermatología y Venereología (GPs) diseño en 2017 la medida Actividad Mínima de Enfermedad en Psoriasis (AME). Se presentan los resultados de un estudio observacional, transversal y multicéntrico de la aplicación de esta escala a nivel nacional.
Material y métodosSe realizó un muestreo no aleatorizado, estratificado para alcanzar representación autonómica y provincial, de pacientes consecutivos con psoriasis (Ps) vulgar sin artritis activa. Se incluyeron 830 pacientes: 493 eran varones (59,5%), con una edad media de 51,4 años (DE=14,2), de todas las autonomías del país (excepto Ceuta y Melilla) y 44 (88%) de las 50 provincias. Se obtuvo un cuestionario recogiendo datos demográficos, DLQI, valoración subjetiva en escalas de 0 a 10 de picor, eritema, descamación y visibilidad; y el PASI y el BSA del paciente.
ResultadosMás de la mitad no cumplían criterio de AME (491; 59,2%), con diferencia significativa entre regiones, por el sexo y por la edad. También había diferencias según el tratamiento realizado (p<0,001). El uso de un medicamento biológico se asoció a un mayor cumplimiento AME frente al uso de otro tipo de medicamentos (59,4 vs. 23,3%). No se observaron diferencias entre los tratamientos biológicos.
ConclusionesEl porcentaje global de cumplimiento AME es bajo, con diferencias por la localización geográfica, el sexo, la edad y el fármaco utilizado, si bien ninguno de esos factores por separado las justifica.
According to the World Health Organization (WHO), psoriasis (Ps) is a chronic, non-communicable, painful, disfiguring, and disabling disease, with no cure and a significant negative impact on the patient's quality of life (QoL).1
Despite therapeutic advances, some patients do not achieve complete clearance of skin signs or continue to have other issues that negatively affect their QoL.2 This, along with differing expectations and priorities between dermatologists and patients in disease management,3 requires changes to adjust treatment on an individual basis, objectively measuring results4,5 to achieve a holistic approach to disease management.6
Disease severity measures can be objective (Psoriasis Activity Skin Index [PASI], Body Surface Area [BSA], or percentage of skin affected; Physician Global Assessment [PGA]), or subjective, evaluated by the patient (Dermatology Life Quality Index [DLQI]). However, each of these indices has intrinsic limitations, as previously mentioned.7
In 2017, the Psoriasis Working Group (PWG) of the Spanish Academy of Dermatology and Venereology embarked on a project to create a measure that jointly assessed the impact of the disease between patient and dermatologist, which gave birth to the Minimal Disease Activity in Psoriasis (MDA).7 MDA includes the dermatologist's evaluation of the BSA, presence or absence of special localization, and the exclusion of arthritis. The patient scores the DLQI and quantifies the intensity of itching (0-10), erythema (0-10), scaling (0-10), and visibility (0-10). MDA is met in the absence of active arthritis plus 3 of the following items: itching ≤ 1/10; scaling ≤ 2/10; redness ≤ 2/10; visibility ≤ 2/10; BSA ≤ 2; DLQI ≤ 2, and no lesions in special locations.
The objective of our study was to describe the MDA situation in the routine clinical practice in Spain.
Materials and methodsWe conducted a national, observational, cross-sectional, and multicenter study. Each region provided information from 10 dermatologists through one coordinator. Participant dermatologists consecutively collected data from 5 patients with plaque Ps and no active arthritis. Informed consent, epidemiological and clinical data (sex, age, therapeutic status, and drug used; presence or absence of special location; and confirmation of the absence of active arthritis), PASI, BSA, DLQI, as well as patient-reported intensity of itching, erythema, scaling, and visibility were collected.
Data were entered by each regional coordinator into a web platform specifically designed by the research unit of AEDV, responsible for the analysis.
A descriptive analysis was conducted where continuous variables were expressed as mean and standard deviation (SD), median, first and third quartile, and maximum and minimum. Differences were evaluated using the Student's t-test or the Mann-Whitney U test. Qualitative variables were expressed as absolute and relative frequencies, and differences were evaluated using the chi-square test. A smoothed line chart of the probability of not meeting MDA criteria based on PASI was created to determine an optimal cut-off point through logistic regression. Finally, multivariable logistic regression adjusted by region was used to determine the association between meeting MDA criteria and different epidemiological and clinical characteristics.
The study was approved by Hospital Universitario de Gran Canaria Dr. Negrín Ethics Committee of (2022-299-1). All patients gave their consent to participate in the study.
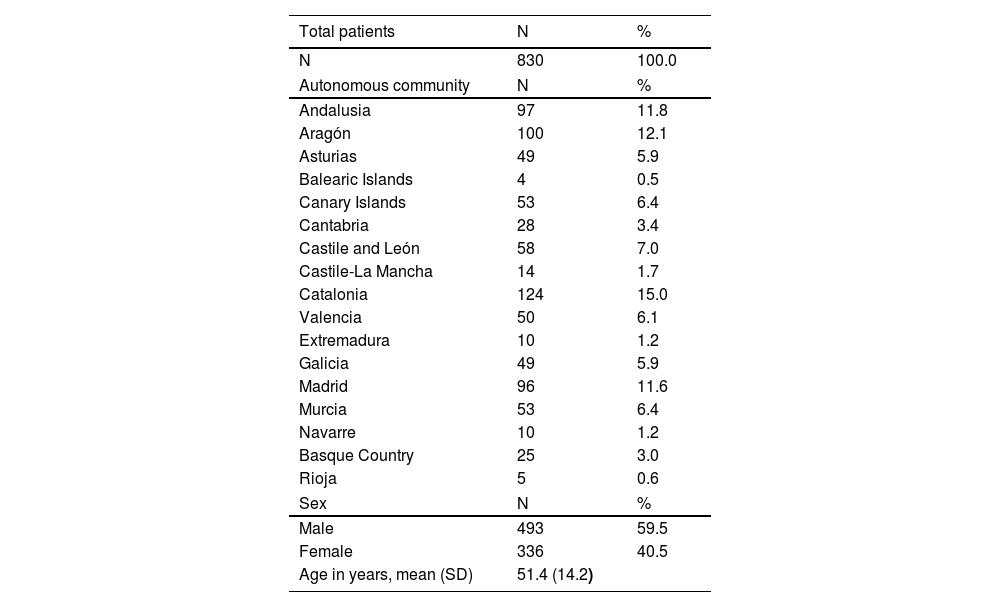
ResultsA total of 18 coordinators and 180 dermatologists from across Spain participated in the study collecting data from 830 patients with vulgar Ps and without active arthritis. Data were obtained from 17 autonomous communities—except for Ceuta and Melilla—and 44 of the 50 provinces, with differences across regions: Catalonia 124 patients, maximum; Balearic Islands, 4 patients, minimum). Of these, 493 were men (59.5%) with a mean age of 51.4 years (SD, 14.2 years) (Table 1).
Demographic data.
| Total patients | N | % |
|---|---|---|
| N | 830 | 100.0 |
| Autonomous community | N | % |
| Andalusia | 97 | 11.8 |
| Aragón | 100 | 12.1 |
| Asturias | 49 | 5.9 |
| Balearic Islands | 4 | 0.5 |
| Canary Islands | 53 | 6.4 |
| Cantabria | 28 | 3.4 |
| Castile and León | 58 | 7.0 |
| Castile-La Mancha | 14 | 1.7 |
| Catalonia | 124 | 15.0 |
| Valencia | 50 | 6.1 |
| Extremadura | 10 | 1.2 |
| Galicia | 49 | 5.9 |
| Madrid | 96 | 11.6 |
| Murcia | 53 | 6.4 |
| Navarre | 10 | 1.2 |
| Basque Country | 25 | 3.0 |
| Rioja | 5 | 0.6 |
| Sex | N | % |
| Male | 493 | 59.5 |
| Female | 336 | 40.5 |
| Age in years, mean (SD) | 51.4 (14.2) | |
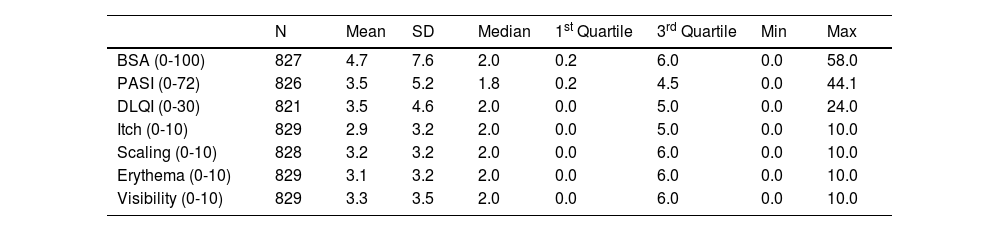
The mean disease severity values as measured by dermatologist and patient were: BSA, 4.7; PASI, 3.5; DLQI, 3.5; itching, 2.9; scaling, 3.2; erythema, 3.1; visibility, 3.3 (Table 2).
Global clinical description.
| N | Mean | SD | Median | 1st Quartile | 3rd Quartile | Min | Max | |
|---|---|---|---|---|---|---|---|---|
| BSA (0-100) | 827 | 4.7 | 7.6 | 2.0 | 0.2 | 6.0 | 0.0 | 58.0 |
| PASI (0-72) | 826 | 3.5 | 5.2 | 1.8 | 0.2 | 4.5 | 0.0 | 44.1 |
| DLQI (0-30) | 821 | 3.5 | 4.6 | 2.0 | 0.0 | 5.0 | 0.0 | 24.0 |
| Itch (0-10) | 829 | 2.9 | 3.2 | 2.0 | 0.0 | 5.0 | 0.0 | 10.0 |
| Scaling (0-10) | 828 | 3.2 | 3.2 | 2.0 | 0.0 | 6.0 | 0.0 | 10.0 |
| Erythema (0-10) | 829 | 3.1 | 3.2 | 2.0 | 0.0 | 6.0 | 0.0 | 10.0 |
| Visibility (0-10) | 829 | 3.3 | 3.5 | 2.0 | 0.0 | 6.0 | 0.0 | 10.0 |
SD: standard deviation.
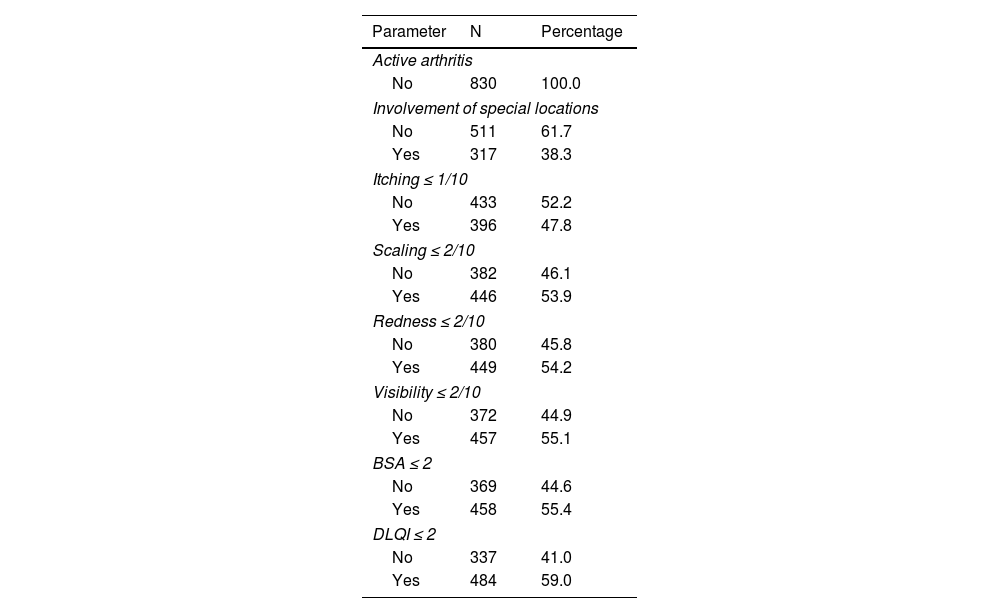
A total of 61.7% had no lesions in special locations, 47.8% had itching ≤ 1/10; 53.9%, scaling ≤ 2/10; 54.2%, redness ≤ 2/10; 55.1%, visibility ≤ 2/10; 55.4%, BSA ≤ 2; and 59%, DLQI ≤ 2 (Table 3).
Values of parameters for MDA criteria.
| Parameter | N | Percentage |
|---|---|---|
| Active arthritis | ||
| No | 830 | 100.0 |
| Involvement of special locations | ||
| No | 511 | 61.7 |
| Yes | 317 | 38.3 |
| Itching ≤ 1/10 | ||
| No | 433 | 52.2 |
| Yes | 396 | 47.8 |
| Scaling ≤ 2/10 | ||
| No | 382 | 46.1 |
| Yes | 446 | 53.9 |
| Redness ≤ 2/10 | ||
| No | 380 | 45.8 |
| Yes | 449 | 54.2 |
| Visibility ≤ 2/10 | ||
| No | 372 | 44.9 |
| Yes | 457 | 55.1 |
| BSA ≤ 2 | ||
| No | 369 | 44.6 |
| Yes | 458 | 55.4 |
| DLQI ≤ 2 | ||
| No | 337 | 41.0 |
| Yes | 484 | 59.0 |
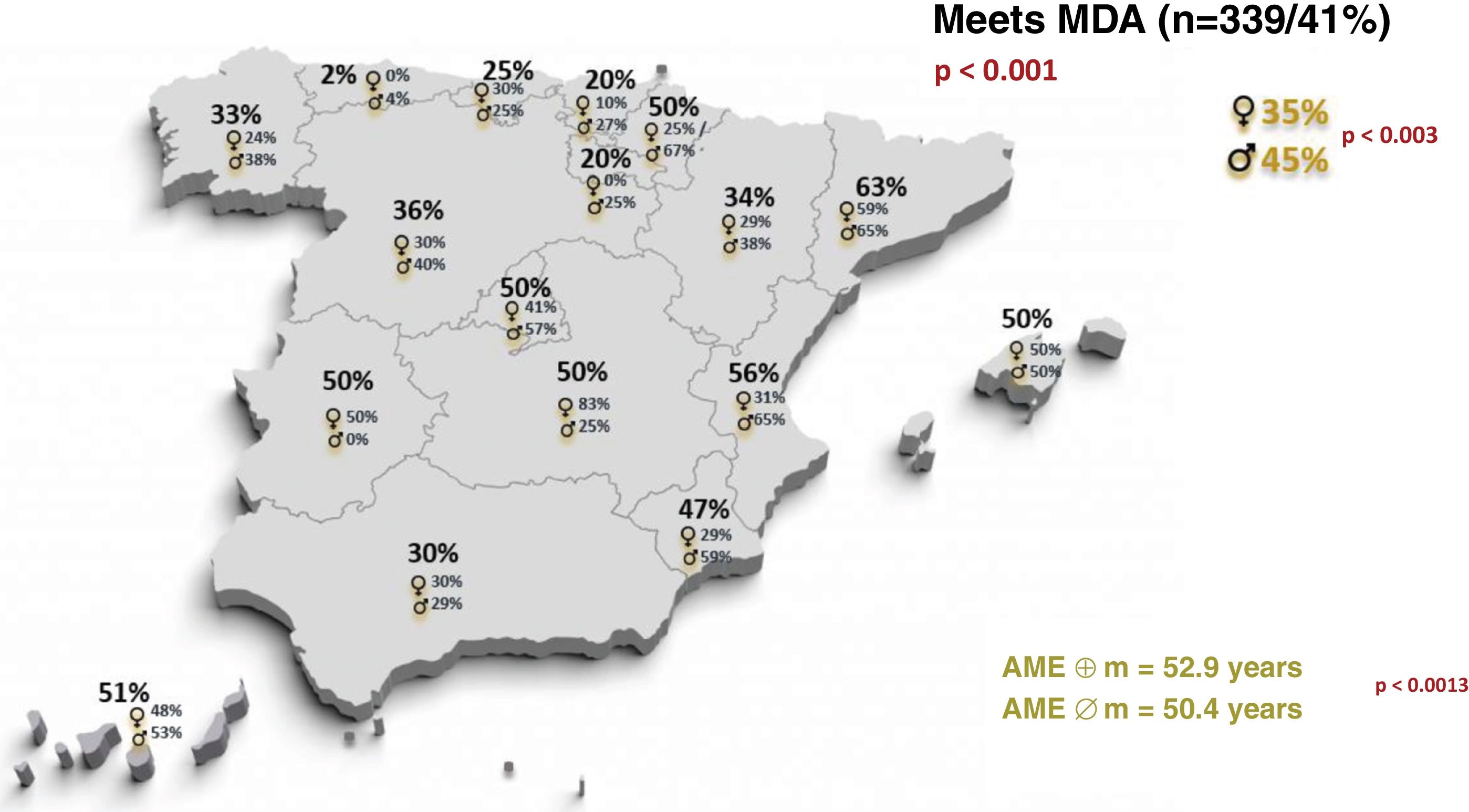
More than half of the patients (491; 59.2%) did not meet MDA criteria, and we found significant differences across regions (highest frequency in Asturias: 98%; lowest in Catalonia: 37.1%) (p <0.001) (Graph 1).
MDA compliance showed significant differences by sex and age. Men had a higher percentage of MDA compliance (222 patients, 45.0% vs 117 women, 34.8%) (p <0.003), as did older patients (mean age, 52.9 years; SD, 14.3) vs younger patients (50.4 years; SD, 14) (p <0.013). Additionally, differences in compliance by sex were seen across regions (Graph 1).
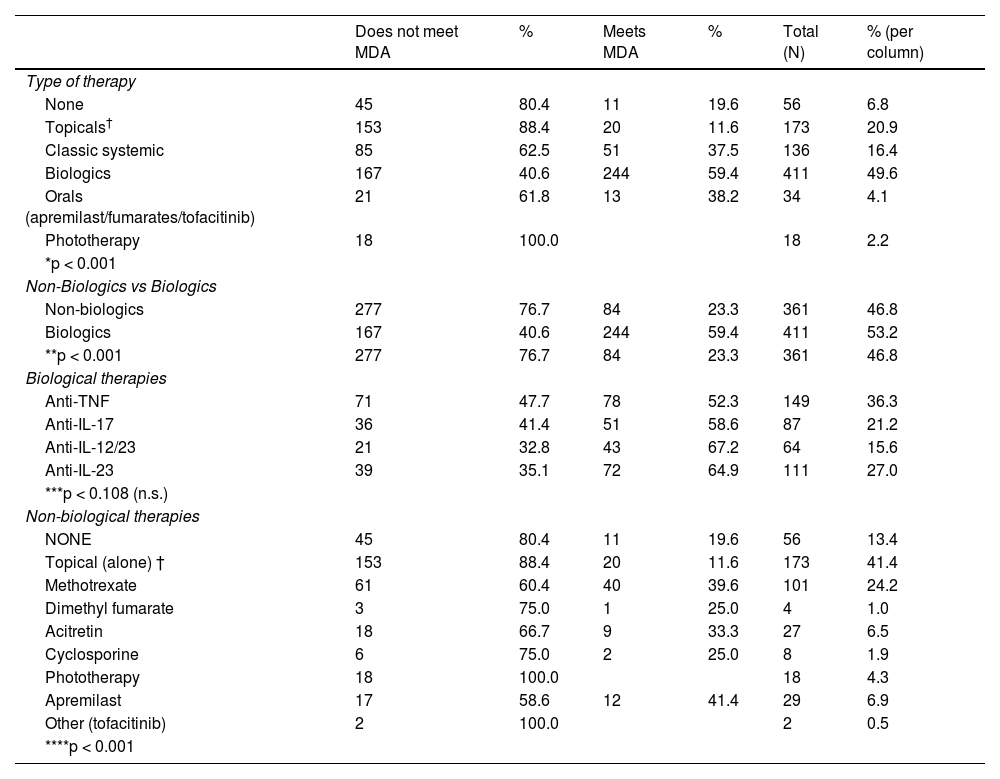
Additionally, differences were reported in MDA compliance based on treatment (p <0.001). Biological therapy was associated with higher MDA compliance vs non-biological therapy (59.4% vs 23.3%). Although no differences were seen between different biological therapies (p=0.108), significant differences were found vs non-biological therapies (p <0.001) (Table 4).
MDA compliance and antipsoriatic treatment.
| Does not meet MDA | % | Meets MDA | % | Total (N) | % (per column) | |
|---|---|---|---|---|---|---|
| Type of therapy | ||||||
| None | 45 | 80.4 | 11 | 19.6 | 56 | 6.8 |
| Topicals† | 153 | 88.4 | 20 | 11.6 | 173 | 20.9 |
| Classic systemic | 85 | 62.5 | 51 | 37.5 | 136 | 16.4 |
| Biologics | 167 | 40.6 | 244 | 59.4 | 411 | 49.6 |
| Orals (apremilast/fumarates/tofacitinib) | 21 | 61.8 | 13 | 38.2 | 34 | 4.1 |
| Phototherapy | 18 | 100.0 | 18 | 2.2 | ||
| *p < 0.001 | ||||||
| Non-Biologics vs Biologics | ||||||
| Non-biologics | 277 | 76.7 | 84 | 23.3 | 361 | 46.8 |
| Biologics | 167 | 40.6 | 244 | 59.4 | 411 | 53.2 |
| **p < 0.001 | 277 | 76.7 | 84 | 23.3 | 361 | 46.8 |
| Biological therapies | ||||||
| Anti-TNF | 71 | 47.7 | 78 | 52.3 | 149 | 36.3 |
| Anti-IL-17 | 36 | 41.4 | 51 | 58.6 | 87 | 21.2 |
| Anti-IL-12/23 | 21 | 32.8 | 43 | 67.2 | 64 | 15.6 |
| Anti-IL-23 | 39 | 35.1 | 72 | 64.9 | 111 | 27.0 |
| ***p < 0.108 (n.s.) | ||||||
| Non-biological therapies | ||||||
| NONE | 45 | 80.4 | 11 | 19.6 | 56 | 13.4 |
| Topical (alone) † | 153 | 88.4 | 20 | 11.6 | 173 | 41.4 |
| Methotrexate | 61 | 60.4 | 40 | 39.6 | 101 | 24.2 |
| Dimethyl fumarate | 3 | 75.0 | 1 | 25.0 | 4 | 1.0 |
| Acitretin | 18 | 66.7 | 9 | 33.3 | 27 | 6.5 |
| Cyclosporine | 6 | 75.0 | 2 | 25.0 | 8 | 1.9 |
| Phototherapy | 18 | 100.0 | 18 | 4.3 | ||
| Apremilast | 17 | 58.6 | 12 | 41.4 | 29 | 6.9 |
| Other (tofacitinib) | 2 | 100.0 | 2 | 0.5 | ||
| ****p < 0.001 | ||||||
Subjective symptoms reported by patients—itching, scaling, erythema, visibility—were the main reason for not meeting MDA, mainly itching> 1 (72.5%) (Supplementary data).
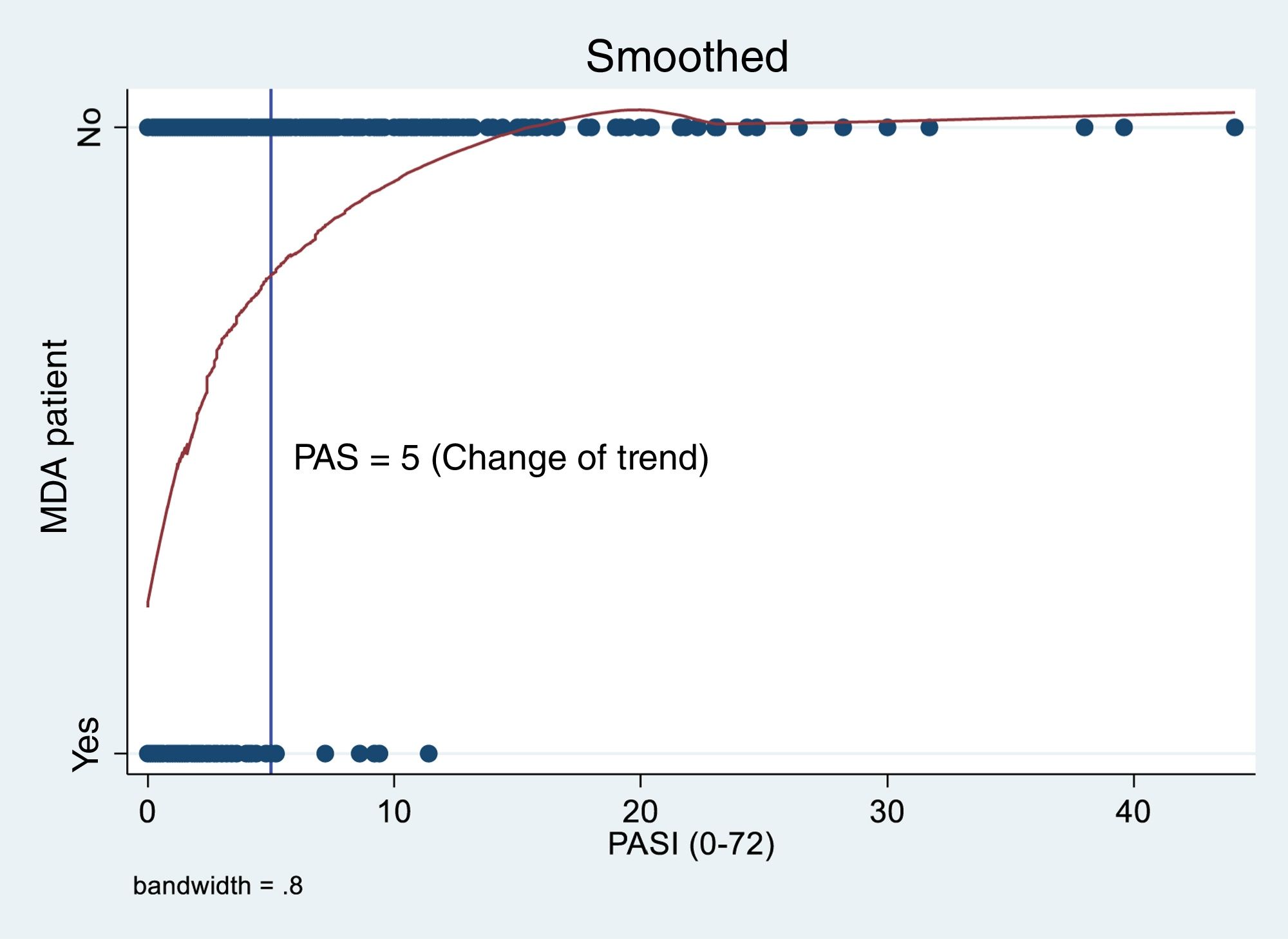
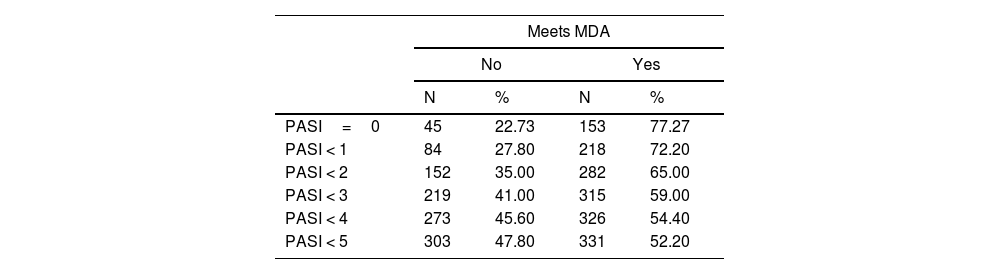
A total of 23% of patients with PASI: 0 (45, 22.3%) did not meet MDA criteria (Table 5). For every unit increase in PASI, the risk of not meeting MDA criteria almost doubled (regardless of treatment); OR, 1.84 (95%CI, 1.61-2.10). In this risk, a change in trend is observed from PASI scores of 5 where increments are not as pronounced (Graph 2).
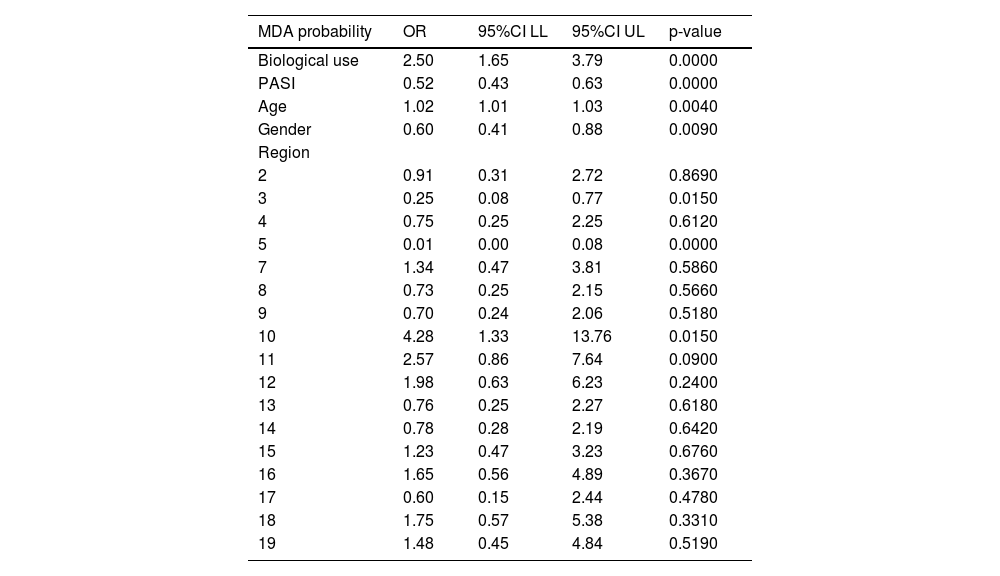
Using a multivariable logistic model, we found that the probability of meeting/not meeting MDA criteria involved the simultaneous use of biological drugs, PASI, age, sex, and geographic region. None of these factors alone—not even the use of biological drugs—explained the differences found (Table 6).
Multivariable probability model for meeting MDA.
| MDA probability | OR | 95%CI LL | 95%CI UL | p-value |
|---|---|---|---|---|
| Biological use | 2.50 | 1.65 | 3.79 | 0.0000 |
| PASI | 0.52 | 0.43 | 0.63 | 0.0000 |
| Age | 1.02 | 1.01 | 1.03 | 0.0040 |
| Gender | 0.60 | 0.41 | 0.88 | 0.0090 |
| Region | ||||
| 2 | 0.91 | 0.31 | 2.72 | 0.8690 |
| 3 | 0.25 | 0.08 | 0.77 | 0.0150 |
| 4 | 0.75 | 0.25 | 2.25 | 0.6120 |
| 5 | 0.01 | 0.00 | 0.08 | 0.0000 |
| 7 | 1.34 | 0.47 | 3.81 | 0.5860 |
| 8 | 0.73 | 0.25 | 2.15 | 0.5660 |
| 9 | 0.70 | 0.24 | 2.06 | 0.5180 |
| 10 | 4.28 | 1.33 | 13.76 | 0.0150 |
| 11 | 2.57 | 0.86 | 7.64 | 0.0900 |
| 12 | 1.98 | 0.63 | 6.23 | 0.2400 |
| 13 | 0.76 | 0.25 | 2.27 | 0.6180 |
| 14 | 0.78 | 0.28 | 2.19 | 0.6420 |
| 15 | 1.23 | 0.47 | 3.23 | 0.6760 |
| 16 | 1.65 | 0.56 | 4.89 | 0.3670 |
| 17 | 0.60 | 0.15 | 2.44 | 0.4780 |
| 18 | 1.75 | 0.57 | 5.38 | 0.3310 |
| 19 | 1.48 | 0.45 | 4.84 | 0.5190 |
The data can be accessed through the viewer: https://aedv.es/grupos-de-trabajo/psoriasis/visualizador-de-casos-de-proyecto-ame/
DiscussionDisease control by applying AME criteria: global and regional perspectivesAlthough the mean values of PASI and BSA show that the patients included had mild disease or were well controlled (4) (Table 2), compliance to MDA is very low: 491 patients (59.2%) do not meet the MDA criteria.
Differences across regions are also clear (Graph 1). Catalonia is the region with the highest MDA adherence, although more than a third of patients (37.1%) do not meet MDA. The fact that a higher percentage of patients on biological therapies was found in this community for our study purposes could favor greater adherence. Access to certain biological drugs is a known factor, as some regions allow the use of any biological drug as a first-line therapy while others require biosimilars of anti-TNF initially or even a specific sequence.8
However, it is not only the greater use of biologicals that justifies this regional difference, as we know that, besides biological use, age, gender, and patients’ PASI scores also influence the outcomes. When we include these factors, regional differences persist, although they tend to decrease (but not completely disappear). As seen in Table 6, the significant differences reported across all factors—simultaneously—imply that all are associated, and the use of biologicals alone cannot fully explain the existing differences.
Adherence to MDA by sex and agePatients’ treatment preferences play an important role in consultations. Age seems to influence therapy choices, both for topical treatments and biologicals, with younger people showing more interest in the potential benefits of these therapies.9 However, we found that older patients are more likely to meet the MDA, which is consistent with the worse quality of life (QoL) scores given by younger individuals,10 though this contrasts with other studies where older patients with skin conditions report worse QoL due to additional health issues.11
In our study, we also found that men are more likely to meet the MDA vs women (Graph 1). Other studies have found a gender distinction favorable to women regarding biological drug prescriptions12; women also seem to experience more itching,13 greater QoL impact,14 and more frequent sleep disturbances.15 These parameters are not typically measured in severity scales—BSA, PGA, PASI—which may underestimate disease severity in certain patient subgroups.
MDA adherence by therapeutic groupUsing more effective drugs could be the most determining factor in achieving MDA. In fact, our study found that the use of biological drugs, as opposed to synthetic drugs or phototherapy, is associated with the highest percentage of MDA adherence. Additionally, studies using the Psoriasis Symptoms and Signs Diary (PSSD)—including erythema, itching, pain, and other symptoms—have shown that although various drugs improve these symptoms, no direct comparisons between drugs exist yet to help choose one over another.16
However, we did not observe any significant differences across different biological drugs, possibly due to selection bias in a non-controlled study where we chose the drug we believed had the best success probability for each patient. This could have led to better results in the first group and worse outcomes in the second, resulting in similar effectiveness rates between the 2.17–20
It is surprising that no patients on phototherapy achieved MDA, and the high percentages of non-adherence were reported among those who were not on therapy (80.4%) or who were on topical therapies alone (88.4%).
Correlation assessment between PASI and MDA adherenceAlthough PASI is the standard measure to assess the severity of Ps, it doesn’t always correlate directly with patient perception7. PASI was included in the study to compare it with MDA adherence.
PASI as a sole severity measure is imprecise, especially in very mild cases which involve small regions of the skin. In fact, in our study, 23% of patients with PASI 0 did not meet MDA criteria. Additionally, PASI doesn’t consider the location of lesions, which we know can significantly impact the patients, such as on nails, folds, genital areas, or palms and soles. Furthermore, PASI is not a linear measure, as 9% to 10% changes in a diseased region of the skin in one location can double the score without any changes being reported in symptoms such as erythema, infiltration, or scaling.21
Therefore, it is understandable that up to 28% of patients with PASI <1 or 35% of patients with PASI <2 from our study do not meet MDA criteria. However, it is striking that a patient with no Ps lesions (PASI 0) and no psoriatic arthritis either does not meet MDA criteria. This suggests other factors—likely psychological—impacting the feeling of illness or being indicative of some limitations in the specificity of the measurement.
The impact of introducing MDAThe most significant subjective signs of the disease are evaluated in the MDA by the patient, who defines how intense their plaques are, how much they flake, how much they itch, how much they bother, and how visible they are. The importance of these values to the patients is seen in the fact that nearly 70% out of the 491 patients from the study who did not meet the MDA included these subjective symptoms as reasons for non-compliance, with itching being the most frequently cited (72.5%) out of the 4 (see Supplementary data).
In fact, the most bothersome symptom for psoriatic patients is itching, which is present in 60% up to 90% of them,22 which is consistent with a multicenter study evaluating psychological factors related to psoriasis in which 69.5% of patients reported itching, and nearly 75% of them experienced it chronically.23
Ps visibility can lead to social rejection and avoidance behaviors, which significantly affect many patients.24 In our study, 372 patients did not meet MDA criteria for this reason, reinforcing the idea that including these subjective symptoms—which are not captured by other indices25,26—is essential to assessing Ps severity through psychological and social factors that negatively affect the patients’ QoL.
MDA is not a sum of PASI, BSA, and DLQI but a global measure of the clinical situation where both the patient and the dermatologist do not see the need for any therapeutic changes or interventions, providing a different qualitative value.
However, despite its utility in patient management,27 its use has not yet become widespread, and few reports specify MDA as a therapeutic outcome measure for psoriatic patients.28
Study limitationsBeing a national study as it is, patient sample is expected to be heterogeneous due to geographic diversity, which can influence the different sensitivities in appreciating the subjective parameters measured by the patient, different perceptions of symptoms based on cultural differences, differences in dermatologist experience (specialized vs general clinic, urban vs rural), different access to more effective drugs,29 etc.
Although patients were not randomized, they were recruited during routine clinical practice over a short period of time (1-2 days), which may have introduced a participation and selection bias by recruiting the most active participants or those who happened to attend the clinic on those days.
ConclusionsAfter applying the MDA nationwide, it seems obvious that adherence is relatively low, with significant differences being reported by sex, age, region, type of therapy, and symptoms reported by patients. However, none of these factors alone explained the differences found, and the use of biological drugs alone could not account for the existing differences.
Evaluating MDA vs PASI provides a better approach to patients by allowing them to participate in measuring the severity of their disease, which could lead to a qualitative improvement in the management of these patients.
The use of MDA in routine clinical practice is easy and convenient, and it can improve the quality of psoriatic patient management by including parameters not considered in other widely used severity scales. Therefore, we encourage dermatologists treating psoriatic patients to use MDA as a measure of disease severity and a therapeutic goal.
AuthorsG. Carretero Hernández: study design, data mining, result interpretation, national coordination of the study, lead author of the manuscript.
Ara Martín, Mariano: data mining, result interpretation, regional coordination of the study in Aragón, lead author of the manuscript.
Armesto Alonso, Susana: data mining, result interpretation, regional coordination of the study in Cantabria, lead author of the manuscript.
Belinchón Romero, Isabel: data mining, result interpretation, regional coordination of the study in the Valencian Community, lead author of the manuscript.
Eiris Salvado, Noemi: data mining, result interpretation, regional coordination of the study in Andalusia, lead author of the manuscript.
Ferrán Farrés, Marta: data mining, result interpretation, regional coordination of the study in Catalonia, lead author of the manuscript.
Galache Osuna, Cristina: data mining, result interpretation, regional coordination of the study in Asturias, lead author of the manuscript.
García Bustínduy, Marta: data mining, result interpretation, regional coordination of the study in the Canary Islands, lead author of the manuscript.
García Latasa de Araníbar, Javier: data mining, result interpretation, regional coordination of the study in Aragón, lead author of the manuscript.
Juliá Manresa, Marc: data mining, result interpretation, regional coordination of the study in the Basque Country, lead author of the manuscript.
Llamas Velasco, Mar: data mining, result interpretation, regional coordination of the study in Madrid, lead author of the manuscript.
López Ferrer, Anna: data mining, result interpretation, regional coordination of the study in Catalonia, lead author of the manuscript.
Roncero Riesco, Mónica: data mining, result interpretation, regional coordination of the study in Castile and León, lead author of the manuscript.
Ruiz Genao, Diana: data mining, result interpretation, regional coordination of the study in Madrid, lead author of the manuscript.
Ruiz-Villaverde, Ricardo: data mining, result interpretation, regional coordination of the study in Andalusia, lead author of the manuscript.
Salgado Boquete, Laura: data mining, result interpretation, regional coordination of the study in Galicia, lead author of the manuscript.
Soria Martínez, Caridad: data mining, result interpretation, regional coordination of the study in Murcia, lead author of the manuscript.
Vilarrasa Rull, Eva: data mining, result interpretation, regional coordination of the study in Cataluña and the Balearic Islands, lead author of the manuscript.
Descalzo, M.A.: data analysis, result interpretation, manuscript preparation.
Conflicts of interestNone declared.
We wish to thank laboratories Almirall and UCB for their financial and human support in the creation, distribution, and collection of the documentary material from collaborating dermatologists, delivery to each regional coordinator, and for data analysis.
This support was not subject to any requirement or condition regarding the study design, data analysis, result acquisition, or drafting of the manuscript.
Abalde Pintos, María Teresa; Alfaro Rubio, Alberto; Aparicio Español, Gloria; Aranegui Arteaga, Beatriz; Arechalde Pérez, Ana; Aróstegui Aguilar, Jorge; Arrue Michelena, Itrziar; Azón Masoliver, Antoni; Bajo del Pozo, Cristina; Ballano Ruiz, Adrián; Baniandrés Rodríguez, Ofelia; Blanco Barios, Susana; Bordel Gómez, María Teresa; Carrascosa Carrillo, José Manuel; Carrizosa Esquivel, Ana María; Castellano González, María; Castro Gutiérrez, Beatriz; Concellón Doñate, María Antonia; Conde Taboada, Alberto; Conejero del Mazo, Raquel; Corral de la Calle, Miriam; Corbalán Vélez, Raúl; Curcó Botargues, Neus; de la Fuente Meira, Sonia; de las Heras, Cristina; de la Torre Gomar, Francisco; del Alcázar Viladomiú, Elena; del Río Gil, Rubén; Delgado Mucienes, Carmen; Delgado Vicente, Sonsoles; Duarte Ferrera, Miguel; Durán Vián, Carlos; Escalonilla García-Patos, Pilar; Fernández Armenteros, José Manuel; Fernández Díaz, María Luisa; Fernández Sánchez, Cristina; Fuentelsaz del Barrio, María Victoria; Fortuño Ruíz, Yolanda; Frías Iniesta, José; Galán Gutiérrez, Manuel; Gallardo Hernández, Fernando; García Arpa, Mónica; García Donoso, Carmen; García Fernández de Villalta, María José; García Font, Mer edes; García Gil, Miguel; García Martínez, Esther; García Sánchez, María; García Souto, Fernando; Garrido Colmenero, Cristina; Gil Faure, Inma; Gil Mateo, María del Pino; Godoy Díaz, Daniel; Godoy Gijón, Elena; Gómez Avivar, Pilar; Gómez Centeno, Pilar; Gómez de Castro, Celia; Gómez Díez, Santiago; Gómez Vila, Borja; González Cantero, Álvaro; González Quesada, Alicia; González Villanueva, Iris; Gracia Cazaña, Tamara; Hergueta Sánchez, Julia Paloma; Hernández Hernández, Zaida; Hernández Montoya, Carlos; Hospital Gil, Mercedes; Lacalle Calderón, Marina; Laso Dosal, Francisco Javier; Lezcano Biosca, Victoria; López Ávila, Angel; López Castillo, Daniel; López-Escobar García-Prendes, María; López Estebaranz, José Luis; Lorda Espés, Marta; Luján Rodríguez, Dunia; Mahiques Santos, Laura; Marcellán Fernández, María; Márquez Henríquez, Juan; Marqués Martín, Laura; Marrón Moya, Servando Eugenio; Martín Alcalde, Javier; Martín González, Isabel; Martín Sáez, Esther; Martínez de Espronceda Esquerro, Iñigo; Martínez de Salinas Quintana, Ana; Mataix Martínez, Javier; Matas Nadal, Clara; Mateu Puchades, Almudena; Medina Montalvo, Susana; Menéndez García-Estrada, Ana; Miralles Botella, Julia; Mitxelena Eceiza, Yosune; Mollet Sánchez, Jordi; Monte Serrano, Juan; Montes Torres, Andrea; Morales Callaghan, Ana; Morales Larios, Elisa; Morales Moya, Ana Luisa; Moreno Suárez, Fátima; Muñoz Santos, Carlos; No Pérez, Nuria; Notario Rosa, Jaume; Ormaetxea Pérez, Nerea; Palacios García, Laura; Pardo Sánchez, José; Pérez Barrio, Silvia; Pérez Caballero, José Antonio; Pérez Gil, Amalia; Pérez Suárez, Beatriz; Pestana Eliche, María; Pousa Martínez, María; Poveda Montoyo, Inés; Prieto Torres, Lucía; Puebla Tornero, Laura, Puig Sanz, Lluis; Pujol Moncusí, Josep; Ramírez Andreo, Antonio; Ramírez Concha, José María; Ramírez Santos, Aquilina; Reguero del Cura, Leandra; Requena López, Sheila; Ribera Pibernat, Miquel; Riera Monroig, Josep; Río García, Irene; Rivera Díaz, Raquel; Rivera Fuentes, Ignacio; Rocamora Durán, Vicenç; Rodríguez Blanco, Sabela; Rodríguez Freire, Lourdes; Rodríguez García, Fernando; Rodríguez Martín, Marina; Rodríguez Nevado, Isabel; Romero Aguilera, Guillermo; Romero Mate, Alberto; Romero Sillero, Estrella; Ruiz Carrascosa, José Carlos; Ruiz Martínez, Javier; Sagristá García; Marc; Saínz Gaspar, Laura; Salas Martínez, Ana; Salleras Redonet, Montserrat; Sánchez Caminero, Prado; Sánchez Largo, Elena; Sánchez Pérez, Javier; Sánchez Salas, María Pilar; Santos-Juanes Jiménez, Jorge; Sahuquillo Torralba, Antonio; Segurado Rodríguez, Agustina; Sidró Sartos, Miriam; Solanas Treviño, Ruth; Suárez Hernández, José; Taberner Ferrer, Rosa; Úbeda Clemente, María Isabel; Urigoitia Ugalde, Peru; Vázquez López, Francisco; Velázquez Tarjuelo, Diana; Vidal Sarro, David; Vilar Alejo, Jaime; Villegas Romero, Isabel, and Yanguas Barona, Ignacio.