Hidradenitis suppurativa (HS) is a chronic immune-mediated inflammatory illness of the pilosebaceous-apocrine unit,1 that has a tremendous impact on the patients’ quality of life, deteriorating their health, and limiting their social relations.2,3 In an effort to optimize the management of this condition, some authors have categorized patients with HS into location-based clinical phenotypes,4 and predominant types of lesion (follicular, inflammatory, and mixed profiles).5 They have also tried to categorize the lesions, especially tunnels, using imaging modalities. Despite of its high prevalence (nearly 1% in developed countries) HS still remains relatively unknown to numerous health professionals, leading to delayed diagnosis, incorrect therapeutic approaches, and disease progression. Some authors have suggested that this progression, along with the presence of certain risk factors often associated with patients with HS, such as smoking and obesity, could lead to a potentially proinflammatory systemic environment that triggers comorbidities and lowers life expectancy, in a similar way to what has already been hypothesized for patients with psoriasis, resulting in more health care spending.6 The approval of adalimumab to treat moderate-to-severe HS by regulatory agencies marked a paradigm shift in the management of patients with the inflammatory phenotype, which has proven to be an independent risk factor for disease progression.5 In recent years, there has been a deeper understanding of the disease pathogenesis, including molecular pathways and interleukins (IL) other than TNF-alpha (IL1, IL-6, IL-10, IL-12/23, IL-17, IL-22, complement, and janus kinase, among others)7,8 that has led to the development of new molecules and the search for possible new indications in existing drugs, thus giving hope to many patients. Unfortunately, currently, due to the type and severity of the lesions, many patients currently require a combination of medical and surgical treatment.8 In many cases, advanced therapies are just a means to prepare the patient for potentially aggressive surgical interventions associated with a non-negligible rate of recurrence depending on the location and procedure performed. Additionally, there is significant heterogeneity in the use of scores/measurement systems in the routine clinical practice, further complicating the already complex standardized management.
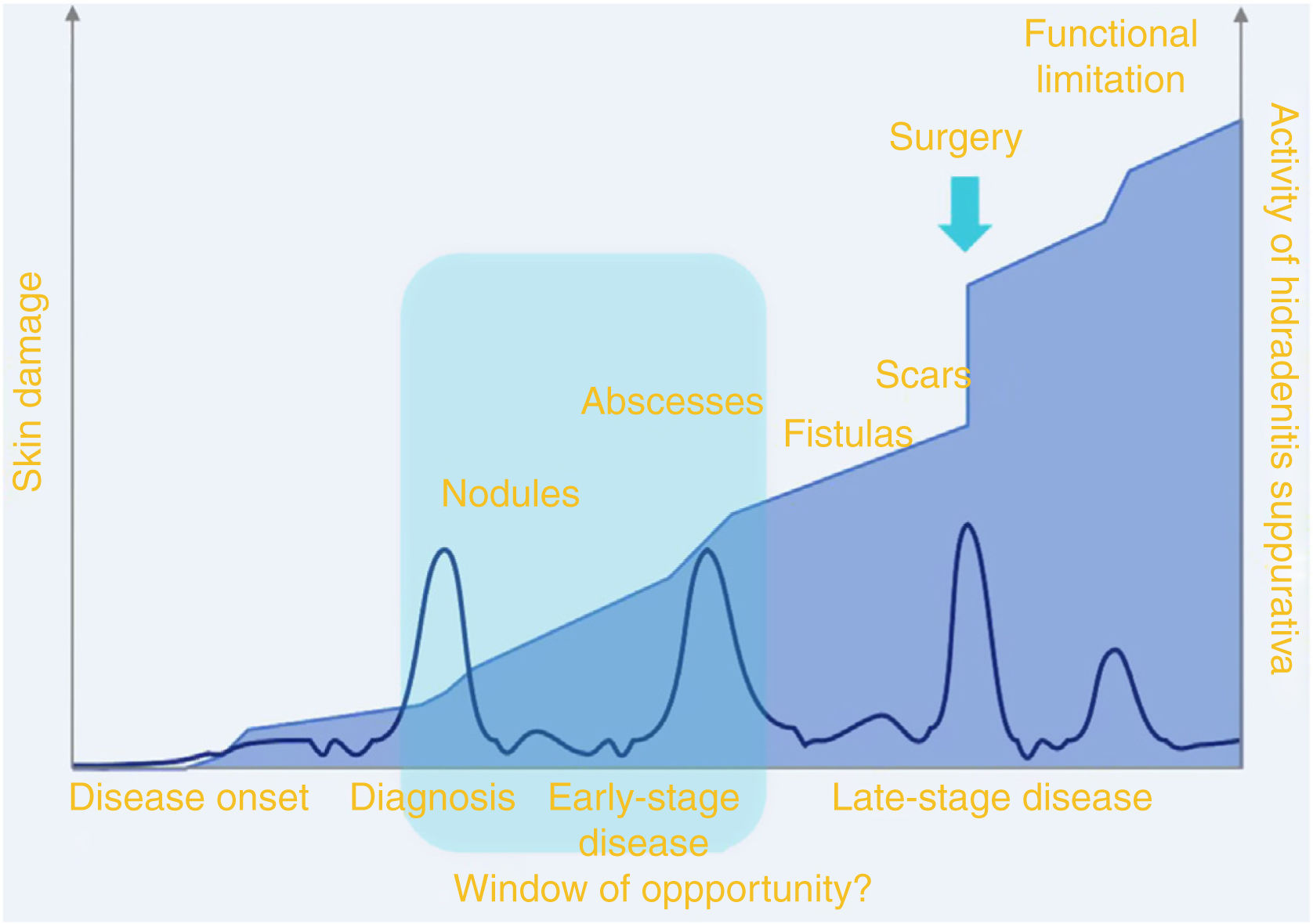
For all these reasons, it is of paramount importance to perform proper clinical assessments. Guided by non-invasive tools like the ultrasound,9 these assessments should enable us to achieve early diagnoses of the disease and its phenotype, identify active and subclinical lesions, and patients in the so-called “window of opportunity” (that stage of the disease when medical treatment is most effective because we’re dealing with reversible lesions). This is consistent with that stage in which patients exhibit nodular/abscess-type lesions (figure 1).10 In this group of patients, early and aggressive interventions with advanced therapies, along with a proper health educational strategy, could have a significant impact on prognosis. Overall, the patients who could be included in this category (table 1) are those who present with the Martorell's inflammatory phenotype, characterized by abscess-like onsets in the absence of comedone-like lesions.5 Also, individuals with an increasingly growing number of inflammatory nodules despite conventional systemic treatment, patients with perianal abscesses, and those with a mixed form of Martorell's HS,5 including patients with an initially follicular phenotype who start developing abscesses in > 2 anatomical areas, with a long history of smoking (< 10 cigarettes/day for > 10 years). This aggressive approach in the early stages of the disease could represent a paradigm shift in the management of this condition, thus preventing progression to mutilating forms of the disease, reducing cardiovascular risk, and improving the patients’ quality of life.
Graphical representation of the “window of opportunity.” Source: Martorell et al.10.
Main groups of patient included in the so-called “window of opportunity.”.
| These are the groups of patients potentially benefiting from early and aggressive treatment:a |
| A) Onset of HS with Martorell's inflammatory phenotype characterized by abscess-like onsets in the absence of comedone-like lesions. |
| B) Individuals with an increasingly growing the number of inflammatory nodules despite conventional systemic treatment. |
| C) Patients with perianal abscesses. |
| D) Individuals with a mixed form of Martorell's HS (patients with an initially follicular phenotype who start developing abscesses in > 2 anatomical regions) with a long history of smoking (<10 cigarettes/day for > 10 years). |
None declared.