Heparin-induced hemorrhagic bullous dermatosis (HBD) is a benign condition, first described by Perrinaud back in 2006.1–3 We report six cases of HBD in adult patients examined in the Dermatology Department of the Italian Hospital of Buenos Aires, Argentina from September 1, 2020 through January 31, 2022. Demographic, clinical, and evolutionary characteristics were obtained from the patients’ electronic health records (figures 1-3).
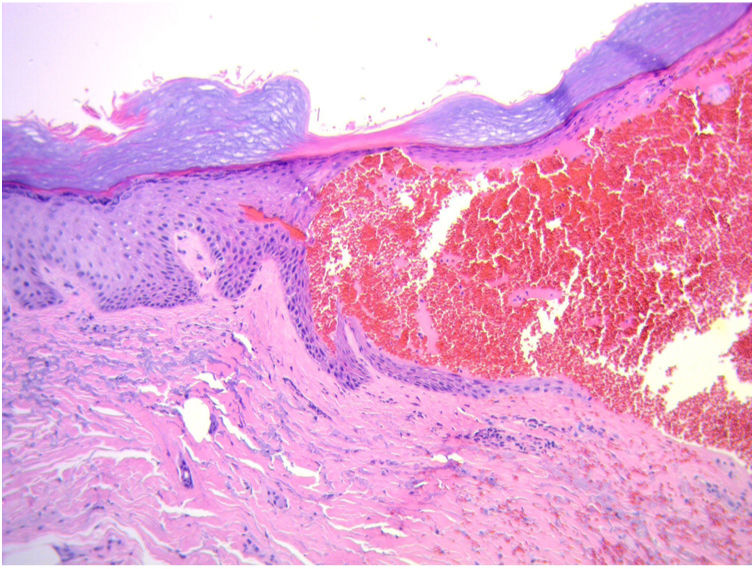
Three patients were women, with an age range from 50 to 78 years. Patients were on anticoagulant therapy (5 on enoxaparin and 1 on sodium heparin). The time elapsed between the start of the drug and symptom onset varied from three days to four years. All of them showed tense, hemorrhagic blisters in various locations. Histopathological examination of tissue biopsies and direct immunofluorescence (DIF) were performed in four patients. Three showed intraepidermal blisters; and one, dermoepidermal blisters with blood content. The DIF tested negative in all four cases. In all the patients, the lesions resolved in less than three weeks, and in one case, anticoagulant therapy had to be discontinued due to dermatosis (Table 1).
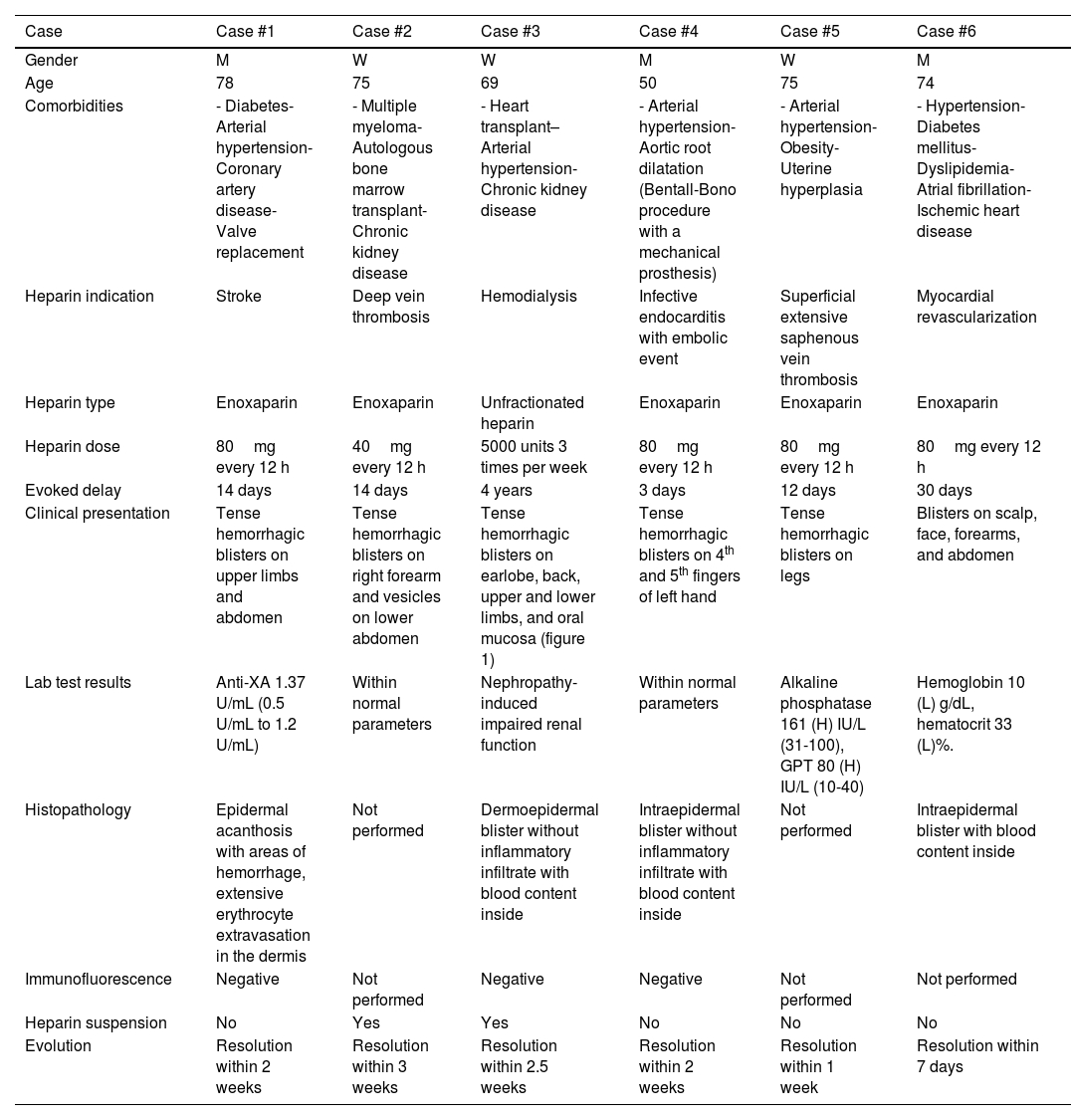
Clinical characteristics, type and dose of heparin, evoked delay, lab test results, histopathological finings, and evolution of 6 cases of patients with hemorrhagic bullous dermatosis.
| Case | Case #1 | Case #2 | Case #3 | Case #4 | Case #5 | Case #6 |
|---|---|---|---|---|---|---|
| Gender | M | W | W | M | W | M |
| Age | 78 | 75 | 69 | 50 | 75 | 74 |
| Comorbidities | - Diabetes- Arterial hypertension- Coronary artery disease- Valve replacement | - Multiple myeloma- Autologous bone marrow transplant- Chronic kidney disease | - Heart transplant– Arterial hypertension- Chronic kidney disease | - Arterial hypertension- Aortic root dilatation (Bentall-Bono procedure with a mechanical prosthesis) | - Arterial hypertension- Obesity- Uterine hyperplasia | - Hypertension- Diabetes mellitus- Dyslipidemia- Atrial fibrillation- Ischemic heart disease |
| Heparin indication | Stroke | Deep vein thrombosis | Hemodialysis | Infective endocarditis with embolic event | Superficial extensive saphenous vein thrombosis | Myocardial revascularization |
| Heparin type | Enoxaparin | Enoxaparin | Unfractionated heparin | Enoxaparin | Enoxaparin | Enoxaparin |
| Heparin dose | 80mg every 12 h | 40mg every 12 h | 5000 units 3 times per week | 80mg every 12 h | 80mg every 12 h | 80mg every 12 h |
| Evoked delay | 14 days | 14 days | 4 years | 3 days | 12 days | 30 days |
| Clinical presentation | Tense hemorrhagic blisters on upper limbs and abdomen | Tense hemorrhagic blisters on right forearm and vesicles on lower abdomen | Tense hemorrhagic blisters on earlobe, back, upper and lower limbs, and oral mucosa (figure 1) | Tense hemorrhagic blisters on 4th and 5th fingers of left hand | Tense hemorrhagic blisters on legs | Blisters on scalp, face, forearms, and abdomen |
| Lab test results | Anti-XA 1.37 U/mL (0.5 U/mL to 1.2 U/mL) | Within normal parameters | Nephropathy-induced impaired renal function | Within normal parameters | Alkaline phosphatase 161 (H) IU/L (31-100), GPT 80 (H) IU/L (10-40) | Hemoglobin 10 (L) g/dL, hematocrit 33 (L)%. |
| Histopathology | Epidermal acanthosis with areas of hemorrhage, extensive erythrocyte extravasation in the dermis | Not performed | Dermoepidermal blister without inflammatory infiltrate with blood content inside | Intraepidermal blister without inflammatory infiltrate with blood content inside | Not performed | Intraepidermal blister with blood content inside |
| Immunofluorescence | Negative | Not performed | Negative | Negative | Not performed | Not performed |
| Heparin suspension | No | Yes | Yes | No | No | No |
| Evolution | Resolution within 2 weeks | Resolution within 3 weeks | Resolution within 2.5 weeks | Resolution within 2 weeks | Resolution within 1 week | Resolution within 7 days |
The purpose of reporting this case series is to raise awareness of a little-known disease, prevent its underdiagnosis, and review its therapeutic management.
HBD is considered a rare condition, and its incidence is unknown to date. It is more commonly seen in men of advanced age, with a mean age at presentation of 70 years, which is similar to the cases reported.2,3
It has been reported that HBD can be due to the use of any type of heparin, primarily enoxaparin, and exceptionally, oral anticoagulants such as warfarin and rivaroxaban.3–5
The pathophysiology of HBD has not yet been elucidated, and four hypotheses have been proposed. One suggests a dose-dependent reaction, as it has been reported in some patients on high doses of heparin. The second theory postulates a synergistic mechanism for patients on one or more anticoagulants, or antiplatelet agents. The third considers cutaneous fragility as the underlying mechanism. Lastly, some authors suggest that the onset of lesions at the site of heparin application could be indicative of a type IV hypersensitivity mechanism.2,3
The onset delay reported to date ranges from 5 to 21 days. However, cases have been reported in which the clinical signs developed anywhere from a few hours to nine months after the start of anticoagulant therapy.2 In case #3 of this series, the onset delay was four years, which raised doubts on its diagnosis. However, additional studies ruled out other conditions, and the disease improved after discontinuing anticoagulant therapy. This would be the first case ever reported with such a prolonged latency.
The clinical presentation of HBD is characterized by tense, hemorrhagic blisters located on the extremities.2 Mucous membranes are often spared, yet HBD can still compromise the oral mucosa, or manifest with exclusive involvement of the oral mucosa.6 Koebner phenomenon may be present, as it was the case of one of the patients from this series.
The histopathology of the lesions is nonspecific and typically shows intraepidermal blisters with blood content, as was the case of 3 patients from this series, although subcorneal or subepidermal blisters have been reported as well. DIF of perilesional skin turns out negative.2,3 Therefore, skin biopsy may not be necessary for diagnosis if the clinical features and history are suggestive of this disease. Due to its clinical characteristics, other diagnoses were considered in case #3 of this series (bullous pemphigoid and linear IgA disease). However, DIF turned out negative, and lesions improved after discontinuing the anticoagulant therapy, which allowed us to achieve the diagnosis of HBD. This case is different from the others though and is associated with the sodium heparin therapy the patient was on during hemodialysis. This raises questions on the relationship between the type of heparin used, the route of administration, pathophysiology, and disease severity.2–4
Because the natural course of this dermatosis is benign and tends to be self-limiting, it is often deemed unnecessary to discontinue or modify anticoagulant therapy. In most cases, the lesions spontaneously resolve in three weeks. However, in case #3, due to the severity of the disease, heparin therapy had to be discontinued.1–3
In conclusion, HBD is a little-known condition, which could contribute to its underdiagnosis. HBD is considered an adverse reaction to heparin and is diagnosed clinically. Although it is not deemed necessary to make any changes to anticoagulant therapy as it is self-limiting in a matter of weeks, this may be necessary in some cases.
FundingNone declared.
Conflicts of interestNone declared.