We describe 28 patients who experienced effluvium with previously unreported features shortly after hair transplant surgery. Notable features were as follows: (a) a linear morphology; (b) immediate onset (1–3 days); (c) association with dense-pack grafting in areas of receding hairline at the temples (Mickey Mouse pattern); (d) a progressive increase in the diameter of the hair loss line (wave-like pattern); (e) in some cases, subsequent concentric linear effluvium on the crown (donut pattern); and (f) other forms of previously unreported immediate-onset effluvium. The linear morphology could be the result of dense packing, which can cause perilesional hypoxia and loss of miniaturized hairs around the recipient area. Since linear hair loss can cause patient concern about graft failure, we recommend taking images of transplanted and nontransplanted areas immediately after surgery and warning patients in advance about these transient effects, which are fully reversed in 3 months.
Describimos 28 pacientes que desarrollaron una forma de efluvio postrasplante capilar con características no descritas en la literatura: a) morfología lineal; b) aparición inmediata (uno a tres días); c) asociación con «dense packing» en entradas («signo de Mickey Mouse»); d) progresión del diámetro de la línea (patrón «wave-like»); e) posible adición posterior de efluvio lineal concéntrico a vértex («signo del donut»), y f) además de otros efluvios tampoco publicados por su inmediatez de aparición. La morfología lineal podría ser el resultado de la alta densidad colocada en nuestros pacientes, provocando hipoxia perilesional y efluvio de las unidades foliculares miniaturizadas que rodean la zona receptora. Debido a que la línea alopécica provoca inseguridad a los pacientes sobre una posible no colocación de injertos, recomendamos iconografía postoperatoria inmediata demostrando unión de áreas trasplantada y no trasplantada, así como la explicación previa al paciente de este fenómeno transitorio y completamente reversible en tres meses.
Hair transplantation (HT) is a surgical technique that can increase hair density in different forms of alopecia, redistributing follicular units from the donor area (occipital-temporal hair or body hair) to the recipient area.1 Many different types of effluvium have been reported after HT. The process usually presents from week 2 (effluvium in the transplanted hair2) up until 2 months after HT (effluvium in the donor areas3,4 and recipient areas5). The underlying mechanism could by multifactorial and associated with stress, surgical trauma, and/or ischemia arising from use of epinephrine for tumescent anesthesia. Dense-packing HT (50–70 follicular units [FU]/cm2) could act in the recipient area as a similar stressor to overexploitation of the donor area. Ever since our center has practiced HT in the front third of the scalp, we have observed the appearance of new types of effluvium with a linear morphology around transplanted areas (‘Mickey Mouse’ pattern at the temples and ‘donut’ pattern on the crown). Onset occurs earlier than in effluvia described in the literature (from the first day after HT) and the lesions form a notable area of transient and reversible alopecia between the recipient area and nontransplanted hair.
The main objective of this study was to describe the characteristics of patients who developed linear effluvium of immediate onset after HT. As a secondary objective, other nonlinear patterns of effluvium were analyzed in parallel in cases in which surgery was not limited to the area of the temples.
Patients and methodsThis was a retrospective, observational, descriptive study of a series of patients who developed linear effluvium immediately after HT (from the first to ninth day post-intervention), operated between January 2020 and March 2022, in the Trichology and Hair Transplant Unit of the dermatology department of the Hospital Juaneda, Palma de Mallorca, Spain.
The following baseline characteristics were recorded for each patient: sex, age, type of alopecia, surgical extraction technique (follicular unit extraction [FUE] or plucking), and number of follicular units transplanted. Patients attended 2 visits with standard photographs during the immediate postoperative period: at 1–3 days and at 7–9 days. At each visit, the following characteristics were recorded: presence or not of linear effluvium at each transplant site (temple, upper forehead, and crown), diameter of resulting alopecia (mm), and coloration (erythema or pale).
Other concurrent effluvia with other characteristics were noted (nonlinear pattern, different site) if they also appeared during the first 9 days after HT.
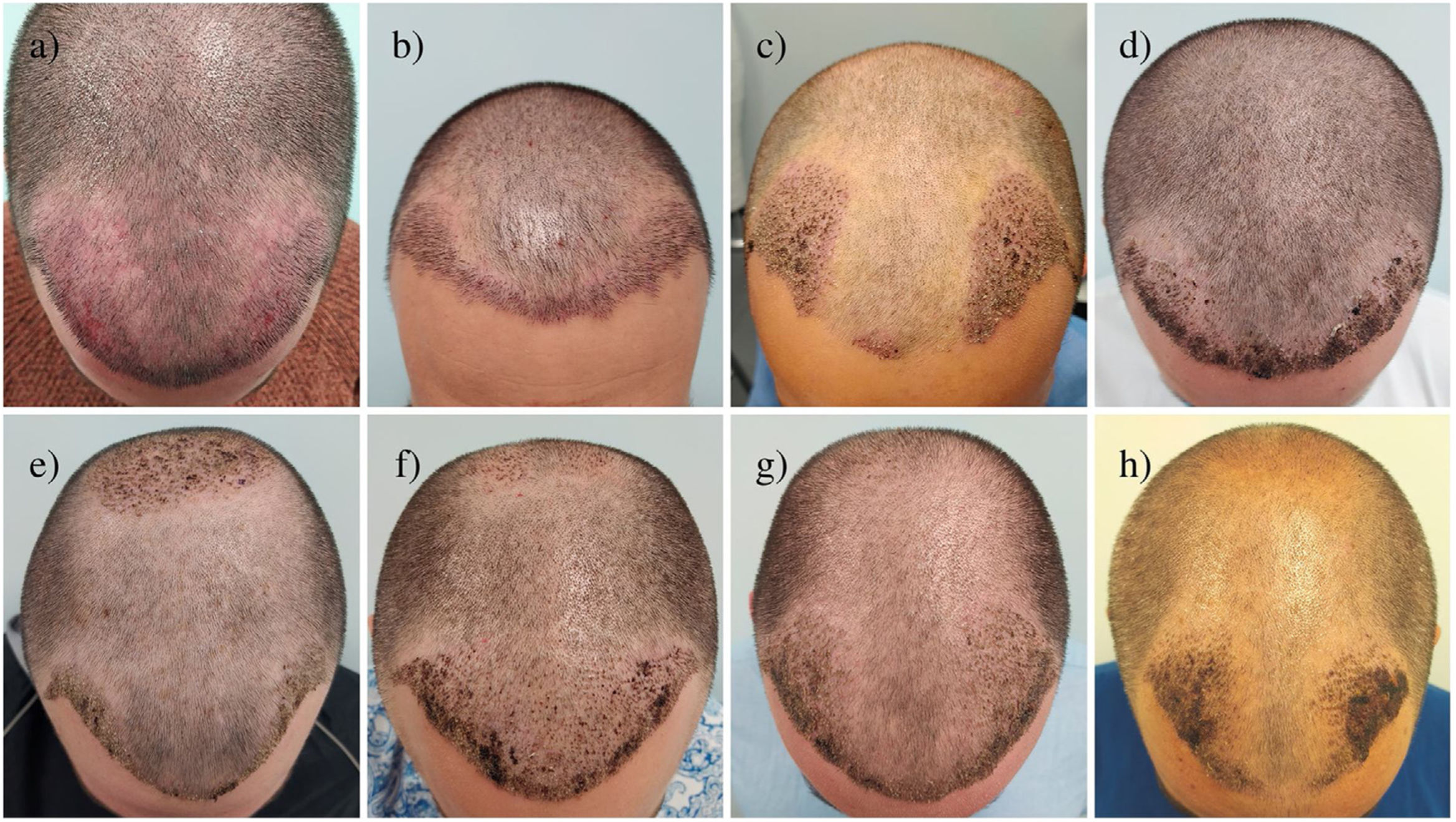
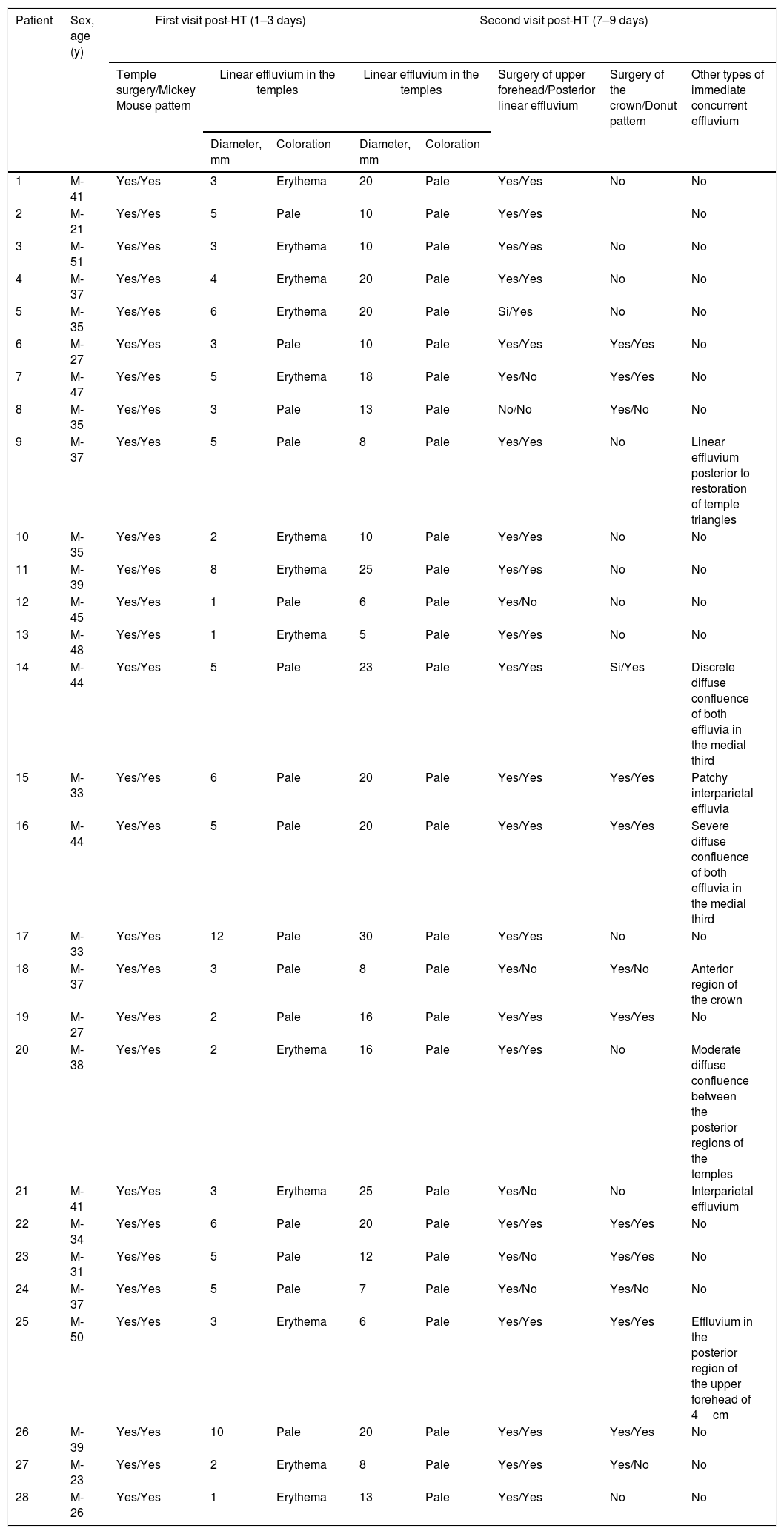
ResultsOf the 274 patients who underwent HT in the study period (270 by FUE and 4 by hair plucking), 261 were men and, of these, 247 were treated for androgenetic alopecia. Of the latter group, 28 developed linear effluvium immediately after HT (Table 1). The median age was 38 years (range, 21–51 years). The median number of FUs transplanted was 2650 (range, 2238–3470) in the front third and 1122 (range, 750–1440) in the crown. All cases had the following characteristics in common: FUE technique and restoration of receding hairline at the temples by dense-pack grafting. In all patients, posterior linear effluvium was noted at the temples (Mickey Mouse pattern) in the control visit between 1 and 3 days after HT (Fig. 1). In this first follow-up visit, we did not observe any other type of accompanying effluvium. At the second visit, 2 additional types of linear effluvia were observed: a concentric linear effluvium in 10 of the 14 patients with restoration of hair loss at the crown and posterior linear effluvium in 21 of the 27 patients with restoration of hair loss on the upper forehead. In 8 cases, other types of immediate effluvium were observed, but these were not linear (detailed in Table 1).
Description of linear effluvia and other variants of immediate onset associated with hair transplantation: epidemiological, surgical, and clinical characteristics in 28 patients.
| Patient | Sex, age (y) | First visit post-HT (1–3 days) | Second visit post-HT (7–9 days) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Temple surgery/Mickey Mouse pattern | Linear effluvium in the temples | Linear effluvium in the temples | Surgery of upper forehead/Posterior linear effluvium | Surgery of the crown/Donut pattern | Other types of immediate concurrent effluvium | ||||
| Diameter, mm | Coloration | Diameter, mm | Coloration | ||||||
| 1 | M-41 | Yes/Yes | 3 | Erythema | 20 | Pale | Yes/Yes | No | No |
| 2 | M-21 | Yes/Yes | 5 | Pale | 10 | Pale | Yes/Yes | No | |
| 3 | M-51 | Yes/Yes | 3 | Erythema | 10 | Pale | Yes/Yes | No | No |
| 4 | M-37 | Yes/Yes | 4 | Erythema | 20 | Pale | Yes/Yes | No | No |
| 5 | M-35 | Yes/Yes | 6 | Erythema | 20 | Pale | Si/Yes | No | No |
| 6 | M-27 | Yes/Yes | 3 | Pale | 10 | Pale | Yes/Yes | Yes/Yes | No |
| 7 | M-47 | Yes/Yes | 5 | Erythema | 18 | Pale | Yes/No | Yes/Yes | No |
| 8 | M-35 | Yes/Yes | 3 | Pale | 13 | Pale | No/No | Yes/No | No |
| 9 | M-37 | Yes/Yes | 5 | Pale | 8 | Pale | Yes/Yes | No | Linear effluvium posterior to restoration of temple triangles |
| 10 | M-35 | Yes/Yes | 2 | Erythema | 10 | Pale | Yes/Yes | No | No |
| 11 | M-39 | Yes/Yes | 8 | Erythema | 25 | Pale | Yes/Yes | No | No |
| 12 | M-45 | Yes/Yes | 1 | Pale | 6 | Pale | Yes/No | No | No |
| 13 | M-48 | Yes/Yes | 1 | Erythema | 5 | Pale | Yes/Yes | No | No |
| 14 | M-44 | Yes/Yes | 5 | Pale | 23 | Pale | Yes/Yes | Si/Yes | Discrete diffuse confluence of both effluvia in the medial third |
| 15 | M-33 | Yes/Yes | 6 | Pale | 20 | Pale | Yes/Yes | Yes/Yes | Patchy interparietal effluvia |
| 16 | M-44 | Yes/Yes | 5 | Pale | 20 | Pale | Yes/Yes | Yes/Yes | Severe diffuse confluence of both effluvia in the medial third |
| 17 | M-33 | Yes/Yes | 12 | Pale | 30 | Pale | Yes/Yes | No | No |
| 18 | M-37 | Yes/Yes | 3 | Pale | 8 | Pale | Yes/No | Yes/No | Anterior region of the crown |
| 19 | M-27 | Yes/Yes | 2 | Pale | 16 | Pale | Yes/Yes | Yes/Yes | No |
| 20 | M-38 | Yes/Yes | 2 | Erythema | 16 | Pale | Yes/Yes | No | Moderate diffuse confluence between the posterior regions of the temples |
| 21 | M-41 | Yes/Yes | 3 | Erythema | 25 | Pale | Yes/No | No | Interparietal effluvium |
| 22 | M-34 | Yes/Yes | 6 | Pale | 20 | Pale | Yes/Yes | Yes/Yes | No |
| 23 | M-31 | Yes/Yes | 5 | Pale | 12 | Pale | Yes/No | Yes/Yes | No |
| 24 | M-37 | Yes/Yes | 5 | Pale | 7 | Pale | Yes/No | Yes/No | No |
| 25 | M-50 | Yes/Yes | 3 | Erythema | 6 | Pale | Yes/Yes | Yes/Yes | Effluvium in the posterior region of the upper forehead of 4cm |
| 26 | M-39 | Yes/Yes | 10 | Pale | 20 | Pale | Yes/Yes | Yes/Yes | No |
| 27 | M-23 | Yes/Yes | 2 | Erythema | 8 | Pale | Yes/Yes | Yes/No | No |
| 28 | M-26 | Yes/Yes | 1 | Erythema | 13 | Pale | Yes/Yes | No | No |
Abbreviations: HT, hair transplant; M, male.
All patients showed a progressive increase in the diameter of the hair loss line, with a median of 10mm (range, 2–22mm), an effluvium common to the transplanted FU or ‘shock loss’ at 2–4 weeks (diffuse telogen effluvium was also observed in 2 patients in the recipient area 1–2 months later while there was no such occurrence in the donor area), and complete regrowth of the hair loss line secondary to the effluvium at the 3-month visit, even before the appearance of transplanted hair.
DiscussionWe describe 28 patients who developed a form of post-HT effluvium with clinical characteristics that have hitherto not been reported in the literature: linear morphology with immediate onset (1–3 days), with involvement of nontransplanted hair in the region of the temples after employing the dense packing technique (Mickey Mouse pattern), an increase in the diameter of the hair loss line over time (wave-like pattern), with possible onset after the first 9 days of concentric linear effluvium at the crown (donut pattern), as well as other concurrent nonlinear effluvia also not previously described as of immediate onset.
The relevance of this study lies in raising dermatologists’ awareness of these novel features, both in morphological terms (linear) and in timing (immediate onset and subsequent spontaneous resolution) to enable appropriate diagnosis and management. The dermatologists will also be able to provide advance warning to the patient to avoid subsequent stress and confusion associated with this process.
Different types of post-HT effluvium have been reported in the literature, although all these present later than those described in our study: (a) shock loss of transplanted grafts at 2–3 weeks2,6,7; (b) localized and diffuse telogen effluvia in the donor areas3,4; and (c) similar effluvia in recipient areas5 after 1–2 months. Conti et al.8 described 3 cases of effluvium around areas of surgical resection of tumor lesions on the scalp. These effluvia could be due to ischemia caused by tumescent anesthesia with epinephrine and suture traction. The authors concluded that they were dealing with anagen effluvium, given its rapid onset (1 month). In line with this concept, our cases could be considered an anagen effluvium, but with earlier onset.
The pathophysiologic mechanism underlining linear effluvium in our patients would seem to be the same as for other post-HT effluvia reported in the literature1–6; surgical trauma, physical and psychological stress, ischemia due to use of epinephrine, and pressure due to tumescent anesthesia. The dense packing used in our patients could induce a state of perilesional hypoxia that extends to effluvia around the area of follicular unit strip surgery3 or around the area of surgery with suture traction of the scalp,8 as well as effluvia in the donor areas due to overexploitation.4
There are hypotheses to explain the unique morphological characteristics and timing of the effluvia present in our study. First, the linear morphology could be the result of lower resistance of the miniaturized hair to this stress. In patients with androgenetic alopecia, the miniaturized FUs surround the areas of alopecia of the temples and crown, and so the morphology and final diameter of the effluvium would be limited concentrically to these areas. Second, the timing could be due to a domino effect that would affect the chronological order of the miniaturized FUs from greater to lower surgical stress: those next to dense packing surrounding the temples (Mickey Mouse pattern), local progression toward neighboring areas increasing the diameter (wave-like pattern), transfer of stress to distant miniaturized FUs around the crown (donut pattern), and, finally, confluence of the lines diffusely in the interparietal area. As a result of this process, we have denoted as primary effluvium that present first in the areas of dense packing (Mickey Mouse pattern), and as secondary effluvia those with later onset as a result of the primary one due to a domino effect (wave-like pattern, donut pattern, final diffuse effluvia). At the follow-up visit after 3 months, all effluvia had spontaneously resolved, even before the appearance of most of the transplanted hair.
In our experience, at the visit at 7–9 days, all patients had doubts and expressed concern that the grafts may not have been implanted in alopecic areas. We also had some doubts in the first few cases, with an impact on the relationship between physician and patient. The dermatologist should avoid such apprehension through awareness of the existence of this condition and explain to the patient that the process is self-limiting and reversible after 2–3 months.
The limitations of this study include its retrospective design, the technical difficulties in performing a trichogram, and the lack of biopsy, given that the condition was considered self-resolving. Future prospective studies would need to confirm whether this effluvium can be avoided with any type of medical treatment prior to HT to revert the miniaturized FUs, something that is uncommon in complete alopecia surgery of temples due to the limited margin for improvement, unlike in alopecia only of the crown (where we have never observed primary donut pattern) and in diffuse alopecias.
In conclusion, to the best of our knowledge we report new variants of effluvia of possible anagen post-HT origin with unique morphological characteristics (linear), timing (immediate onset), and clinical course (description of concepts of primary and secondary effluvia). The dermatologist should be aware of the possibility of the development of this type of alopecia in HT with hair restoration at the temples by dense packing, the common and differentiating characteristic in all our patients. To avoid major misunderstandings and resulting anxiety, we recommend taking intraoperative and immediate postoperative photographs demonstrating the union of the transplanted and nontransplanted areas, as well as discussing with the patient this transient phenomenon that resolves after 3 months before the operation.
Conflicts of interestThe authors declare that they have no conflicts of interest.