The reconstruction of surgical defects in high-tension anatomical regions is challenging due to the ischemia and subsequent necrosis associated with tension closure. Research on new flaps capable of closing these defects exerting less tension would be a tremendous advancement in dermatological surgery.
Patients and methodsWe conducted a multicenter, retrospective study that used 2 new flaps-the bishop and the sigma ones-to repair surgical defects in high-tension regions such as the scalp, lower extremities, and the nasal pyramid. The bishop flap was used in 9 patients, 5 of whom exhibited their lesion in the nasal pyramid, 2 in the legs and another 2 in the scalp. The sigma flap was used in 6 patients, 5 of whom exhibited scalp lesions and 1 leg lesion.
ResultsUneventful and excellent results were obtained in all 15 patients due to infection, dehiscence, or necrosis.
ConclusionsBoth the bishop and the sigma flaps are a good alternative to repair surgical defects in high-tension regions such as the scalp, lower extremities, or the nasal pyramid.
La reconstrucción de defectos quirúrgicos en zonas anatómicas con elevada tensión supone un reto por la isquemia y posterior necrosis que conlleva el cierre forzado. La investigación de nuevos colgajos que consigan un cierre del defecto con menor tensión supondría un avance importante en la cirugía dermatológica.
Pacientes y métodosEstudio retrospectivo multicéntrico en el que se emplean 2 nuevos colgajos, el colgajo obispo y el colgajo sigma, para la reconstrucción de defectos quirúrgicos en zonas de elevada tensión como el cuero cabelludo, las extremidades inferiores y la pirámide nasal. El colgajo obispo se utilizó en 9 pacientes, de los cuales 5 tenían localizada la lesión en la pirámide nasal, 2 en las piernas y otros 2 en el cuero cabelludo. El colgajo sigma se empleó en 6 pacientes, 5 de ellos con lesiones en el cuero cabelludo y uno en la pierna.
ResultadosEn los 15 pacientes se obtuvieron resultados excelentes sin complicaciones por infección, dehiscencia o necrosis.
ConclusionesEl colgajo obispo y el colgajo sigma son una buena alternativa para defectos quirúrgicos en zonas de tensión elevada como el cuero cabelludo, las extremidades inferiores o la pirámide nasal.
There are anatomical areas, such as the scalp, lower extremities, and nasal pyramid, where the excision of a tumor creates surgical defects whose reconstruction poses a challenge. This is due to the high tension present in these areas, which makes it difficult to approximate and close the defects. When direct suture closure is not possible, skin flaps are used as a second option due to the similarity of the neighboring skin. However, many of the classic flaps used in other locations are not suitable for these special areas because of the high tension generated at the sutured edges, which predisposes to flap necrosis. Flaps that have proven useful in these locations, such as the double rotation O-Z flap on the scalp and the Keystone flap on the legs, have some limitations, such as the mobilization of a large amount of tissue on the scalp or the depth of detachment down to the muscular fascia in the lower extremities. Therefore, new flaps are needed for these high-tension areas that are safe in their viability and simple to perform, without requiring such extensive or deep dissections.
Material and methodsWe conducted a multicenter retrospective study that included patients with malignant tumors in high-tension areas such as the scalp, legs, and nose. Once the lesions were excised, the defects were reconstructed using 2 new flaps: the bishop flap and the sigma flap.
Data were collected on tumor location, size of the surgical defect, tumor histology, and follow-up on the viability of the flaps and recurrences. To arrive at the final design of these flaps, foam molds were initially used and subsequently experimented on pig skin with the corresponding design changes to ensure closure with the least possible tension.
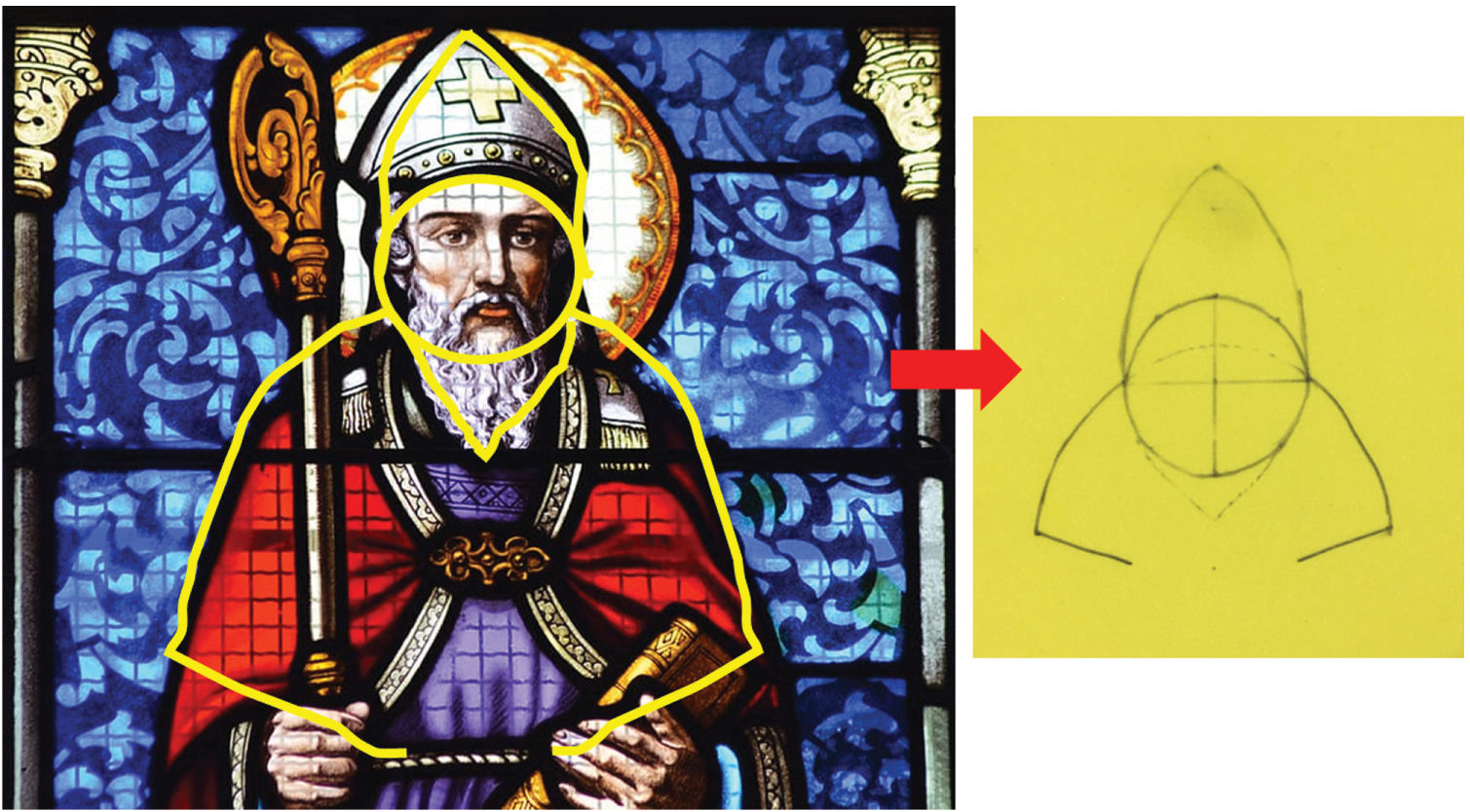
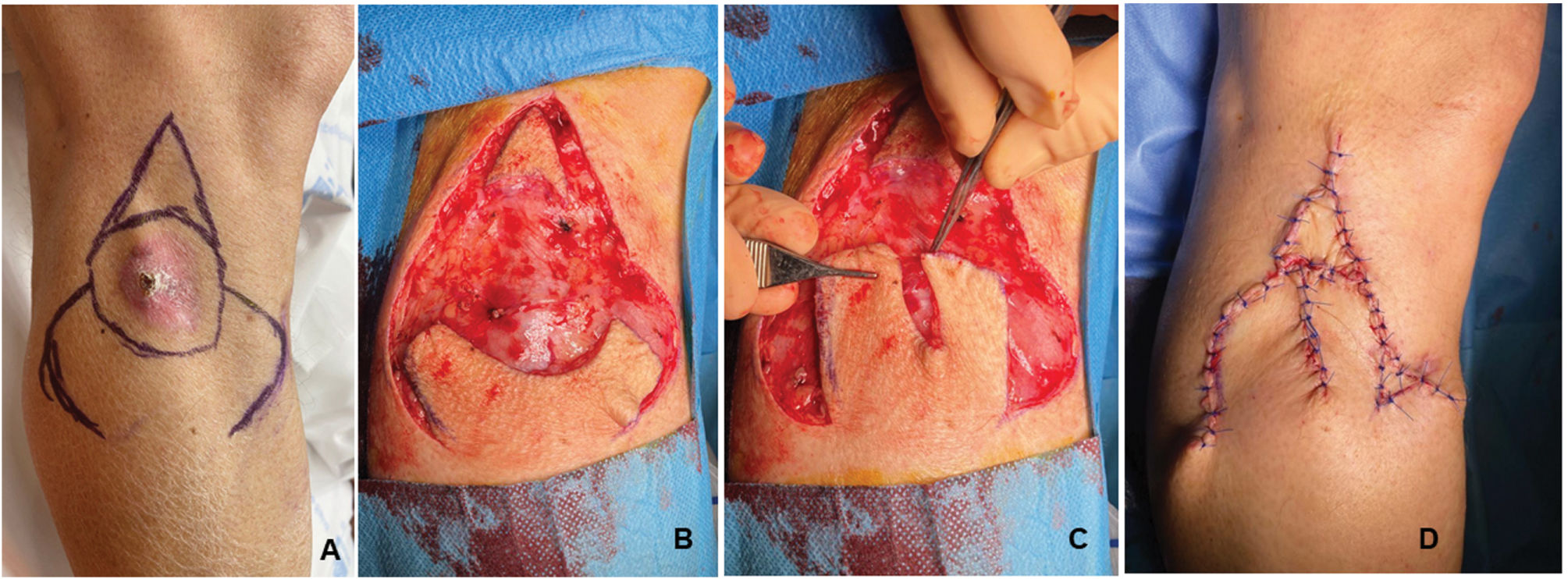
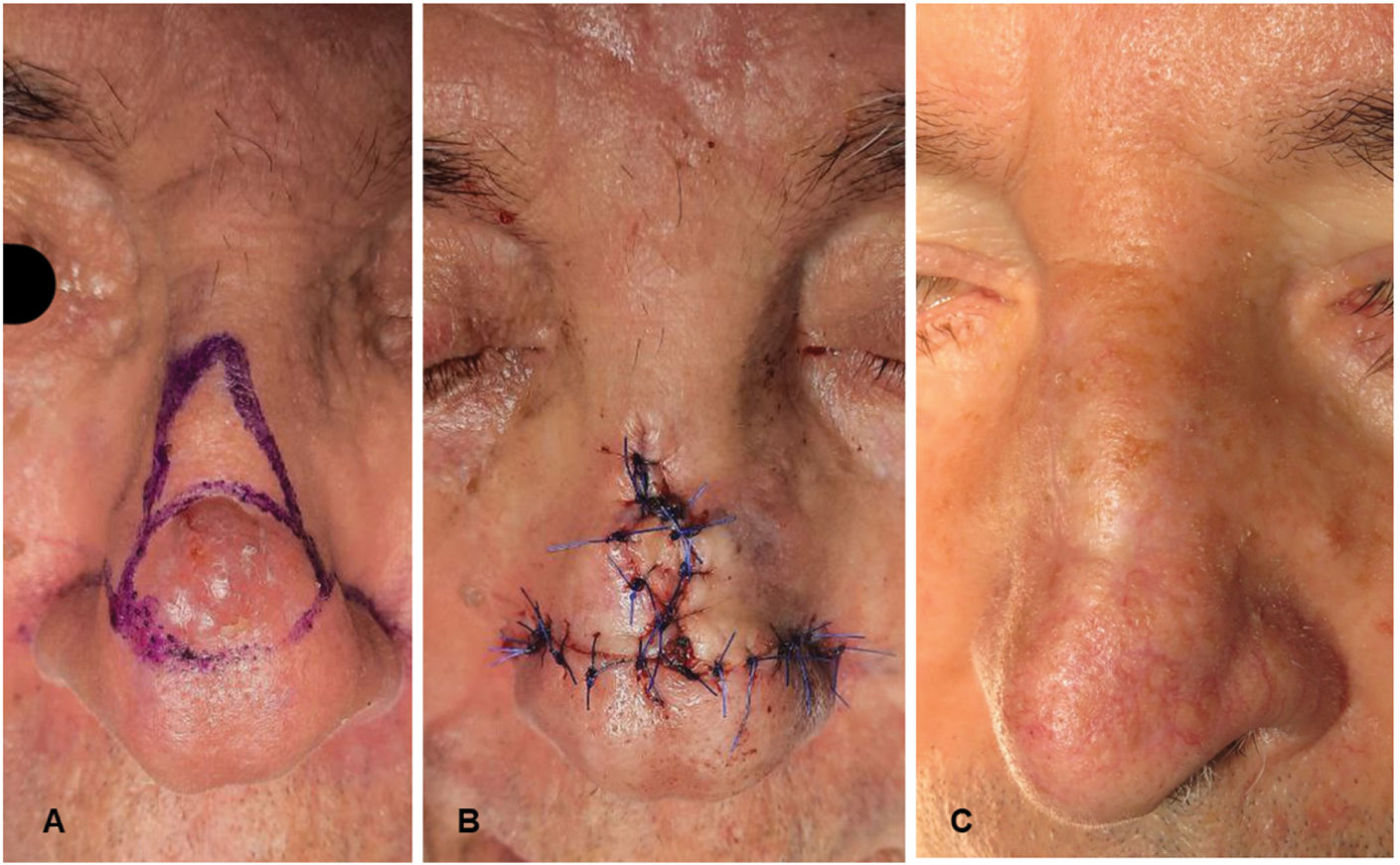
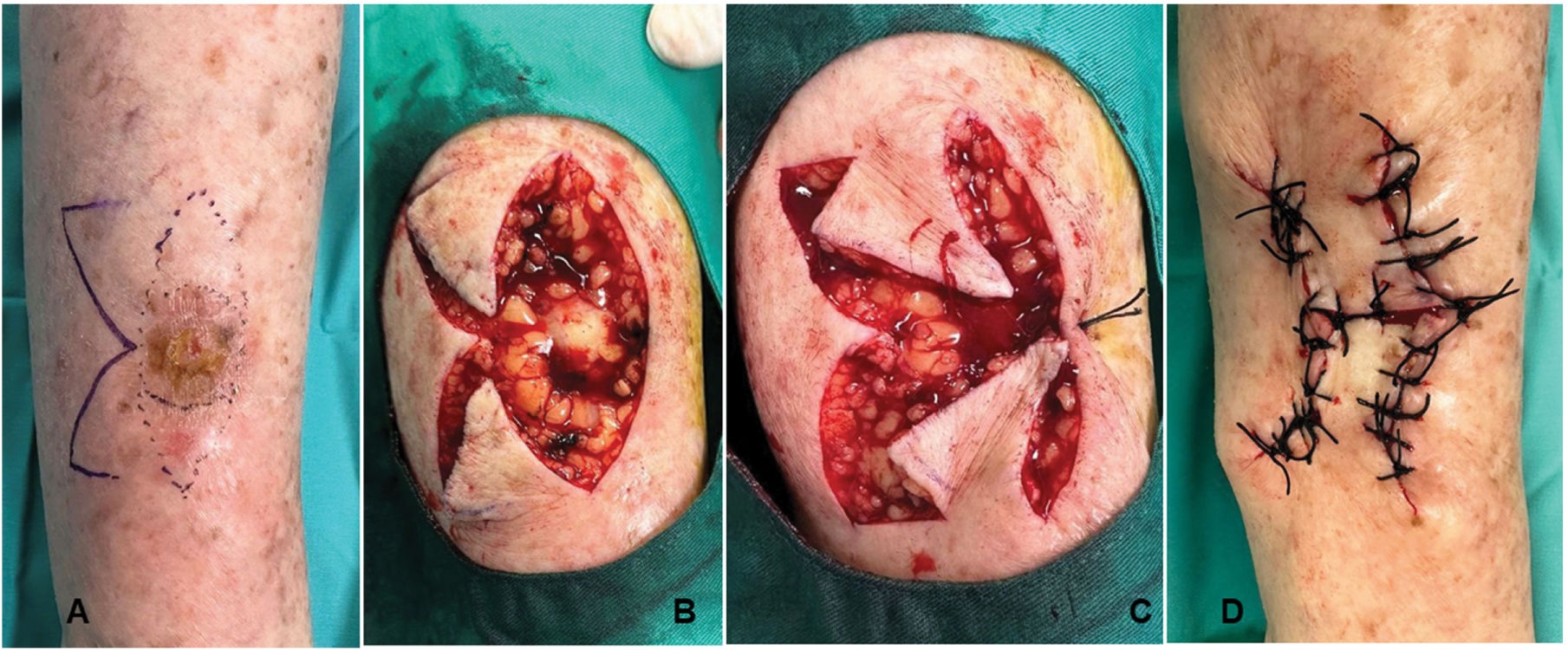
Bishop flapOn a circular defect (Fig. 1), 1 triangular-shaped island flap on top and 2 lateral axe-shaped flaps are designed. At the lower pole of the circular defect, a Burow's triangle is removed. The flap is figuratively named “bishop flap” because the shape of the graft resembles its silhouette, which helps remember the design in the early learning stages.
The subcutaneous pedicle island flap is moved downward to cover the upper half of the defect, and the 2 axe-shaped flaps are rotated laterally to close the other lower half of the defect, aided by the prior removal of the Burow's triangle (Figs. 2–4).
(A) Design of the bishop flap in a patient with squamous cell carcinoma on the leg. (B) Excision of the lesion along with the incision of the flaps. (C) Lateral displacement of the 2 axe-shaped rotation flaps. (D) The island flap is initially moved, and the remaining defect is closed with the 2 lateral axe-shaped flaps.
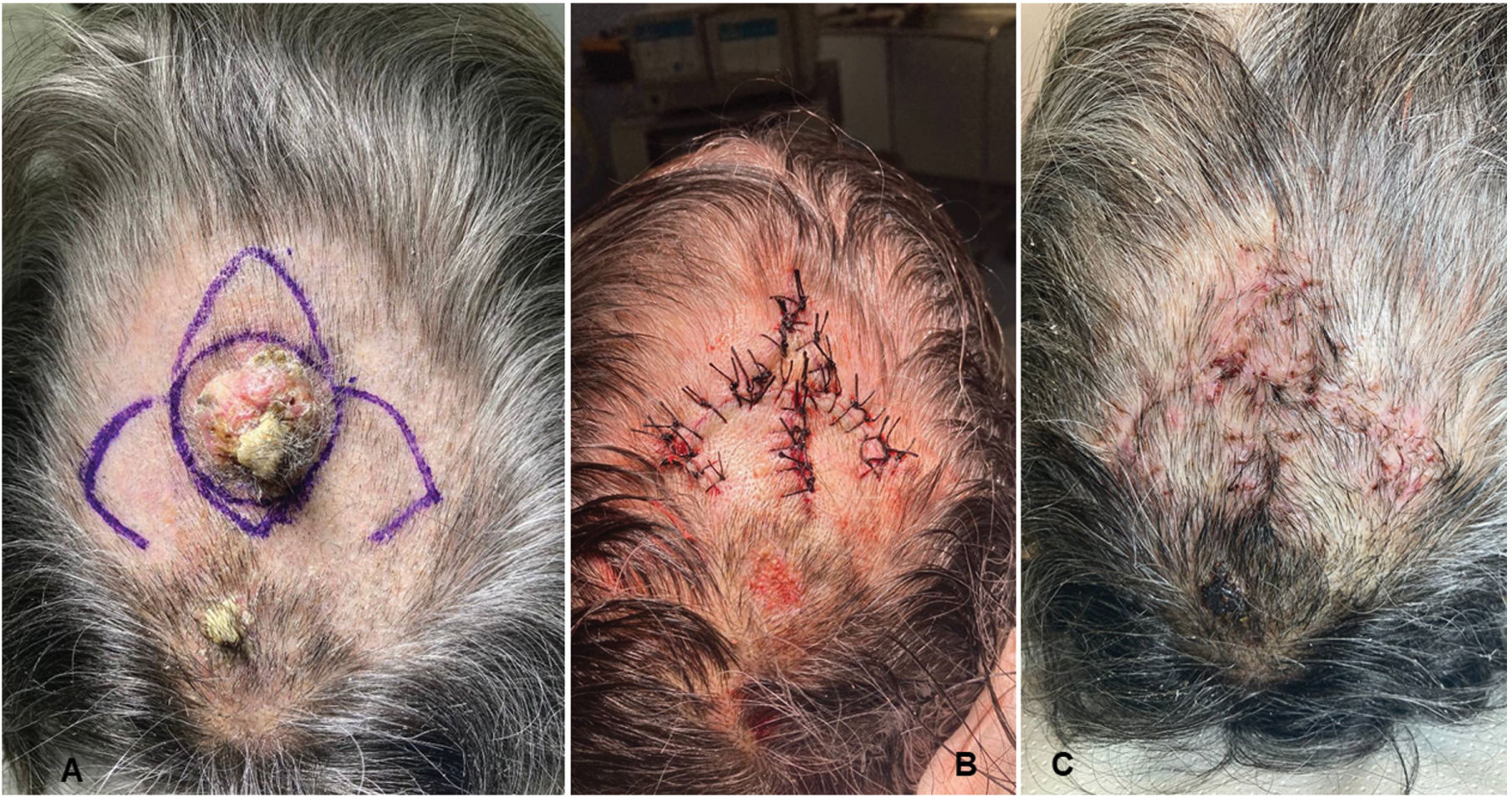
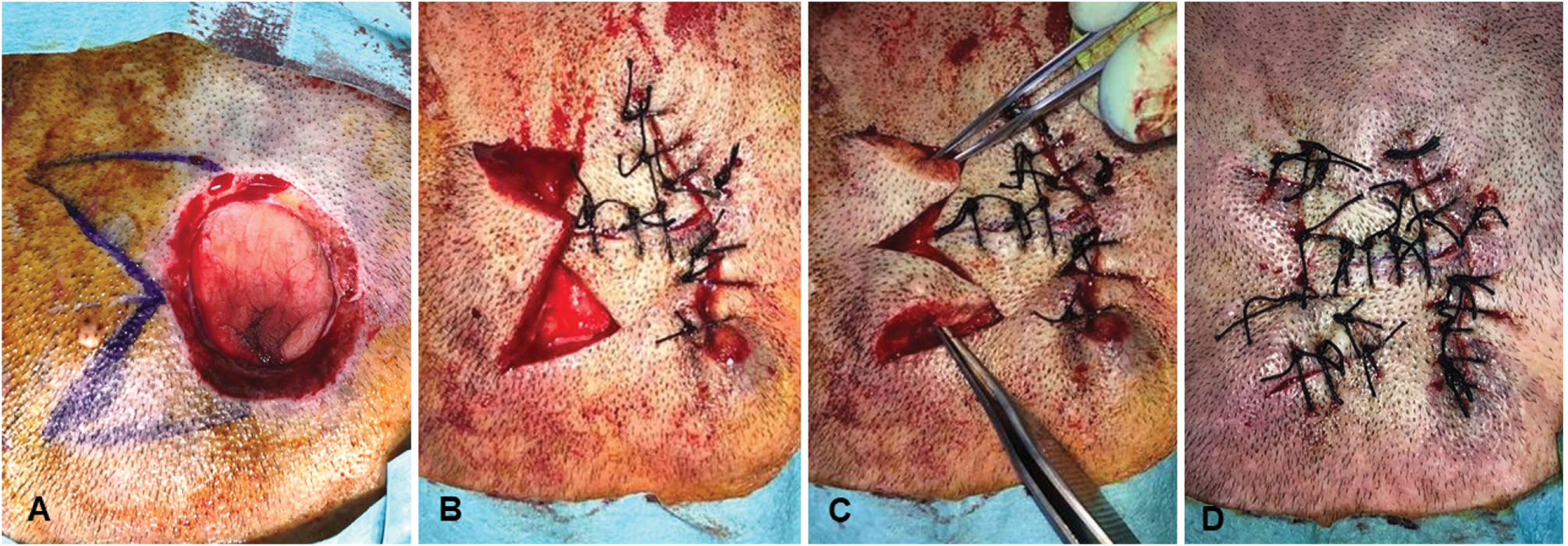
On a circular defect, the classic fusiform shape is drawn, and on one of the sides, a capital letter sigma is traced, occupying the entire length of the said shape (Fig. 5). Once the 2 flaps are incised in a wedge shape, they are rotated to be sutured, closing the other side of the fusiform shape and bringing them together in the center to form a transverse shape. The secondary defect is closed by laterally displacing the remaining skin from the other side after it has been previously undermined. Occasionally, to facilitate the final lateral displacement of the remaining skin, it is split in 2, allowing for a better fit of the flaps to achieve the final closure of the defect (Fig. 6).
(A) Design of the sigma flap in a circular defect on the scalp. (B) Rotation of the 2 axe-shaped flaps and suturing on the contralateral side and transversely in the center of the defect. (C) Split of the remaining lateral skin into 2 parts to fit into the secondary defect. (D) Final suturing.
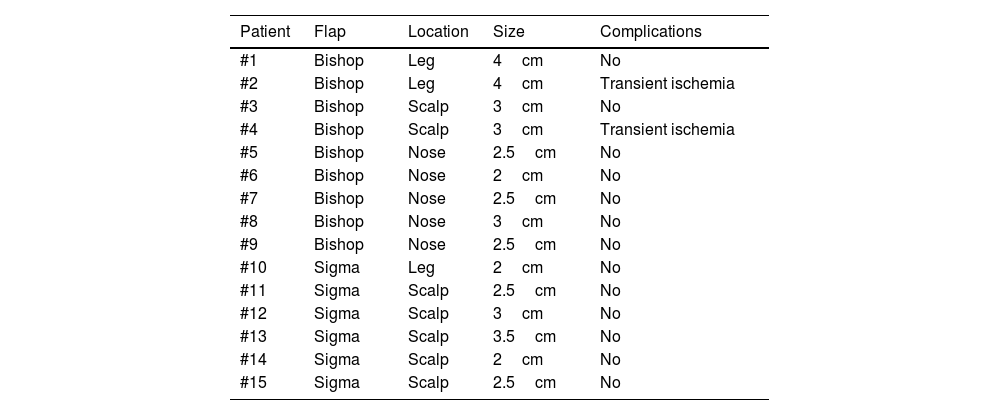
The results are shown in Table 1.
Flaps performed, location, size, and complications during follow-up.
| Patient | Flap | Location | Size | Complications |
|---|---|---|---|---|
| #1 | Bishop | Leg | 4cm | No |
| #2 | Bishop | Leg | 4cm | Transient ischemia |
| #3 | Bishop | Scalp | 3cm | No |
| #4 | Bishop | Scalp | 3cm | Transient ischemia |
| #5 | Bishop | Nose | 2.5cm | No |
| #6 | Bishop | Nose | 2cm | No |
| #7 | Bishop | Nose | 2.5cm | No |
| #8 | Bishop | Nose | 3cm | No |
| #9 | Bishop | Nose | 2.5cm | No |
| #10 | Sigma | Leg | 2cm | No |
| #11 | Sigma | Scalp | 2.5cm | No |
| #12 | Sigma | Scalp | 3cm | No |
| #13 | Sigma | Scalp | 3.5cm | No |
| #14 | Sigma | Scalp | 2cm | No |
| #15 | Sigma | Scalp | 2.5cm | No |
A total of 15 patients were included, 3 women (20%) and 12 men (80%), aged between 42 and 86 years, with a median age of 71 years. The main diagnosis of the excised lesion was squamous cell carcinoma (53%) mainly located on the scalp and legs, followed by basal cell carcinoma (40%) mainly located on the nasal pyramid and 1 case of melanoma (7%) on the leg. The largest diameter of the defect went from 2cm up to 4cm—with a mean of 2.8cm—while the defect area went from 0.15cm2 up to 8.6cm2, with a mean area of 2.54cm2.
The bishop flap was used in 9 patients, 5 of whom had the lesion located on the nasal pyramid, 2 on the legs, and 2 on the scalp. The sigma flap was used in 6 patients, 5 of whom had lesions on the scalp and 1 on the leg. Histological analysis of the specimens showed no involvement of the surgical margins in any of them.
No dehiscence phenomena were reported in the course of the flaps, and only 2 cases of signs of transient ischemia were observed, which resolved uneventfully. The esthetic result of the scar was excellent in all cases, and no recurrences of the excised lesions were detected in any of the patients, with a median follow-up time of 11 months (range, 4–18 months). Supplementary data show the 6-month result of the sigma flap on the scalp of one of the patients (case #15).
DiscussionFew articles in the literature investigate new skin flaps, despite the need for alternatives in complex areas. This is the case of anatomical regions with high basal tension, such as the scalp, lower extremities, and the nasal pyramid, where most classic flaps that work in other areas present problems of ischemia and necrosis due to tension closure.
The measurement of the tension generated at the sutured edges of a flap is extremely important because it is directly related to the ischemia it causes and, ultimately, to the likelihood of necrosis of that flap. In previous studies, we developed a digital tensiometer1 and compared this tension measurement with vascular flow using a laser speckle contrast imaging device. These objective measurements of tension and vascular flow were used to compare various classic flaps with each other, as well as with new flaps.2–4
We have explored different reconstructive options in these high-tension locations such as the scalp: the “1–2-3 rule”,5 the V-Y flap6 tension-relieving incisions,7 or the windmill flap.8
Continuing with this line of research, we have developed these 2 new flaps—the bishop flap and the sigma flap—with the intention of assessing their utility in complex areas with high basal tension.
There are flaps that have proven to be useful and safe in the scalp, such as the O-Z flap.9,10 However, to achieve good mobilization of the flaps and tension-free closure, it is necessary to design large flaps with extensive prior dissection, which carries a risk of bleeding and a final large scar. Regarding the lower extremities, the Keystone flap11 has also proven to be very useful in recent years, but it requires deep dissection down to the muscle fascia and, in some cases, including fasciotomy. This makes it a more complex and delicate flap due to the possibility of damaging deep nerve and vascular structures.
The retrospective study on these 15 patients, in whom the bishop flap and sigma flap were used, has shown that these are safe and viable flaps, achieving appropriate levels of tension and vascular flow. We have decided to publish these 2 flaps together because they share the particularity of achieving low closure tensions, allowing their use in areas of high basal tension such as the scalp, legs, or nasal pyramid.
One advantage over classic flaps is that these are simpler flaps, require less superficial and deep dissection and a smaller amount of surrounding tissue needs to be moved, which eventually results in a smaller scar.
Regarding other options used on the scalp, legs, or nasal tip such as grafting or secondary intention closure, it is important to consider that the esthetic results of grafting are sometimes inadequate. The color and texture of the graft skin are different from those of the surrounding skin, and sometimes the graft surface sits below the surrounding skin, giving an esthetically undesirable sunken patch appearance. In the case of secondary intention closure, the longer healing time involves discomfort and wound care for weeks.
In the past, flaps were named after the first author who described them, but that system has become obsolete. Based on the classification of flaps by the type of movement they produce, the bishop flap would be a combination of a subcutaneous pedicle island flap plus 2 lateral axe-shaped rotation flaps. However, the current trend is to use figurative names, as they are easier and help in remembering the flap design during the early learning phases, such as the “reading man” flap.12 In the case of the bishop flap, drawing it reminiscent of a bishop with his miter (subcutaneous pedicle island flap on top), beard (lower Burow's triangle), and shoulders (2 lateral axe-shaped rotation flaps), greatly facilitates the final design. Similarly, the sigma flap is named as such because the design is easier to remember by drawing the capital sigma letter on one of the lateral edges of the fusiform shape required in this type of flap.
When these theoretical flap designs were tested on foam rubber and pig skin, we found some technical details that improved the final results. Regarding the bishop flap, we found it most useful to start by lowering the triangular subcutaneous pedicle island flap. The area of the defect that it will cover is, in most cases, just the upper half, while in other instances, it may cover the entire defect, making the creation of the lateral axe-shaped flaps unnecessary. This would turn the bishop flap into a useful secondary alternative to any subcutaneous pedicle island flap that does not fully cover the defect. It is advisable to create the lateral axe-shaped flaps after the island flap has been displaced, as the “shoulders” should be designed precisely at the lower point reached by the island flap as it moves downward. The size of these lateral flaps will also depend on this lower point, in such a way that if the remaining surgical defect to be covered is smaller, the size of the lateral flaps will be proportionally smaller too. When we used the bishop flap on the nasal pyramid, a few changes to the original design were also made due to the anatomical particularities of the area. If possible, the incisions of the lateral axe-shaped flaps should be placed over the nasolabial folds, so that the subsequent scar is better concealed within these natural creases. When rotating these 2 lateral flaps, the island flap should be trimmed at its lower angles to ensure a proper fit and facilitate a perfect closure. The adaptation of the bishop flap to the nasal pyramid ends up turning the closure of an initially triangular wound into a curvilinear scar.
Regarding the sigma flap, surgical practice on several patients has shown us that once the 2 flaps are rotated and sutured to one edge of the fusiform shape required, in some cases splitting the remaining skin on the other side of the spindle into 2 parts may help so that it fits perfectly into the secondary defect.
To avoid ischemic complications and necrosis, it is important to stick to the design of the bishop and sigma flaps, as the rotation pedicle of both flaps is already narrow in the original design.
The good results obtained with both flaps in a series of patients with tumor lesions in anatomically complex areas with high tension encourage us to use them in future studies in other complex locations such as the sole of the foot or fingers. Moreover, if these flaps have proven to be safe in complex areas, it is evident that they can be reliably used in other anatomical areas with lower basal tension or better vascularization.
ConclusionsThe bishop flap and sigma flap are 2 good reconstructive options for surgical defects located in complex areas of high tension, such as the scalp, lower extremities, or nasal pyramid. They have proven to be safe by achieving closure with less tension and without inducing ischemia or necrosis. Additionally, they have the advantage over classic options of not requiring as much tissue dissection at superficial or deep level, resulting in smaller scars.