The benefit of lower limb compression therapy is not limited to chronic venous insufficiency or/and lymphoedema. Thanks to its anti-edema and anti-inflammatory effects, compression therapy is considered a beneficial adjuvant therapy to treat atypical wounds, inflammatory dermatoses, cellulitis, and traumatic wounds in the absence of contraindications. Strict contraindications are limited to severe peripheral arterial disease and decompensated heart failure. The variability of commercially available compression materials and systems, such as short-stretch bandages, multi-component systems, zinc oxide bandages, medical adaptive compression systems, ulcer compression stockings or medical compression stockings, facilitates the adaptation of compression therapy to the individual needs of each patient. Compared to venous leg ulcers, low pressures of 20mmHg are often sufficient to treat dermatological disorders, with higher patient tolerance and compliance.
El beneficio de la terapia compresiva en miembros inferiores no se limita a la insuficiencia venosa crónica y/o al flebolinfedema. Por su efecto antiedema y su acción antiinflamatoria puede considerarse una terapia adyuvante beneficiosa, por ejemplo, para heridas atípicas, dermatosis inflamatorias, celulitis y heridas traumáticas, siempre que no haya contraindicación. Las contraindicaciones estrictas se limitan a la arteriopatía periférica grave y la insuficiencia cardíaca descompensada. La variabilidad de sistemas de compresión disponibles en el mercado, como vendas de corto estiramiento, vendajes multicomponente, vendas de óxido de zinc, sistemas de compresión con cierre de velcro o medias de compresión, facilitan la adaptación de la terapia compresiva a las necesidades de cada persona. Al contrario que en la insuficiencia venosa crónica, en la enfermedad dermatológica habitualmente se necesitan bajas presiones (20mmHg), con una consiguiente mayor tolerancia y mayor cumplimiento de los pacientes.
Regardless of its etiology, the inflammatory process of any leg injury is associated with changes to microcirculation, with increased capillary filtration, and, due to the force of gravity, with an increased IV pressure. Therefore, despite the absence of reflux or an obstructive cause, a state of venous hypertension may develop, hindering injury healing. The term “hydrostatic ulcers” has been proposed to refer to leg injuries of various etiologies that meet this condition.1 This group includes injuries in obese patients, with immobilization, traumatic injuries, wounds due to autoimmune disease (vasculitis, pyoderma gangrenosum), and many others. Additionally, it is not uncommon for a patient to exhibit several of these predisposing conditions at the same time.1,2
Of note that any painful ulcer will make the person to move less, and this immobilization, often with the legs in decline, will increase edema and delay healing.
The recent publication of an interesting review on compressive therapy in dermatology by Dissemond et al., which also includes inflammatory dermatoses, has motivated the authors of this publication to conduct a review in Spanish of this necessary—and often unknown—therapy in our dermatological practice.3
Basic and physiological principles of compressive therapyThe effects of compressive therapy most widely investigated include the reduction of edema and constriction of vein lumens, leading to a decrease in venous blood volume in the leg. Additionally, there is a decrease in capillary filtration, increased local lymphatic drainage, reduction of inflammation, increased arterial flow, and pain reduction.1,3
The effectiveness of compressive therapy depends on the applied pressure, overlap between layers of such material, proper application of materials, and patient adherence. As mentioned in a previous article on compressive therapy in venous ulcers,4 a bandage becomes a dressing when applied to the patient's leg, and therefore, their properties differ. If we overlap materials with different physical properties, then the dressing will be called multicomponent. A bandage is more or less elastic or stretchable, while the dressing is more or less rigid. Rigidity is defined as the resistance of the dressing to changes in muscle volume in the calf. Friction between layers of a dressing, especially if there is a cohesive component, or between 2 stockings, increases its rigidity. The greater the rigidity, the more effective it is in reducing venous hypertension while walking (ambulatory venous hypertension) because, by presenting resistance to muscle contraction, elevated pressure peaks are achieve that create brief and intermittent venous occlusions, which is a similar phenomenon to valvular physiological functioning. During rest, these peaks do not occur, and pressure is lower.5
To promote the healing of venous ulcers, the recommendation is to apply strong pressure at the upper ankle, somewhere between 40mmHg and 60 mmHg.6 This measurement is taken with a device placed on the ankle that indicates the pressure exerted at that point at rest (point B1=transition point between the Achilles tendon and the gastrocnemius muscle). However, the pressure exerted varies at each point of the leg and depends on different factors, all of which are covered in Laplace's famous law7: the pressure underneath the bandage at a given point is greater the more pressure is exerted (force applied to the dressing during its application), the more layers there are, the smaller the circumference radius is at that point of the limb (greater prominence, e.g., pretibial region), and the narrower the bandage width is. The ability to maintain that degree of pressure over time depends on the properties of the dressing components, and on the patient's mobility. Padding techniques are explained by this physical law too.4
In addition to exercises involving plantar venous pump activation and calf muscle contraction, leg elevation while at rest is essential to optimize the anti-edema effect of compressive therapy.
Compressive therapy in atypical injuries and other inflammatory dermatological diseasesThe benefits we have just seen, especially regarding edema reduction, may justify the recommendation to use compressive therapy, provided it is not contraindicated, in any leg with an injury.1
Although a recent review concludes that few studies have been published supporting the use of compression for non-venous leg ulcers,8 clinical practice experience in the management of traumatic ulcers and atypical injuries due to pyoderma gangrenosum, necrobiosis lipoidica, or vasculitis demonstrates that it may promote the healing of these wounds.2,8
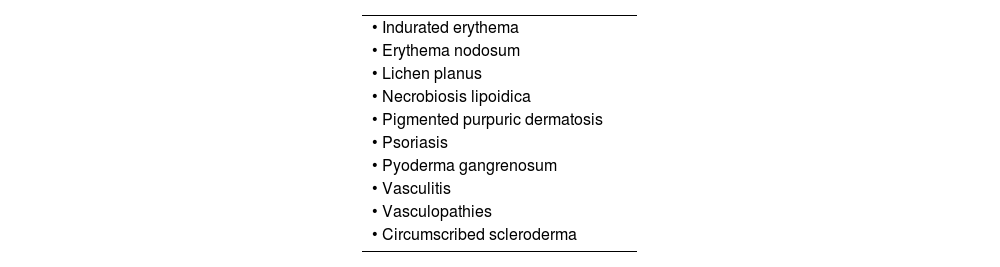
Furthermore, the benefit on microcirculation and inflammation justifies the indication of compressive therapy in various inflammatory dermatological diseases. In fact, by preventing capillary hypertension, compressive therapy helps treat and prevent edema-induced skin complications. In addition to promoting vasodilation and capillary perfusion by releasing nitric oxide and prostacyclins, compressive therapy may increase capillary density and diameter. A release of anti-inflammatory mediators by endothelial cells has also been demonstrated.9–11Although very few reports have been published on compressive therapy to treat inflammatory leg dermatoses, there are numerous expert recommendations regarding its use in various inflammatory diseases (Table 1).
In the routine clinical practice, we often see that certain generalized inflammatory dermatoses are much more persistent and pronounced in the legs than in other anatomical regions. For example, psoriasis plaques are usually refractory to treatment vs other affected body areas. Although the cause is still to be elucidated it has been hypothesized that inflammation is more prone to edema, in such a way that the resolution of the inflammatory reaction is somehow slowed down by venous stasis.12 Although the interest in adjuvancy with compressive therapy in psoriasis has only been described in isolated cases—in addition to the pressure effect—the benefit of dressing occlusion should also be considered.3
Regarding vasculitis, the authors of a retrospective and single-center uncontrolled study on the clinical course of 31 patients with various forms of cutaneous vasculitis and adjuvancy with short-stretch compression bandages concluded that the therapeutic response possibly improved while compression-related systemic immunosuppression decreased.13
Regarding livedoid vasculopathy, given the thrombotic occlusion of cutaneous vessels that occurs, compressive therapy could, in addition to promoting healing, prevent recurrence, based on expert recommendations.14
Regarding pyoderma gangrenosum, despite the scarce studies available, experts agree that patients benefit from compressive therapy thanks to its anti-inflammatory action.15
Expert recommendations also include compressive therapy for the management of necrobiosis lipoidica,16,17 and cases have been published on its benefit in other diseases, such as erythema nodosum18,19 or pigmented purpuric dermatosis.3
Dermatological surgery and compressive therapyAmong the possible causes of a chronic leg injury, a history of surgical excision is not uncommon. In many cases, we associate this healing stagnation with chronic venous insufficiency, yet this situation has also been reported in patients without underlying disease. As mentioned in the introduction, despite the absence of reflux or an obstructive condition, a state of venous hypertension that hinders wound healing can develop in any leg injury.1 In this context, a postoperative injury will benefit from anti-gravity measures, whether we have confirmation of underlying venous insufficiency or not.
Although within the first few days, rest with the lower limb properly elevated is the most important anti-gravity recommendation, applying a compressive bandage or compression stocking will help the patient return to their routine activities much sooner. Patients without clinical signs of chronic venous insufficiency may discontinue the use of compression bandages or stocking once the wound has closed, provided there are no other signs of local inflammation, and no edema occurs after discontinuing use.20
If not contraindicated, the use of compressive therapy right after surgical interventions on the leg limits the inflammatory phase and accelerates wound healing. This therapeutic strategy optimizes surgical outcomes in the lower limb and prevents suture dehiscence and graft and flap necrosis.20 In fact, therapeutic compression promotes the fixation and uptake of grafts—both in seal and laminar form—in leg ulcers.21
Scars and compressive therapyRegarding pathological scars, hypertrophic scars, and keloids, early application of compressive therapy is recommended, even prophylactically.22 Although the underlying pathophysiology is not fully understood, we know that scar compression reduces capillary perfusion and affects fibroblast differentiation and proliferation, resulting in a decrease in type I and type III collagen.23–25 Studies have shown that adjuvancy with compressive therapy leads to a significant reduction in pain and better scar elasticity within 2 to 4 months.26 The results obtained confirm the anti-inflammatory action of compression, which is why it is recommended both preventively and therapeutically, especially in patients with burns.
Contraindications and new indicationsA relevant question in clinical practice is: which are the contraindications for compressive therapy? In principle, externally and continuously applied pressure should not exceed intra-arterial and arteriolar pressure. Therefore, it has been established that compressive therapy is contraindicated with an ankle-brachial index (ABI) <0.6.27 However, patients with mild peripheral artery disease (PAD) can benefit from compressive therapy. In fact, an increased arterial flow has been demonstrated in these patients with the use of high-rigidity bandages or pneumatic compression devices.27 In immobile patients with PAD and ABI >0.5, bandaging with a high rigidity index with pressures <30mmHg is a safe and effective option if foot dorsiflexion exercises are performed. Additionally, a dual benefit can be achieved, as the resulting reduction in edema can improve arterial flow.28
In this context of understanding the benefit of compressive therapy as the best anti-inflammatory and anti-gravity treatment for leg ulcers, an expert consensus has established only the following 2 situations as contraindications for compressive therapy: severe PAD and severe heart failure (NYHA FC III and IV).29
Consequently, in addition to the growing spectrum of indications for compressive therapy, even traditional contraindications such as cellulitis have become indications for it. A recent study has shown that initiating compressive therapy together with antibiotic therapy, not only does not increase the risk of infection spread, but also reduces inflammation, edema, and eventually the risk of secondary ulcers.30,31
Injuries in older adults and compressive therapyIn a society where the elderly population is increasing, and we are living longer, leg ulcers associated with physiological changes due to aging are becoming increasingly common. Such as in the case of ulcers due to dermatoporosis (skin tears, deep dissecting hematomas) (Fig. 1), and the spectrum of lesions due to arteriolosclerosis. Additionally, comorbidities involving edema and delayed healing, such as heart failure or chronic venous insufficiency, are more common in older individuals. Congestive heart failure is the most common cause for hospitalization in older people and a risk factor to develop chronic wounds.
Although severe congestive heart failure is considered a contraindication for compressive therapy, less severe stages benefit from it both to prevent and treat ulcers resulting from increased diffusion space. During episodes of decompensated heart failure, the space between capillaries and tissue increases. This leads to poorer nutrient diffusion and, consequently, a decrease in cutaneous perfusion. In these less severe cases, the progressive increase in the compression device pressure only produces very brief phases of increased cardiac load capable of facilitating substantial reduction in peripheral edema.32,33
Considering that heart failure is a typical syndrome of old age, it is not uncommon for the same individual to present simultaneously a certain degree of arterial or arteriolar disease, chronic venous and lymphatic insufficiency, and dermatoporosis, which increases the risk of torpid ulcers. Indeed, it is not uncommon for skin tears, Martorell ulcers (those due to subcutaneous ischemic arteriolosclerosis), or arterial ulcers to develop following an episode of decompensated heart failure (Fig. 2). Furthermore, heart failure is considered a risk factor for venous ulcers.34
Compressive therapy, tailored to the needs of each patient, and always adjunctive to heart failure therapy, can have a significant impact on the prevention and treatment of leg injuries in older adults.35
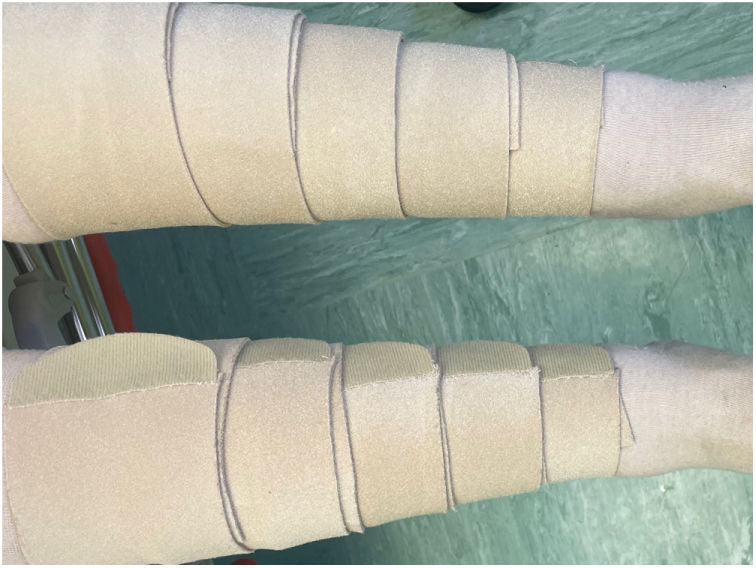
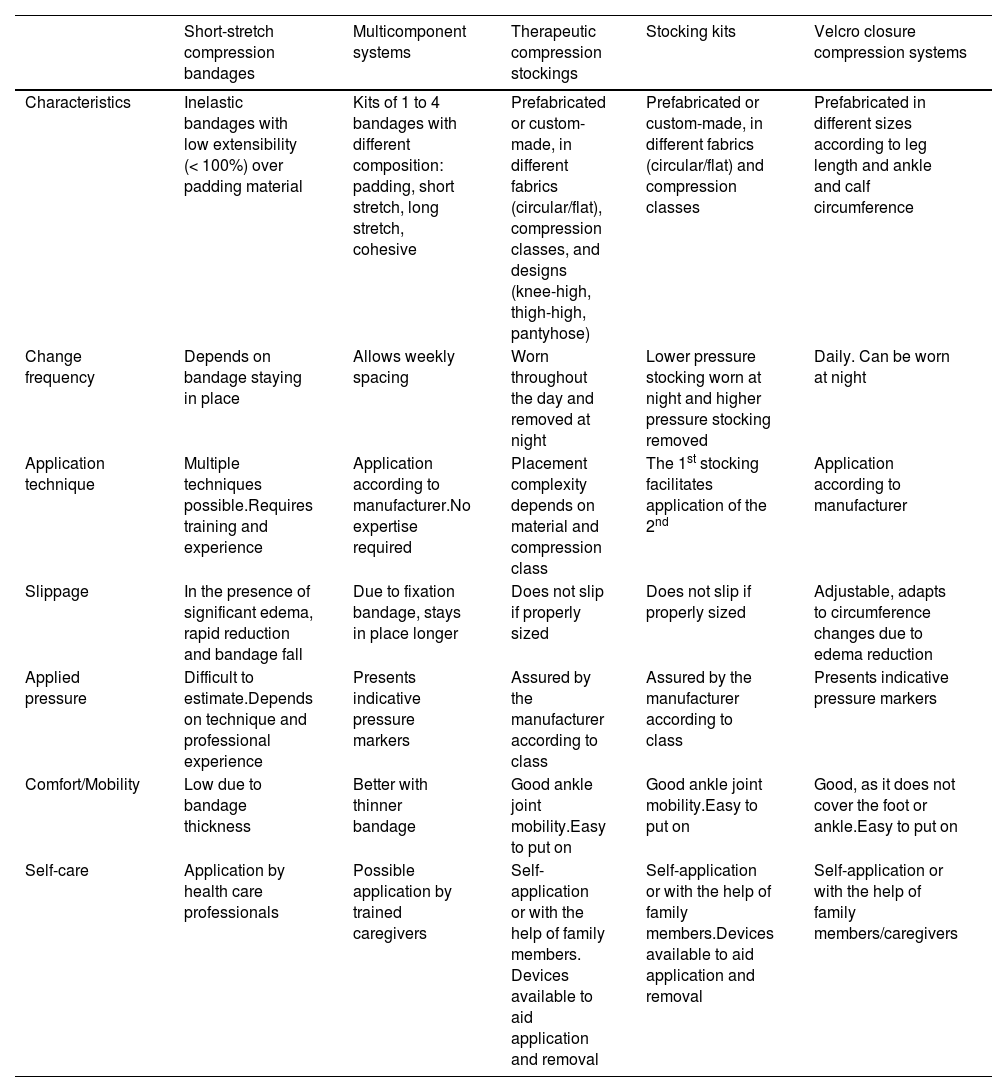
Types of systems and materials used in compressive therapyThe choice of material and compression system depends on the treatment phase and the needs and physical capabilities of each individual (Table 2). Although walking is directly associated with the effectiveness of compression, in case of immobility, the flexion and extension movement of the ankle joint during rest activates the plantar and calf muscle pump, thus increasing the effectiveness of compressive therapy in these patients.4
- -
Short-stretch compression bandages
Characteristics of various compression systems.
| Short-stretch compression bandages | Multicomponent systems | Therapeutic compression stockings | Stocking kits | Velcro closure compression systems | |
|---|---|---|---|---|---|
| Characteristics | Inelastic bandages with low extensibility (< 100%) over padding material | Kits of 1 to 4 bandages with different composition: padding, short stretch, long stretch, cohesive | Prefabricated or custom-made, in different fabrics (circular/flat), compression classes, and designs (knee-high, thigh-high, pantyhose) | Prefabricated or custom-made, in different fabrics (circular/flat) and compression classes | Prefabricated in different sizes according to leg length and ankle and calf circumference |
| Change frequency | Depends on bandage staying in place | Allows weekly spacing | Worn throughout the day and removed at night | Lower pressure stocking worn at night and higher pressure stocking removed | Daily. Can be worn at night |
| Application technique | Multiple techniques possible.Requires training and experience | Application according to manufacturer.No expertise required | Placement complexity depends on material and compression class | The 1st stocking facilitates application of the 2nd | Application according to manufacturer |
| Slippage | In the presence of significant edema, rapid reduction and bandage fall | Due to fixation bandage, stays in place longer | Does not slip if properly sized | Does not slip if properly sized | Adjustable, adapts to circumference changes due to edema reduction |
| Applied pressure | Difficult to estimate.Depends on technique and professional experience | Presents indicative pressure markers | Assured by the manufacturer according to class | Assured by the manufacturer according to class | Presents indicative pressure markers |
| Comfort/Mobility | Low due to bandage thickness | Better with thinner bandage | Good ankle joint mobility.Easy to put on | Good ankle joint mobility.Easy to put on | Good, as it does not cover the foot or ankle.Easy to put on |
| Self-care | Application by health care professionals | Possible application by trained caregivers | Self-application or with the help of family members. Devices available to aid application and removal | Self-application or with the help of family members.Devices available to aid application and removal | Self-application or with the help of family members/caregivers |
Translated from Dissemond et al.3
These bandages stretch little (<100%).6 They are rigid, with low resting pressures and high working pressures, with significant pressure peaks associated with muscle contraction. Before their application, padding material (usually cotton) is applied to avoid areas of hyperpressure and homogenize perimeters.
The main objectives of padding are the following ones3–7:
- -
Homogenize leg perimeters in patients with an impaired limb morphology.
- -
Protect bony prominences and other sensitive areas from hyperpressure (such as the pretibial region or the Achilles tendon area).
- -
Increase retromalleolar pressure in injuries located behind the malleolus to overcome the “tent effect” that usually occurs in that concave area.
- -
Avoid venous congestion (erythematous-violaceous discoloration) due to excess pressure to the skin microcirculation and the superficial venous system.
Regarding acral edema, toe bandaging can be applied. The main issue is that, in the decongestive phase, short-stretch compression bandages need to be renewed daily, as pressure is quickly lost with edema reduction.7 Due to movement, short-stretch compression bandages significantly lose pressure over a short period of time (within 30minutes).36–38 Another problem is that to achieve adequate pressure and maintenance over time with this type of bandage, the professional applying it must be trained and experienced. A positive aspect is that they can be washed and reused, always remembering that they usually lose their properties after the 10th-15th wash.3
- -
Zinc oxide bandages (Unna boot)
The traditional Unna boot remains a very interesting bandage alternative, with a special anti-inflammatory benefit for stasis dermatitis.38 In fact, its combination with medium-high potency topical corticosteroid cream is the treatment of choice for leg eczema due to venous hypertension (Fig. 3).
Zinc paste bandages are not too elastic or extensible (extensibility rate <10%). The Unna boot creates very high working pressure with low resting pressure, which eventually produces rapid decongestion in mobile patients.39 However, these pressures decrease as volume decreases. To help maintain them over time, a cohesive bandage is applied over them. Its application requires knowledge of the material and experience.3,4
- -
Multicomponent bandaging
It has become an alternative to short-stretch compression bandages. They are available as kits to be used with 1 to 4 bandages. They include various elements, such as padded bandages, short- and long-stretch compression bandages, special foam bandages—some of which contain zinc or calamine—and cohesive fixation bandages or combinations thereof.3,40
Unlike short-stretch compression bandages, the application of multicomponent bandages does not require knowledge of complex bandaging techniques. Furthermore, their application takes less time.41 In some systems, special stretching techniques of the bandage or visual markers provide an indication of the generated resting pressure and ensure proper fit (Fig. 4). The inclusion of a cohesive bandage as part of the kit helps keep it in place. When applied correctly, multicomponent systems achieve and maintain pressures ≥ 40mmHg for several days. Many manufacturers of multicomponent systems also offer “lite” versions that, when used correctly, produce a resting pressure of approximately 20mmHg. Multicomponent systems are not washable or reusable, but compared to reusable short-duration dressings, are more cost-effective since decongestion is achieved more quickly, resulting in fewer personnel and material spending.42 Compared to short-stretch compression bandages, multicomponent systems increase patient adherence due to better mobility, thinner bandages, easier shoeing, and less discomfort.
- -
Therapeutic compression stockings
The pressure they exert does not depend on the professional applying the bandage, and their use facilitates footwear, as well as other activities of daily living. There are several fabrics and models marketed, but they can be custom-made for patients with leg measurements outside the normal range. Depending on the type of knitting, they have been classified as circular knit and flat knit. This latter is stiffer and especially indicated in patients with phlebolymphedema.4
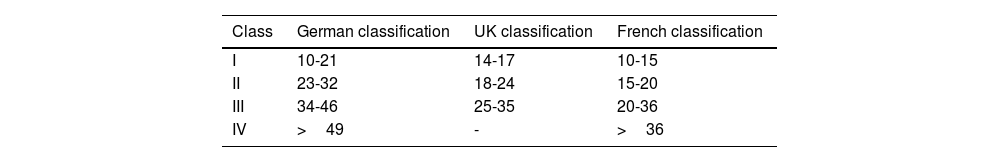
The classification of therapeutic compression stockings depends on the pressure exerted by the stocking at point B1. The most widely used in Spain is the German classification (Table 3). Two stockings are often used to treat venous ulcers and reach the recommended 30mmHg to 40mmHg, which makes their placement easier and allows for more rigidity. Furthermore, several devices have been marketed to facilitate their application.43
- -
Stocking kits for ulcer treatment
Depending on the manufacturer, lower stockings provide a resting pressure of 17mmHg to 22mmHg, keep the dressing in place, and facilitate the application of upper stockings. When they overlapped, the pressure values add up to compression in a similar way to a class III. The upper stocking can be removed at night, while the lower stocking, if possible, should be worn all day. Patients or their family members can apply these systems themselves, thus facilitating self-care. Furthermore, unlike compression bandages, these stocking systems are less bulky and allow for better ankle mobility, maintain a constant level of pressure and are less prone to slipping.3
- -
Velcro closure compression system
This is a type of adjustable compression device with low elasticity fabric and Velcro fastening. These systems produce resting pressures of 20mmHg to 50mmHg, depending on the system, if applied correctly. In some, the generated resting pressure can be visually controlled by markers, or specifically adjusted using stretching techniques. After a simple and quick training, they are easy to apply and remove, so the patient can put them on themselves if they can reach their feet while reclining and adjust pressure as it is gradually lost (Fig. 5). The stiffness obtained with these devices is similar to that obtained with short-stretch compression bandages, with the additional benefit that pressure can be readjusted throughout the day.3,4,44
- -
Intermittent pneumatic compression
These are devices formed by air chambers that surround the leg, connected to a system that creates gradual pressure from proximal to distal, alternated with intervals without pressure to achieve the passive activation of the muscle pump. In addition to thrombosis prophylaxis, an improvement in arterial flow has been observed.45 By repeatedly increasing and decreasing pressure, intermittent pneumatic compression promotes venous and lymphatic drainage while decongesting edema.46 Its main interest is to help other compression systems in immobile patients or in situations where other types of compression therapy cannot be used, such as edema in severe PAD situations.47
In addition to devices for clinics and medical offices, there are also home devices that can be prescribed temporarily or long-term and used independently by patients or their family members. The application duration is 30 to 60minutes and should be repeated up to 3 times a day.3
Questions arising in clinical practice- -
How much pressure is needed to treat non-venous leg ulcers?
There are no studies on the optimal pressure. However, this has not been thoroughly studied with injuries of different etiologies. In cases where we have an injury of a different cause, i.e, vasculitis, and chronic venous insufficiency, pressure should be closer to 40mmHg.
However, patients with inflammatory ulcers often do not tolerate initially elevated resting pressure values, which is why compression therapy systems with low resting pressure values—around 20 mmHg—can also be used.48,49 In the routine clinical practice, this is usually applied well with “lite” variants of multicomponent bandages, compression bandages with Velcro closures, or class 1 medical compression stockings.48,49
- -
Prefabricated or custom-made stockings?
For proper stocking fit, each limb should be measured individually. If the measured circumferences and lengths correspond to standard measurements, a standard compression stocking should be selected. Custom-made compression stockings are only necessary if there are significant discrepancies. Measurements should be taken after reducing edema whenever possible.3
- -
Circular or flat knit stockings?
When prescribing therapeutic compression stockings, circular knit stockings are considered the standard of care. Flat knit compression stockings should only be prescribed in special situations. These include significant circumferential changes in the limb or limbs with a conical shape or deep tissue folds, as seen in severe CVI, lymphedema, pronounced phlebolymphedema, and obese patients, among others.3
- -
Closed-toe or open-toe compression stockings?
The use of closed-toe compression stockings is considered the standard of care and offers the following advantages: a 2nd sock is not needed in cold climates, it is well tolerated even in the presence of hallux valgus, and it provides compression to the forefoot and toes area too.3 In case of toe discomfort (especially in the presence of hammer toes), or if devices are needed to facilitate placement, the use of a toeless stocking is preferable.
Conflicts of interestNone declared.