Malignant syphilis is a rare manifestation in secondary syphilis and one that is associated in most cases with immunosuppression.1–4
We report the case of a 26-year-old man with a possible adverse reaction to penicillin. He consulted because of progressive lesions on the trunk, genitals, and lower limbs in the form of excoriated nonfollicular papules that were slightly painful. Staphylococcus aureus was isolated from the exudate from these lesions, so the patient was treated with topical mupirocin and later with oral erythromycin (500mg/day for 14 days). Serology was positive for syphilis (positive rapid plasma reagin; Treponema pallidum hemagglutination assay [TPHA], 1/80), which was associated with a genital ulcer treated with oral erythromycin in primary care 1 year before the patient came to our clinic.
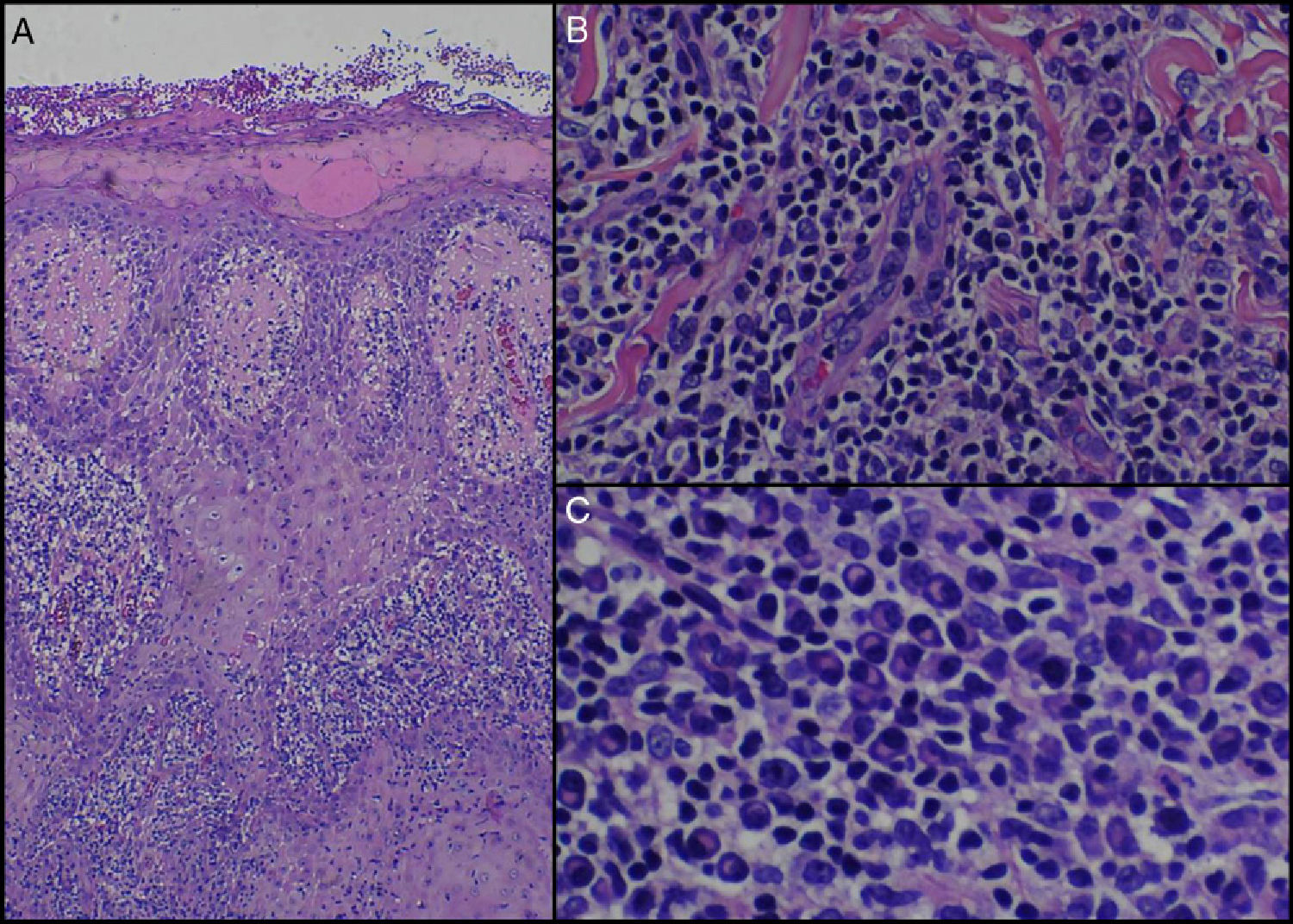
A month after starting the treatment that we prescribed, the patient reported acute worsening of the lesions. He presented with numerous intensely painful round plaques with raised borders and collarette scaling. Most of these plaques had very adherent necrotic eschars and central squamous crusts. The plaques were between 2 and 5cm in diameter and were located on the scalp, trunk, genitals, and lower limbs (Fig. 1). For the last month the patient had also had evening fever and poor general condition.
Clinical differential diagnosis was made with cutaneous T-cell lymphoma.
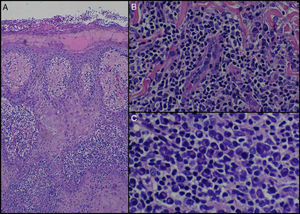
A biopsy of one of the lesions revealed an acanthotic epidermis with areas of pseudoepitheliomatous hyperplasia covered by a squamous crust (Fig. 2A). In the dermis there was an intense perivascular lymphohistiocytic and plasma cell infiltrate with endarteritis and associated vascular occlusion (Fig. 2B and C).
Chest radiograph revealed no pleuropulmonary abnormalities. The complete blood count revealed a slightly elevated white blood cell count without left shift or lymphocytosis; serology for human immunodeficiency virus (HIV) and hepatotropic viruses was repeatedly negative. Ocular, neurological, and cardiac involvement and other cell-mediated immune disorders were ruled out. Serology for syphilis was strongly positive (VDRL test, 1/128; TPHA, 1/20 480), confirming the diagnosis of malignant syphilis in an HIV-negative patient. A sample of cerebrospinal fluid revealed no abnormal findings and allergy to β-lactams was ruled out by a skin prick test. We therefore started treatment with intramuscular injection of 7.2 million units of penicillin G benzathine in 3 weekly doses. Clinical response was rapid and without complications, with involution of all the lesions after 3 weeks.
Follow-up was performed at 3, 6, and 12 months. HIV serology was repeatedly negative, with stable titers at least 4 times lower (VDRL test, 1/32) than at the start of treatment. We plan to continue with follow-up visits, including serology, every 6 months for a period of 2 years.
Malignant syphilis is a rare form of secondary syphilis. Most of the cases reported in the last 20 years have been described in HIV-infected patients.1–4 This finding suggests a relationship between qualitative alterations in immunity and a more virulent course of the infection. However, it is paradoxical that most of these patients have a CD4 lymphocyte count above 200.1–4 The relationship between HIV and syphilis is regulated by complex immunological mechanisms that are not well defined at present.2.3 Other cases reported in HIV-negative patients had some immunological impairment due to alcoholism,5,6 hepatitis,7 or reinfection.8
The 2010 guidelines of the Centers for Disease Control and Prevention (CDC)9 make no specific recommendation for malignant syphilis, with or without HIV seropositivity. The treatment for late latent syphilis is the most frequently used.
For secondary syphilis in patients allergic to penicillin the CDC guidelines recommend oral treatment with doxycycline or tetracycline for at least 2 weeks. As in our case, the literature indicates a poor response to these drugs in malignant syphilis and proposes intravenous ceftriaxone as an alternative.2.3 Treatment with cephalosporins is inadvisable without first ruling out adverse cross-reactivity with β-lactams,9 so we consider it necessary to test for this allergy before treatment.
The latest data on the incidence of syphilis in Spain published by the Spanish Ministry of Health10 show a great increase in cases in recent years, probably related to changes in sexual habits. Although notifiable diseases are not always reported, the number of reports of syphilis in Spain rose from 700 in 1998 to over 2500 in 2008 and 2009.10
These data suggest that malignant syphilis is an atypical form of a sexually transmitted infection that is becoming increasingly common in Spain. The increased incidence may be associated with unusual clinical manifestations that are difficult to diagnose.
Malignant syphilis should not be considered an opportunistic infection or one exclusive to HIV-positive patients6 because it can occasionally occur in immunocompetent patients.
Please cite this article as. García-Martínez FJ, et al. Sífilis maligna en un paciente inmunocompetente. Actas Dermosifiliogr.2012;103:437-52.