Dermatofibrosarcoma protuberans (DFSP) is a slow-growing cutaneous tumor of fibrohistiocytic origin characterized by a high capacity for recurrence and local destruction with a low metastatic potential (<1%).1 Despite its low incidence rate, DFSP is the most common cutaneous sarcoma.2 Its incidence rate is higher in black individuals, the mean age of onset is between 40 and 43 years, and there is a slight predominance in women.3–5 The most common locations are the trunk (40% up to 60%), limbs (20% up to 30%), and head (10% up to 15%).3 Although its etiology remains unknown, there is a history of local trauma in 10% up to 20% of cases, suggesting that it could be a triggering factor.6 Although the histogenesis of DFSP is uncertain, the most accepted theory is that it originates from a pluripotential neuromesenchymal cell.7
The asymmetrical growth and poor clinical delimitation justify the observation that up to 21% of cases present local recurrence (LR) within 5 years after treatment.8 Multiple therapeutic guidelines recommend delayed Mohs micrographic surgery (MMS) as the treatment of choice, relegating conventional surgery (CS) with wide margins for cases in which it is not feasible, and reserving radiotherapy (RT) and treatment with imatinib for special situations.1 An incidence rate of LR of 3.7% after CS vs 1.7% after MMS has been estimated, showing significant differences between the 2.9
The primary endpoint of our study was to define the characteristics of patients with DFSP at our center, and the endpoint objective was to define the differences in management between those treated by the Dermatology Service of our hospital vs other specialties.
We conducted a retrospective descriptive study, consecutively including all patients with a histological diagnosis of DFSP from January 2010 through August 2022 at Hospital Universitario Puerta del Mar, Cádiz, Spain. Epidemiological, clinical, and treatment variables were collected, and data were analyzed globally and subsequently based on whether they were treated by the Dermatology Service (Group #1) vs other specialties (Group #2). Measures of central tendency and dispersion were taken for quantitative variables, and frequency distribution measures were used for qualitative variables, depending on their distribution. For the latter, the Kolmogorov-Smirnov test was used to check if quantitative variable followed a normal distribution. Inferential analyses were performed using the Student's t-test for quantitative variables and the chi-square test for qualitative variables. The level of statistical significance was set at p<0.05. The IBM-Statistical Package for the Social Sciences (SPSS) version 27 (IBM Company) program was used.
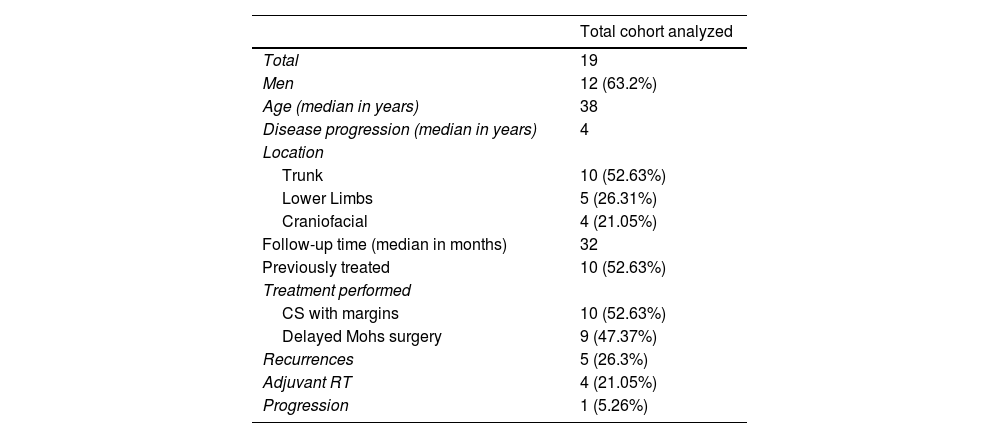
A total of 19 patients were identified, 12 (63.2%) of whom were men, with a median age of 38 years (range, 16-77). The most common locations were the trunk (11 [57.9%]), the lower limbs (4 [21%]) and craniofacial (4 [21%]). The median course of the disease was 4 years (range, 1-30), and 10 (52.6%) had received some previous treatment. The median follow-up time after treatment was 32 months (3-141) (Table 1).
Results of the entire cohort analyzed.
| Total cohort analyzed | |
|---|---|
| Total | 19 |
| Men | 12 (63.2%) |
| Age (median in years) | 38 |
| Disease progression (median in years) | 4 |
| Location | |
| Trunk | 10 (52.63%) |
| Lower Limbs | 5 (26.31%) |
| Craniofacial | 4 (21.05%) |
| Follow-up time (median in months) | 32 |
| Previously treated | 10 (52.63%) |
| Treatment performed | |
| CS with margins | 10 (52.63%) |
| Delayed Mohs surgery | 9 (47.37%) |
| Recurrences | 5 (26.3%) |
| Adjuvant RT | 4 (21.05%) |
| Progression | 1 (5.26%) |
CS: conventional surgery; RT: radiotherapy.
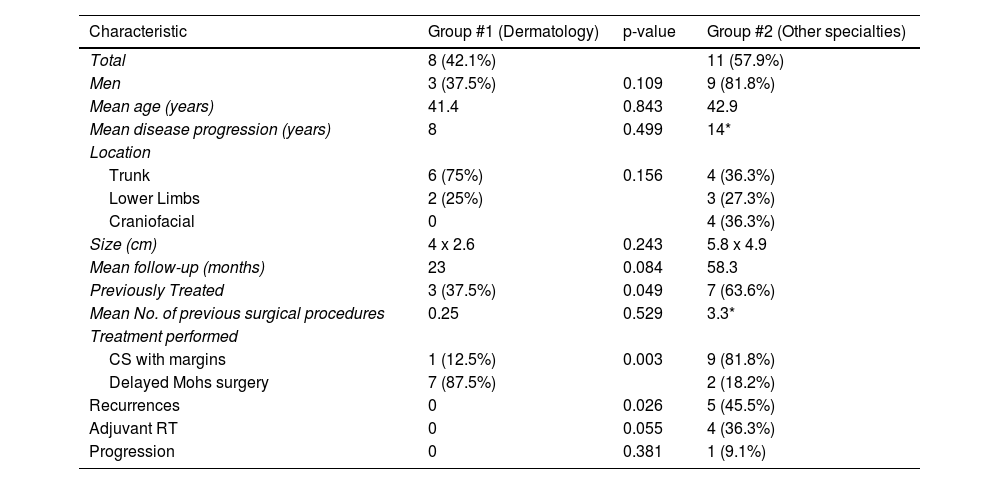
The comparative analysis between the 2 groups can be seen in Table 2. Group #1 differed significantly from Group #2 in that it included patients who had not been previously treated (37.5% vs 63.6%, p=0.049), were mostly treated with MMS (87.5% vs.18.2%; p=0.003), and had a lower rate of LR at the follow-up (0% vs 45.5%; p=0.026). No significant differences were seen regarding sex, age, disease progression, location, size, follow-up time, No. of previous surgeries, adjuvant RT, or progression.
Comparative analysis results between the 2 groups: group #1 (treated in the dermatology service) and group 2# (treated in other services at the same center).
| Characteristic | Group #1 (Dermatology) | p-value | Group #2 (Other specialties) |
|---|---|---|---|
| Total | 8 (42.1%) | 11 (57.9%) | |
| Men | 3 (37.5%) | 0.109 | 9 (81.8%) |
| Mean age (years) | 41.4 | 0.843 | 42.9 |
| Mean disease progression (years) | 8 | 0.499 | 14* |
| Location | |||
| Trunk | 6 (75%) | 0.156 | 4 (36.3%) |
| Lower Limbs | 2 (25%) | 3 (27.3%) | |
| Craniofacial | 0 | 4 (36.3%) | |
| Size (cm) | 4 x 2.6 | 0.243 | 5.8 x 4.9 |
| Mean follow-up (months) | 23 | 0.084 | 58.3 |
| Previously Treated | 3 (37.5%) | 0.049 | 7 (63.6%) |
| Mean No. of previous surgical procedures | 0.25 | 0.529 | 3.3* |
| Treatment performed | |||
| CS with margins | 1 (12.5%) | 0.003 | 9 (81.8%) |
| Delayed Mohs surgery | 7 (87.5%) | 2 (18.2%) | |
| Recurrences | 0 | 0.026 | 5 (45.5%) |
| Adjuvant RT | 0 | 0.055 | 4 (36.3%) |
| Progression | 0 | 0.381 | 1 (9.1%) |
CS: conventional surgery; RT: radiotherapy.
The analyzed cohort presented epidemiological characteristics—age, location, size, and evolution time—similar to other published cohorts, except for a higher prevalence of men.3,10 In the comparative analysis, significant differences were seen in the number of previously treated patients, the number of LRs, and the type of surgery performed, highlighting a greater use of MMS in Group #1, resulting in a lower rate of LR. Additionally, the comparative analysis also highlighted striking differences between the 2 groups in disease progression, No. of previous surgical procedures performed, and administration of adjuvant RT (higher in Group #2), although none reached statistical significance. The greater No. of previous interventions, higher No. of LRs at the follow-up, and greater need for adjuvant RT seen in Group #2, possibly mainly due to multi-operated patients and some with affected surgical margins may suggest a greater complexity in the patients treated in this group.
The limitations of this work stem from its retrospective nature, including data loss in variables such as the number of previous surgical procedures and disease progression, which did not allow for significant differences to be obtained in the comparative study.
The results obtained are consistent with the superiority of MMS over CS in the treatment of DFSP observed in the literature. This study concludes that the care and treatment of DFSP by MMS by the Dermatology Service reduces the number of recurrences and, consequently, may avoid the need for adjuvant RT and its associated morbidity. Therefore, it would be advisable for DFSP to be treated in services that perform MMS, and, if not possible, refer to the reference unit.