Reconstruction of large surgical defects on the cheek can be challenging for dermatologic surgeons. We describe using a modified rhomboid flap and Burow's advancement flap to close a surgical defect resulting from the excision of a basal cell carcinoma measuring 10cm×10cm in the buccomandibular area of the cheek.
La reconstrucción de grandes defectos quirúrgicos de mejilla puede constituir un gran desafío para el cirujano dermatólogo. Se describe una paciente con un carcinoma basocelular de 10cm de largo por 10cm de ancho que ocupaba la región bucomandibular de la mejilla, en la que la reconstrucción del defecto resultante de la cirugía se cerró con una combinación de un colgajo romboidal modificado con un injerto de Burow.
Basal cell carcinoma is a common malignant tumor that develops above all on areas exposed to sunlight, with the cheek being a very frequent site.1
After the tumor is resected from the cheek, defect closure may require complex reconstruction techniques. We report a case in which, after debating the different closure options, a modified rhomboid flap was chosen in combination with a Burow advancement flap, an option we consider useful and innovative for reconstruction of large defects in this area.
Case historyA 58-year-old woman had a basal cell carcinoma measuring 10cm×10cm in the buccal-mandibular area of the left cheek, with onset of the lesion several years earlier.
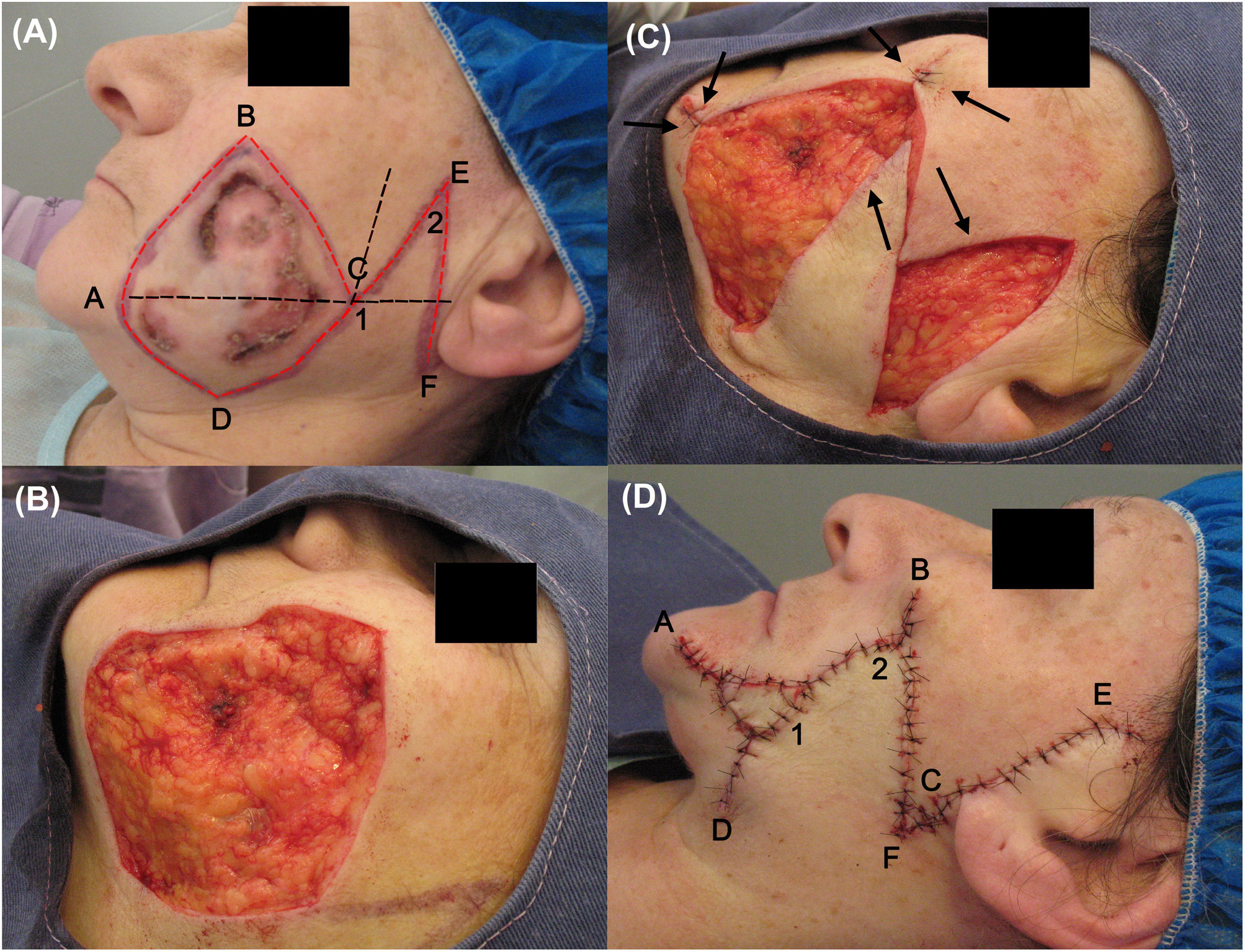
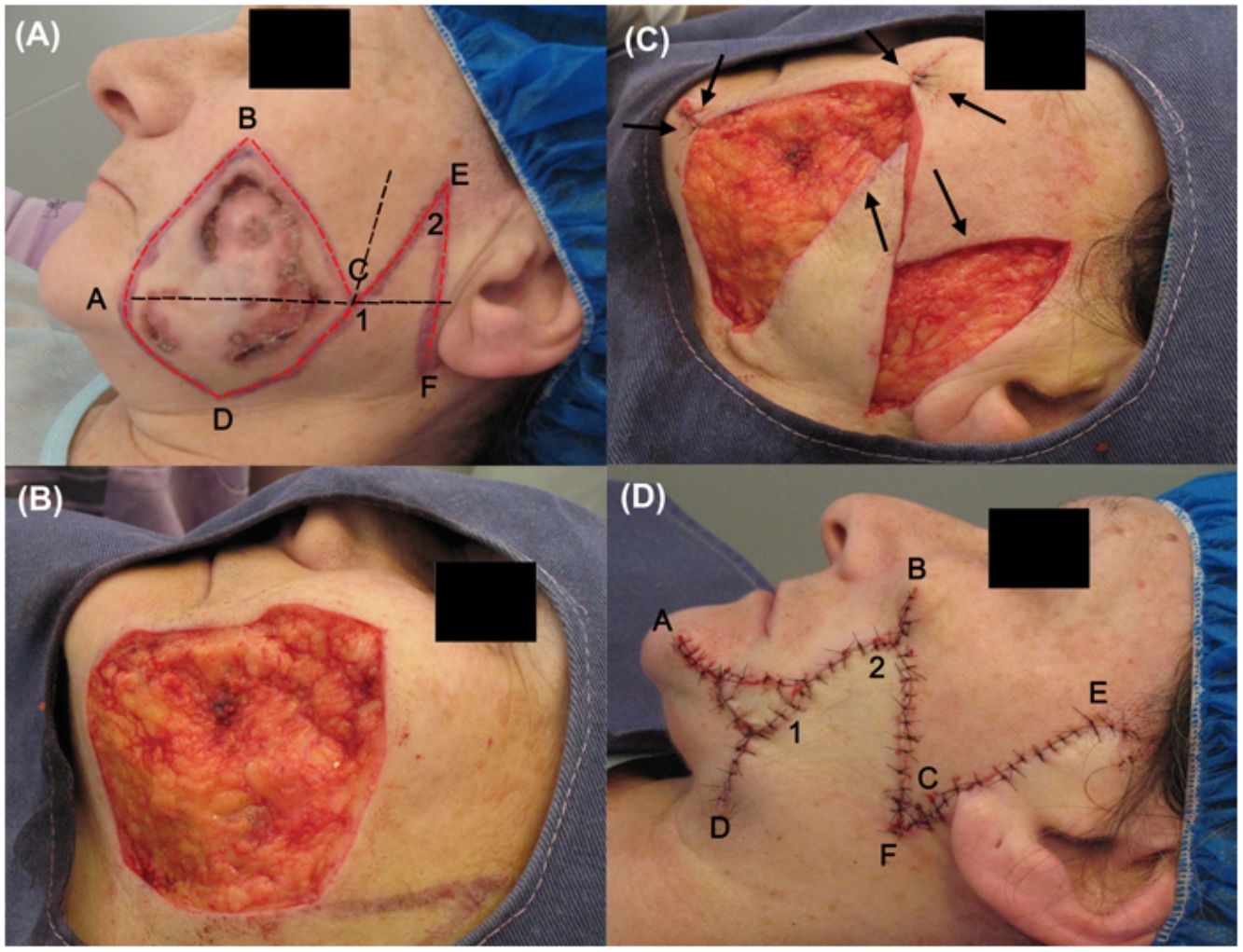
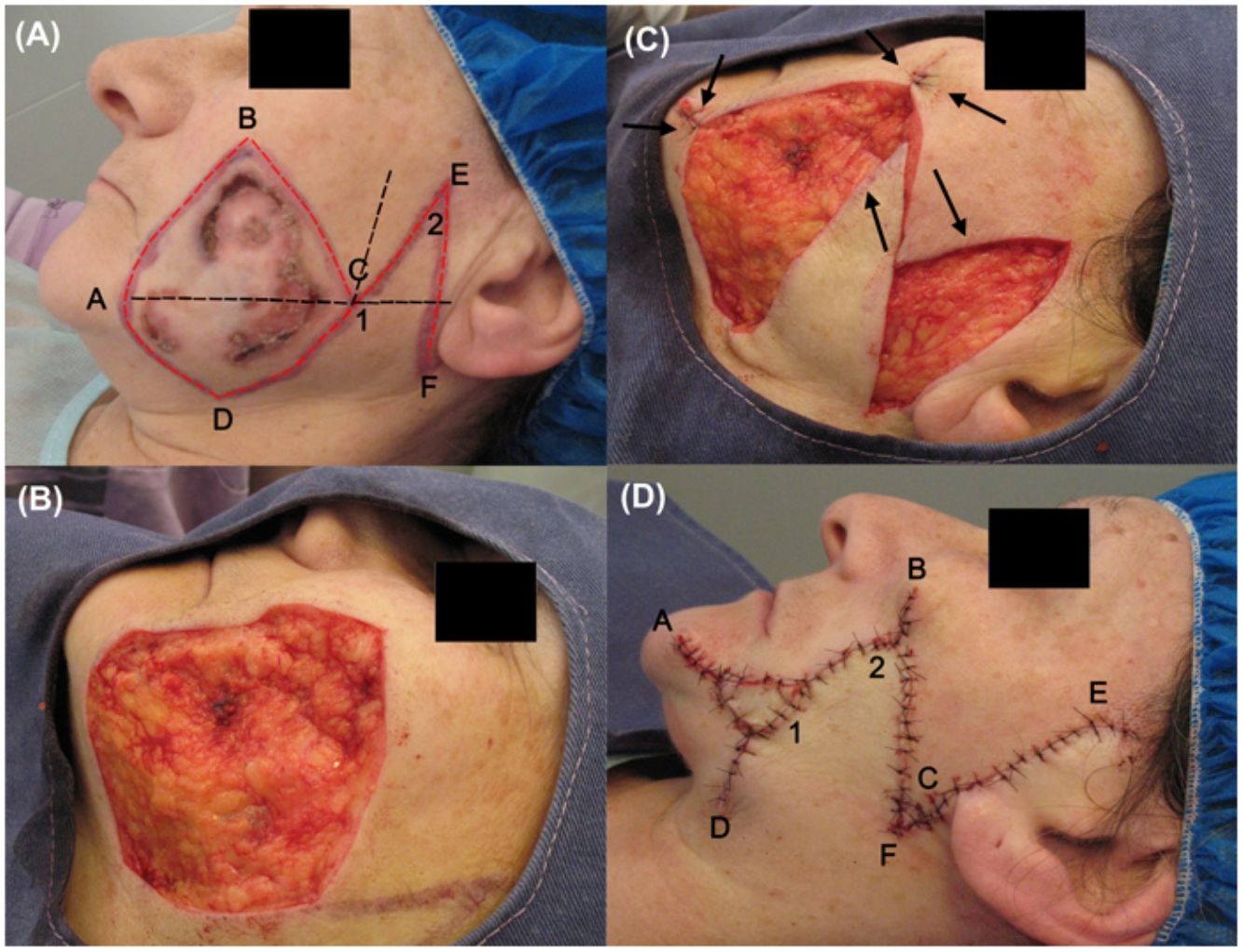
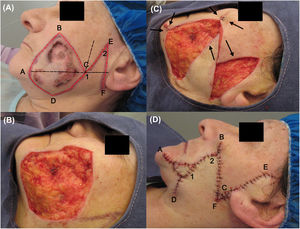
The tumor was excised according to the following procedure. First, asepsis and antisepsis were performed on the area, to which tumescent anesthesia was then applied (composed of 20mL saline solution, 7.5mL bupivacaine 0.5%, 5mL lidocaine 2%, and 0.3mL adrenalin). Subsequently, the option of a rhomboid flap was chosen. For this, a rhomboid outline was traced, formed of equal-length sides and 2 angles of 30° and 150°, in which a line (A-C) was marked dividing the shape into 2 equilateral triangles. Two imaginary lines were extended from this shape, one from the A-C line continuing a few centimeters in the posterior direction and the other from the D-C line upwards. A line, of the same length as the D-C side, bisecting the angle formed by these 2 imaginary extensions was marked. Finally, a line perpendicular to the A-C line was drawn, denoted E-F (Fig. 1A).
Photographs during surgery. (A) Flap incision lines (in red) and imaginary ones (in black). (B) Defect after tumor excision. (C) The flap could only close the posterior part of the defect (cheek). (D) Immediate postoperative period, in which a Burow advancement flap was placed on the anterior area (mandibular).
Then, taking into account the oncological margins required (1cm) and the rhomboid form of the defect, tumor excision was performed in accordance with these 2 conditions, followed by suitable hemostasis (Fig. 1B).
To obtain the flap, incisions were made along the lines traced in red to ensure tension-free closure of the defect and the flap was completely dissected at the level of adipose tissue (Fig. 1C).
For reconstruction of the defect, the flap managed to cover almost the entire wound in the cheek, but the flap was unable to cover the entire area of the mandibular sector, which was closed using a Burow advancement flap. The donor area was obtained from surplus skin that was withdrawn due to the flap rotation (angle D). For flap placement, the excess defect was measured, the excess adipose tissue from the graft was removed, and the flap was placed and adjusted to this area, holding it in place with suture around the perimeter. The subcutaneous tissue and skin were sutured with discontinuous sutures with simple stitches, with absorbable 5-0 thread (polyglactin 910) and nonabsorbable thread (nylon 5-0), respectively (Fig. 1D).
Histological study of the surgical piece indicated disease-free margins.
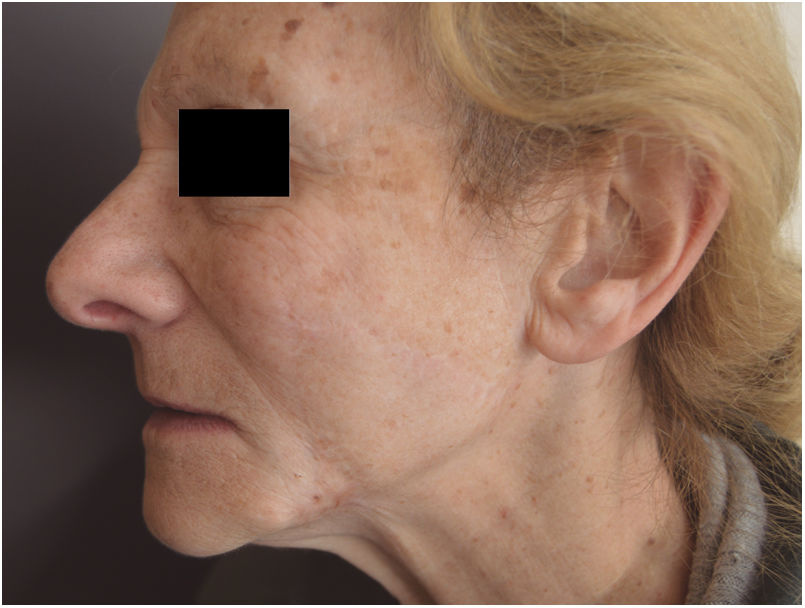
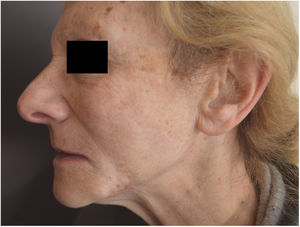
There were no complications during surgery or the postoperative period. After 5 years of follow-up, excellent anatomofunctional and esthetic outcomes were achieved (Fig. 2).
DiscussionReconstruction of defects in the buccal-mandibular region is complex given its relationship with the mouth and nose, areas where pulling can generate tractions that lead to functional and esthetic complications.2
There are several options for reconstruction of defects in this area. The one chosen will depend on factors such as the size of the defect and whether redundant skin is available.3
In the case described here, several options were considered. Given the amount of redundant skin in the preauricular area and neck, this area was considered most valid as the donor area for a flap. One alternative could have been a rotation and advancement flap, for which an oval-shaped flap would be designed, and the flap would be formed by tracing a line from the upper part backwards, around the area in front of the ear, downwards in the preauricular fold, and then around the ear lobe to then extend the line upwards, such that on rotating upwards and forwards, it would cover the wound.4,5 However, despite the advantages, given that this type of flap usually requires extensive tissue movement, it was not the chosen option.2,4
Another alternative would have been an approach by primary closure from the angles with a skin graft, or closure by second intention for areas that could not undergo primary closure. Neither of these approaches were considered a suitable option given that worse cosmetic outcomes would be obtained.2
In this case, we opted for a modified rhomboid transposition flap combined with Burow advancement graft. Although this type of flap has some disadvantages, such as the fact that the defect has to have a rhomboid shape and excess healthy tissue is sacrificed to obtain optimal esthetic results, this approach was used given the several advantages that it offered. One of these is that it makes use of the laxity of an adjacent area to allow acceptable coverage, as well as redistributing and redirecting closure tensions thus avoiding deforming the free margins and orifices. Also, in comparison with rotation flap and advancement flaps, these flaps are usually smaller, thus enabling limited detachment.
The combined technique also has several benefits. For example, in the present case, it can be seen that although the primary defect was limited to the cheek, with the oncological margins and the rhomboid form of the defect, the final defect covered 2 esthetic units (cheek and chin), so the use of 2 reconstruction techniques to repair 2 esthetic units separately (cheek flap and flap in the mandibular area) constitutes a very good option for this type of reconstructive challenge. The reconstructive alternative also allows for a suitable cosmetic outcome, operative ease, low rates of complications, durability, and relatively short healing times.
Conflict of interestsThe authors declare they have no conflict of interest.