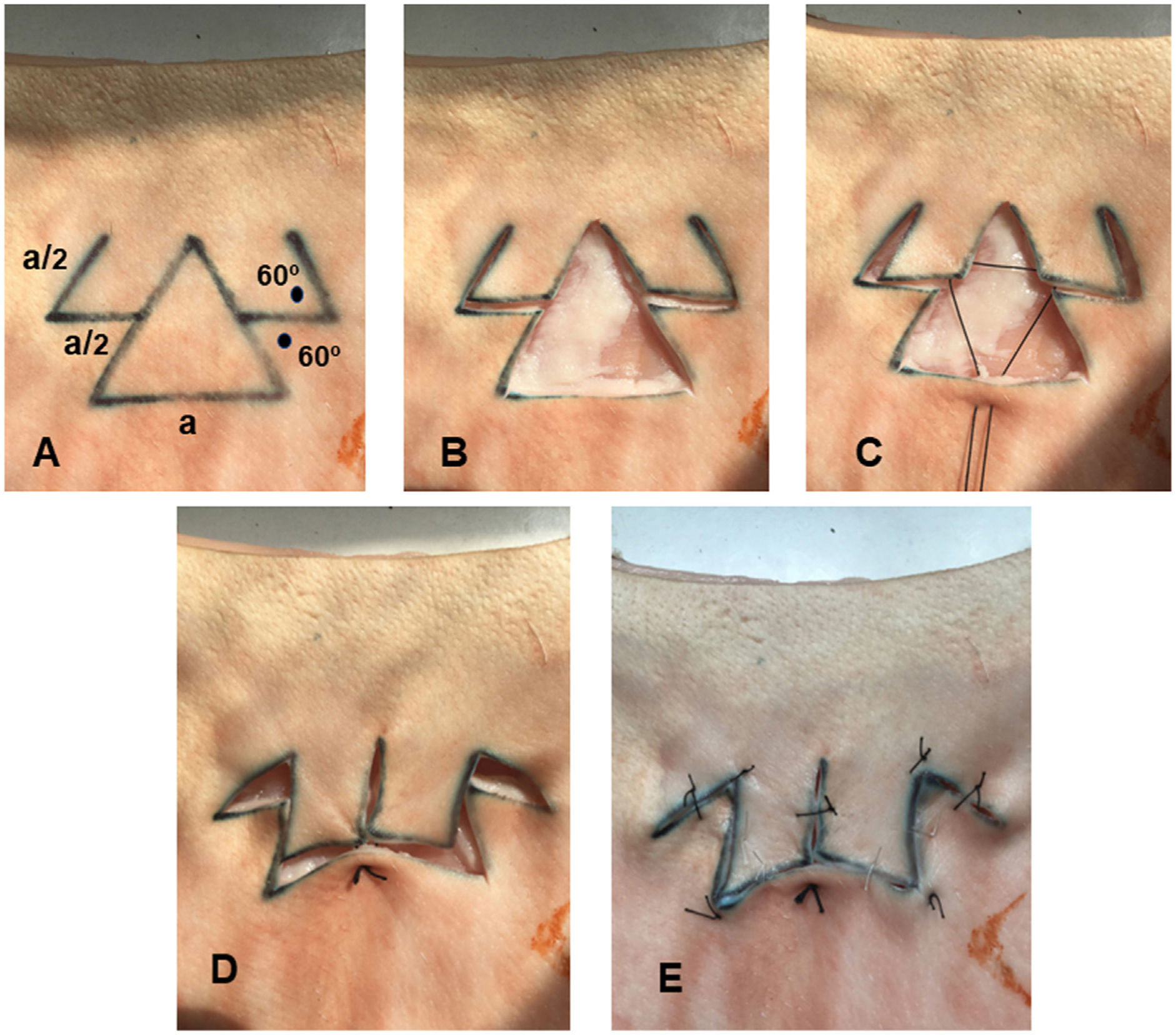
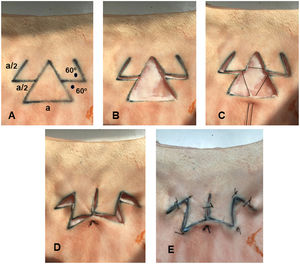
We recently designed the spider crab flap for reconstruction of triangular surgical defects.1 The flap is a double transposition flap that behaves much as a double Z-plasty at each side of the triangle, enabling central closure with a final W-plasty (Fig. 1).
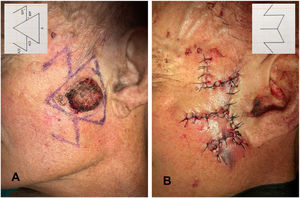
Design of the spider crab flap on pig skin. A, The 2 lateral transposition flaps, which represent the arms of the crab, are traced from the central point of the sides of the triangle. These lateral flaps measure half the length (a/2) of the base of the triangle (a), with an angle of 60° (black spots). B, Excision of the triangle representing the surgical defect and dissection of both flaps. C, Central point of suture, which starts at the base of the triangular defect and passes through the internal vertices of the lateral flaps. D, Closure of the defect with the single central stitch. E, Outcome after complete suture of the flap.
With the aim of setting parameters to enable objective evaluation of the viability of this new flap, we measured the tension generated at the borders of the flap using an experimental model based on pig skin and a digital tensiometer. In a previous study,2 we had evaluated the tension generated at the borders of classic rotation, advancement, and transposition flaps and objectively compared tension values for this new flap with those of the classic flaps.
In their study, Brinca et al.3 reported measuring blood flow in the classic flaps using in vivo laser speckle contrast imaging. This direct measurement of perfusion could complement measurement of tension at the borders of the flap, since both produce objective values that are directly related to the viability of the flap.4,5 Therefore, we decided to measure perfusion of the new spider crab flap in vivo using the same laser-based system as in the previous study in order to draw an objective comparison with the vascularization parameters found for the classic flaps.
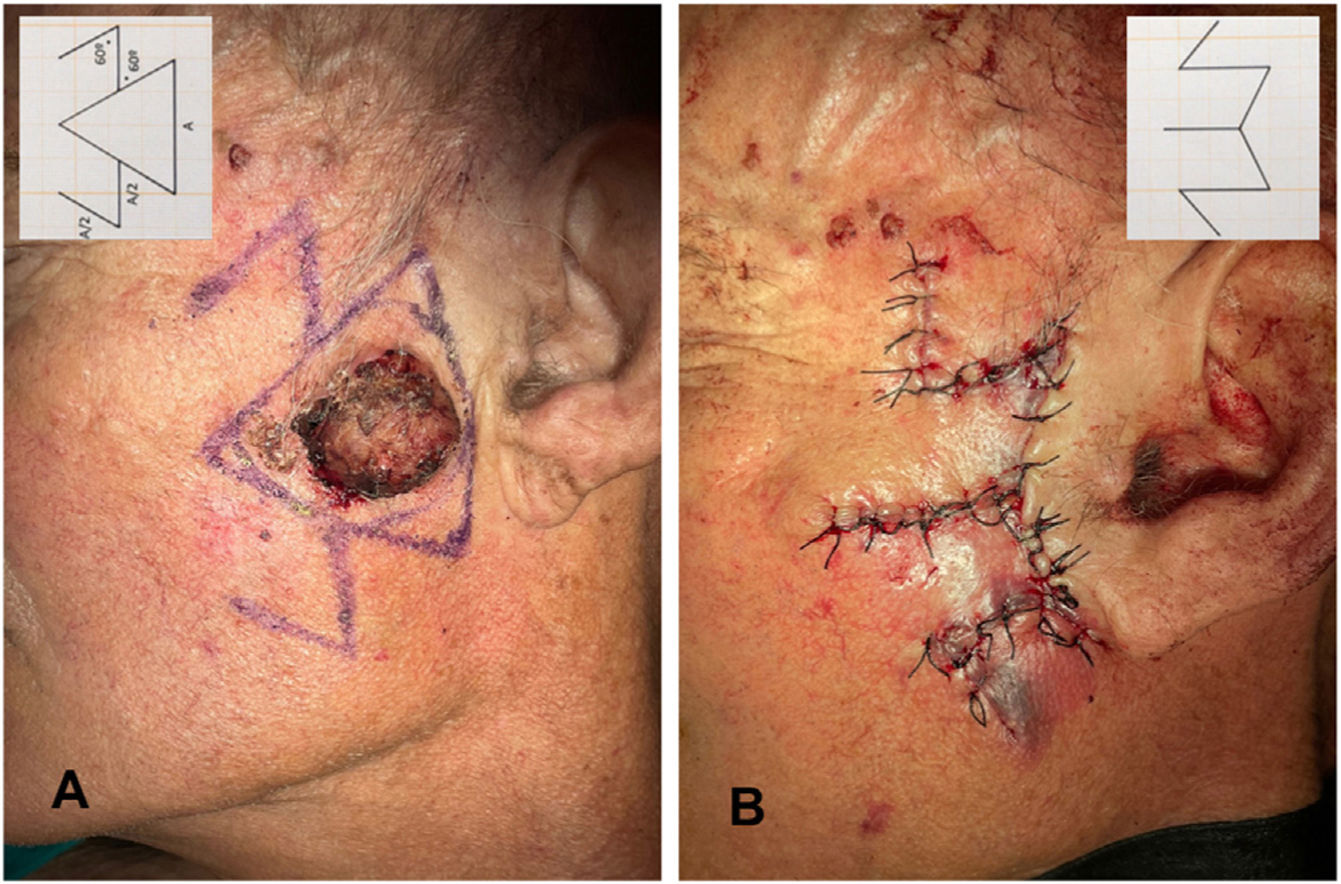
A 67-year-old man underwent surgery for wide excision of a squamous cell carcinoma on the cheek. Excision was performed following a triangular design, and the cheek was reconstructed using a spider crab flap (Fig. 2).
Perfusion was measured using laser speckle contrast imaging (PeriCam PSI NR) and PIM Soft (version 1.5.4.8078).
Mean perfusion values for the spider crab flap were measured at 3 time points: baseline (i.e., before the procedure); with the flap dissected; and with the flap sutured. Measurements were taken at 4 points along the flap: base, proximal third, distal third, and vertex.
Perfusion data for the spider crab flap show that cutaneous vascular conductance at baseline was 3.012 arbitrary perfusion units (APU)/mmHg. This fell to 2.347 APU/mmHg when the flap was dissected and further to 2.321 APU/mmHg when the flap was sutured (Table 1 Supplementary material). The mean perfusion decreased by 23.7% when the spider flap was dissected and by 27.8% when it was sutured.
When we measured perfusion at the base of the flap, the medial third, the distal third, and the vertex, we found that on dissecting and suturing the flap, perfusion decreased as we moved away from the base. Perfusion pressure at the vertex of the flap after suturing reached 40% of the perfusion at the base.
When we compared the findings for blood flow in the spider crab flap in this study with those recorded previously with classic rotation, advancement, and transposition flaps,3 we saw that the reduction in mean perfusion of the flap with respect to baseline perfusion reached 58.34% in the case of the rotation flap, 48.74% in the advancement flap, and 57.85% in the transposition flap. However, in the spider crab flap, the mean decrease in perfusion proved to be only 22.93%.
Furthermore, after combining these data with those from previous studies1,2 on maximum tension at the border of the sutured flaps, we found the lowest tension values in the rotation flap (4.27N), followed by the spider crab flap (4.42N), with the highest values recorded for the advancement flap (6.05N). (Table 2 Supplementary material).
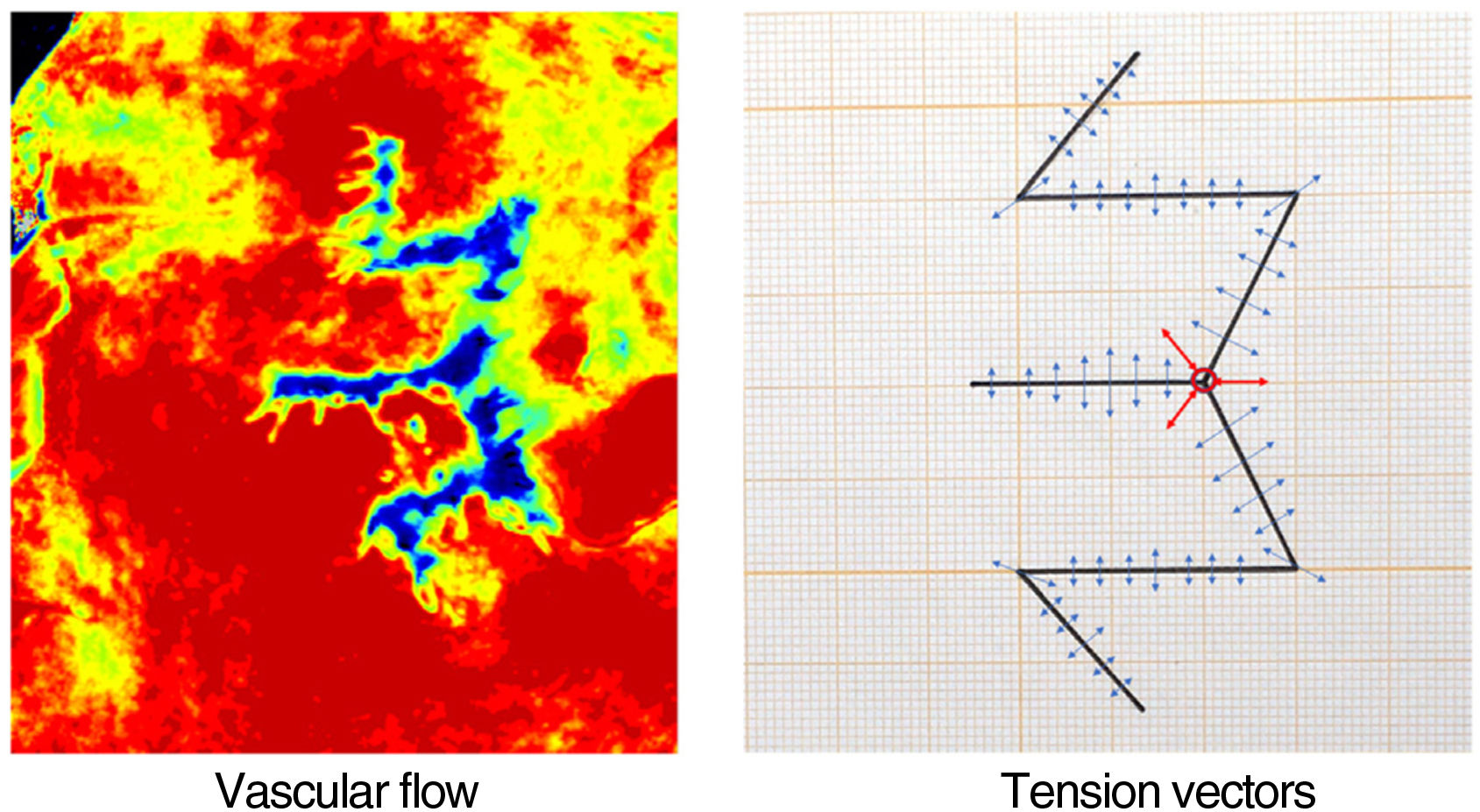
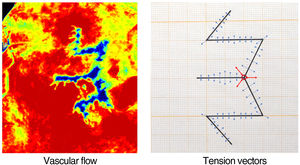
It is interesting to note that the perfusion image acquired with in vivo laser speckle contrast imaging correlated exactly with the ex vivo tension vector plan of the borders of the sutured spider crab flap (Fig. 3). This supports the hypothesis that both parameters complement each other in the evaluation of the viability of the new flaps.
Direct correlation between the perfusion image and the tension vectors. The image on the left represents blood flow. Red indicates maximum perfusion. As blood flow diminishes, the color scale gradually degrades until it reaches blue-black, which indicates minimum perfusion. The image on the right shows the tension vectors at each suture point, such that the length of the arrows represents the magnitude of the tensions. The central vector highlighted with 3 red arrows is the point of maximum tension and, in the flow image on the left, corresponds exactly to the central area of minimum vascular flow shown in blue-black. The silhouette of the W-plasty scar, where the tensions are focused, corresponds exactly to the image of the blue flows.
In conclusion, when we combined the results for perfusion in this reconstruction based on a spider crab flap with our previous data on blood flow and tension in classic flaps (rotation, advancement, and transposition), we observed that in terms of decreased perfusion values when suturing, the lowest values were found for the spider crab flap. In terms of tension at the borders, the second lowest values were recorded for the spider crab flap. These parameters show the excellent viability of the spider crab flap, making it a favorable option for surgical reconstruction, even in areas with high baseline anatomical tension or poor blood flow.
Our study attempted to provide objective parameters for evaluation of the viability of new flaps. However, further cases must be assessed to determine the various parameters that can affect flap perfusion, such as the anatomical area, the age of the patient, and the experience of the surgeon.
FundingThe authors declare that no funding was received for the present study.
Conflicts of InterestThe authors declare that they have no conflicts of interest.