The nose is a common site for skin tumors. The main arteries that supply the nose extend through the subcutaneous tissue. Submuscular dissection facilitates the design of safe, reliable musculocutaneous flaps that adapt well to the morphology of nasal defects. The diversity of these flaps makes them the first choice for reconstructing defects in more complex regions, such as the inner canthus of the eye and the nasal ala. We describe the surgical design of the procerus, V-Y nasalis, and lateral wall nasalis musculocutaneous flaps used to repair defects following tumor excision. The descriptions are illustrated by photographs taken by the authors during procedures and in cadaveric dissections.
La nariz es una localización habitual de asiento de tumores cutáneos. Las arterias principales que vascularizan la nariz discurren en el espesor del tejido celular subcutáneo. La disección en el plano submuscular permite diseñar colgajos musculocutáneos fiables y seguros, adaptados a la morfología del defecto. Su gran versatilidad los convierte en colgajos de primera elección para la cobertura de defectos ubicados en localizaciones más complejas, como el canto interno del ojo o el ala nasal. Presentamos la técnica quirúrgica de los colgajos musculocutáneos procerus, nasalis de morfología V-Y y colgajo nasalis de pared lateral empleados tras exéresis tumorales. La descripción se acompaña de imágenes realizadas por los autores en pacientes y en disecciones cadavéricas para la mejor comprensión de dichos colgajos.
The nose is a common site for skin tumors. Surgeons should therefore be familiar with reconstruction of defects arising from excision of nasal tumors. The choice of which reconstruction technique to use should follow 3 basic principles, with the aim of achieving good esthetic and functional outcomes.
- 1.
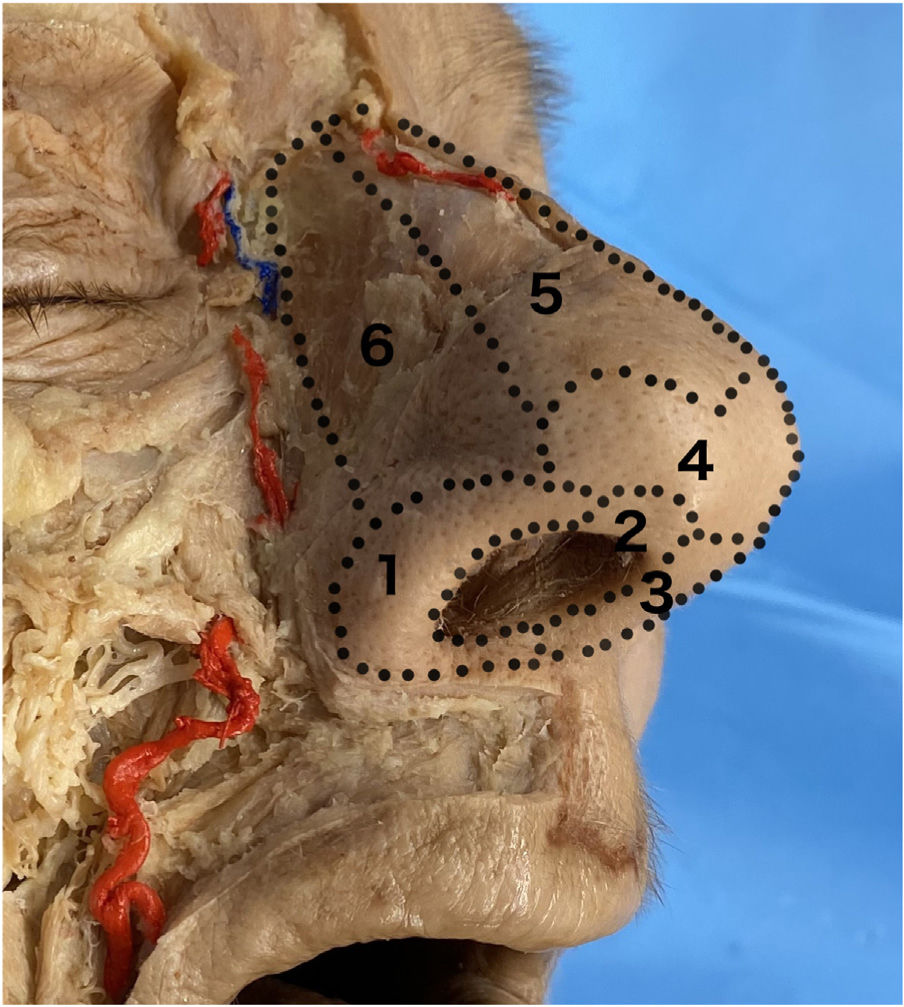
Principle of esthetic subunits: The nose comprises 9 esthetic subunits—nasal dorsum, nasal walls, nasal alae, the tip of the nose, the columella, and soft triangles (Fig. 1). Skin flaps should be designed as far as possible within the subunit where the defect is located, attempting to avoid crossing to neighboring subunits. It is recommended to make incisions at the borders between these subunits to leave less noticeable scars.1
- 2.
Reconstruct “like with like”: It is recommended to retain the qualities and outline of the absent subunits with tissues that resemble them as closely as possible. For this, in defects measuring more than 8–10mm, it is preferable to use local plasties instead of graft or closure by second intent. Local flaps better preserve the characteristics of the resected area.2
- 3.
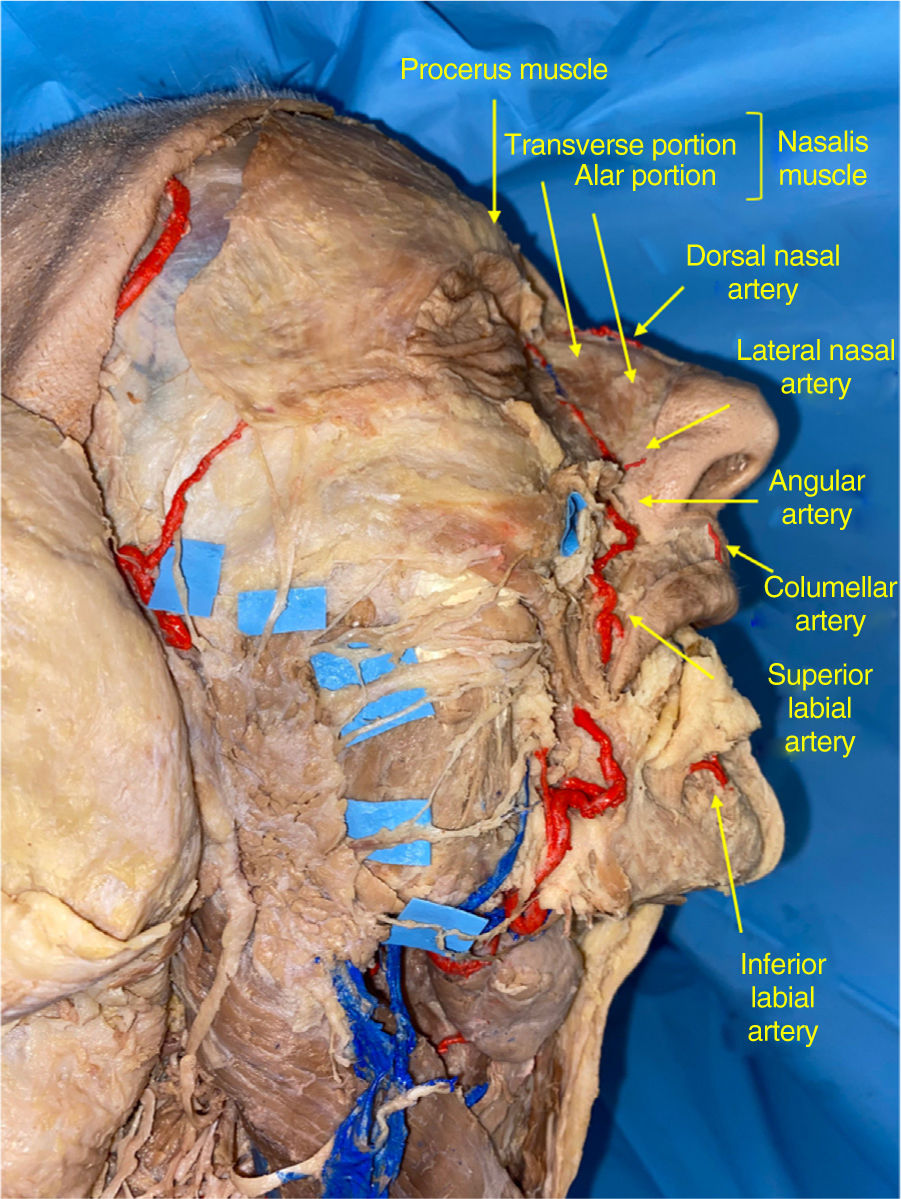
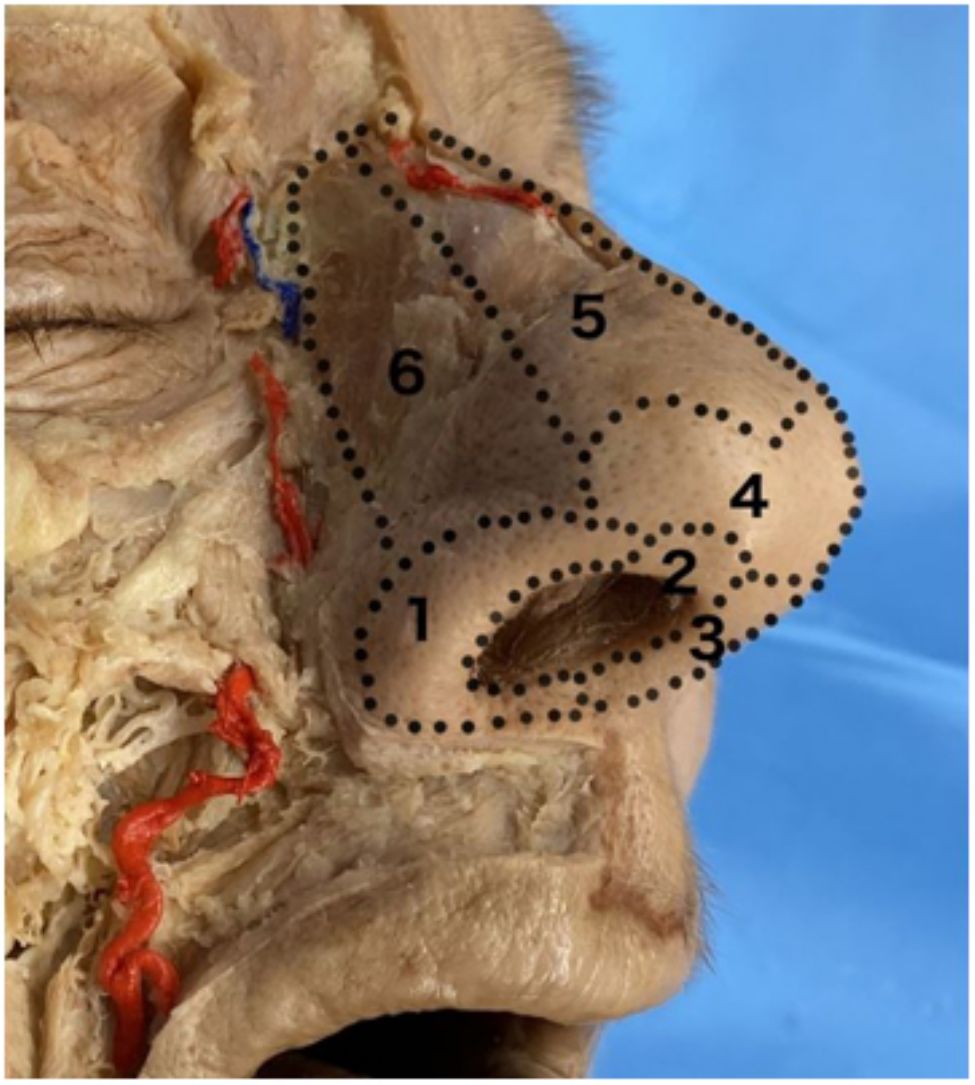
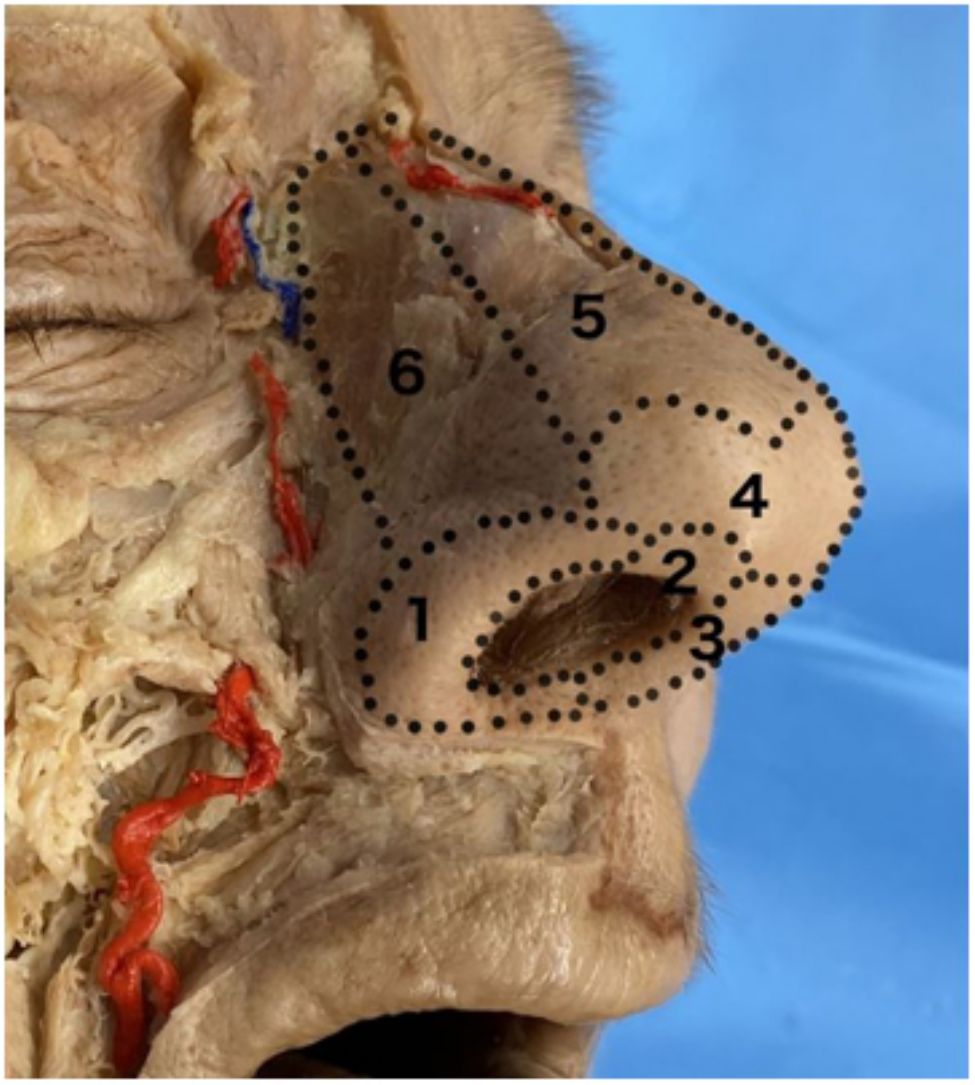
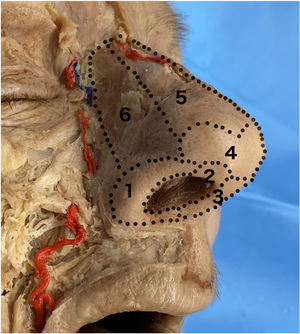
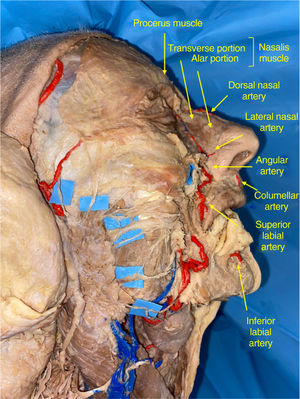
Principle of preservation of nasal vasculature: The nose has a 3-dimensional structure comprised of 4 superimposed planes: the skin, subcutaneous fatty tissue, the musculoaponeurotic plane, and the osseocartilaginous skeleton. The main artery branches that irrigate the nasal pyramid extend through the subcutaneous cell tissue, above the muscular plane (Fig. 2). Dissection in the submuscular plane is more conservative with vascularization of the nasal flaps. Therefore, smaller flaps can be designed and adapted to the morphology of the defects in more complex sites, such as the inner canthus of the eye or the nasal ala.3
Figure 2.Anatomic dissection by the authors in which the 2 main sources of irrigation of the nasal pyramid are identified: dorsal artery of the nose from the ophthalmic artery and the angular artery and its branches from the facial artery. The divisions of the facial nerve are highlighted with contrast.
The literature includes a wide variety of local skin flaps for reconstruction of nasal defects.4–8 However, there are few publications that highlight the importance of musculocutaneous flaps. The aim of the present article is to describe the surgical technique and main indications for procerus flaps, nasalis flaps, and lateral wall nasalis flaps in nasal reconstruction, with cadaveric dissection as an aid to understanding.
Procerus perforator flapAnatomyThe procerus perforator flap is a V-Y island advancement flap that incorporates skin, subcutaneous cell tissue, and the procerus muscle. It is irrigated by the dorsal nasal artery, a branch of the ophthalmic artery9 (Fig. 2).
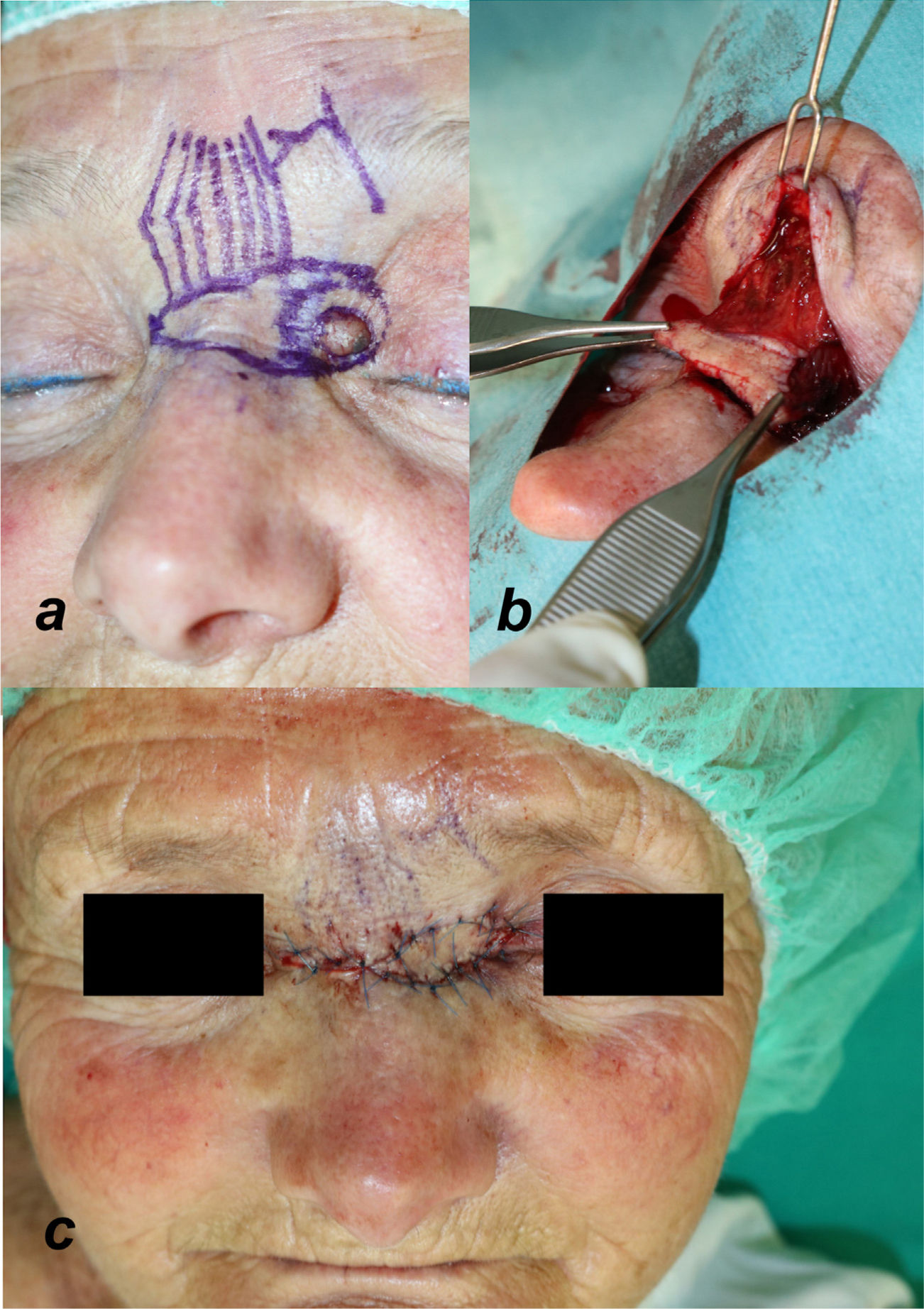
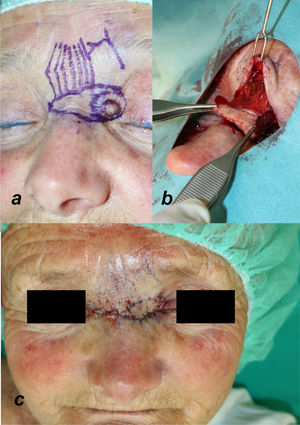
Technique for obtaining the flapUnder local anesthetic, a cutaneous island flap is designed of the same size as and medial to the defect, located on the nasal dorsum (Fig. 3a). The caudal incision of the flap is made down to the periosteum, followed by blunt dissection in the cephalic direction below the procerus muscle. The artery branches extend through the subcutaneous cell tissue, between the procerus muscle and the skin. Therefore, dissection below the muscle plane guarantees blood supply. The cranial incision is made until reaching the muscle plane, enabling greater blood supply (Fig. 3b). Exposing the pedicle of the flap is not necessary and may compromise its viability. To obtain greater mobility, the pedicle can be dissected horizontally with scissors close to both medial canthi. Once dissection is complete, the flap is advanced toward the defect without tension and held in place with subcutaneous resorbable sutures and nonresorbable percutaneous sutures. The defect in the donor area is closed with a V-Y pattern (Fig. 3c).
Illustration of the different steps for designing and detaching the procerus perforator flap. (a) Flap design. The direction of the procerus muscle fibers and the outflow of the supratrochlear artery are marked on the skin. (b) Dissection and detachment of the flap below the muscle plane. (c) Advancement and closure of the V-Y defect.
The procerus flap enables reconstruction of superficial defects of up to 2cm located in the proximal nasal wall and inner canthus of the eye.3 By using the procerus muscle, it is possible to achieve better advancement than with conventional V-Y flaps. The muscle component also adds a greater volume to the defect if required. It has an advantage compared with other conventional flaps, such as the glabellar flap, that the donor skin is of similar characteristics to that of the missing tissue, and so the esthetic outcomes are satisfactory.10 In addition, as there is no tension at the advancement front, the risk of displacement of neighboring structures, such as the eyebrow or lower eyelid, is avoided; these are drawbacks of advancement or revolving-door flaps of the cheek or nasal dorsum.
Nasalis musculocutaneous V-Y flapAnatomyThe nasalis musculocutaneous V-Y flap is a flap that includes skin, subcutaneous cell tissue, and the alar portion of the nasalis muscle. It has axial vascularization via the lateral nasal artery, a branch of the angular artery (Fig. 2).11
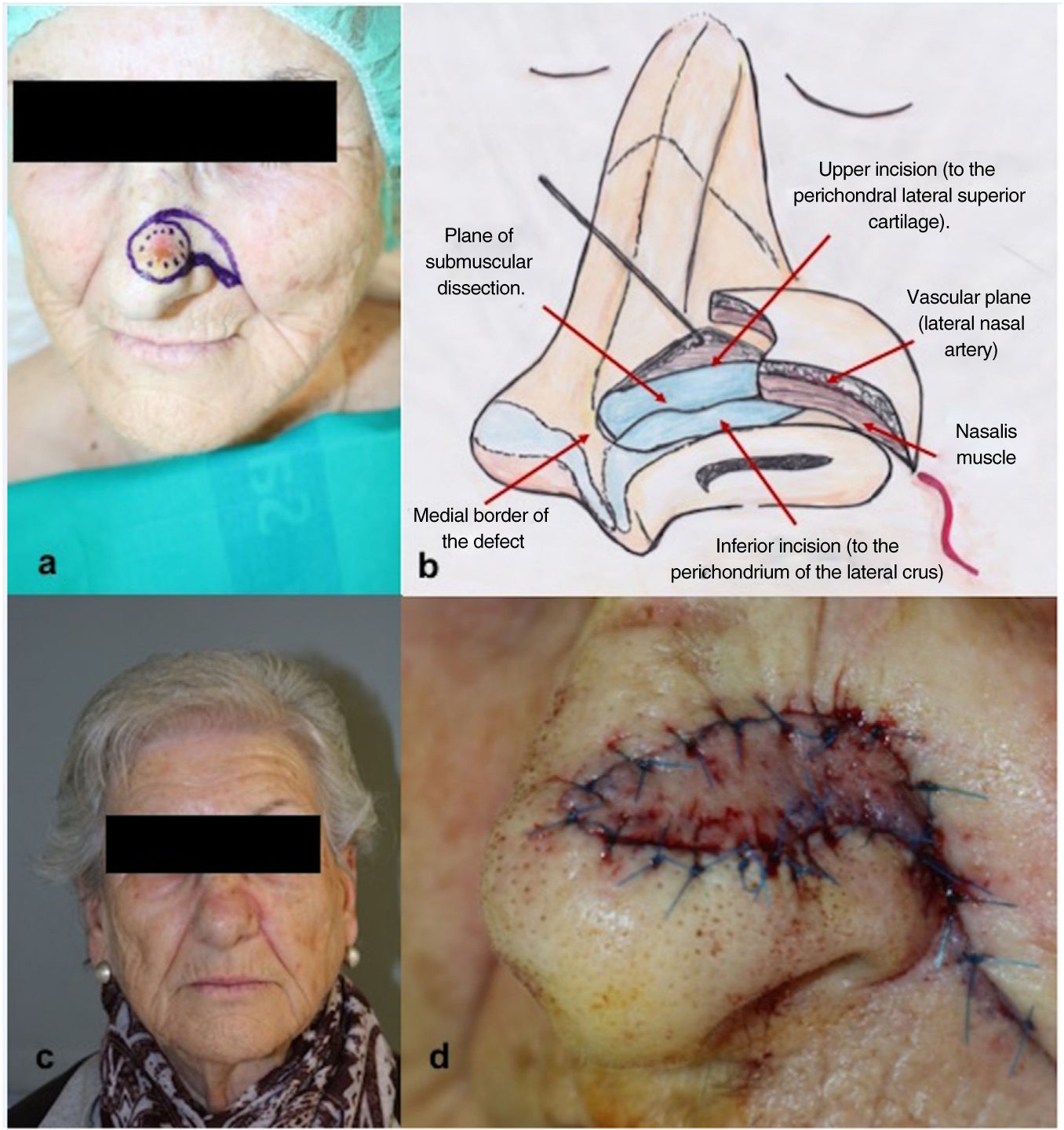
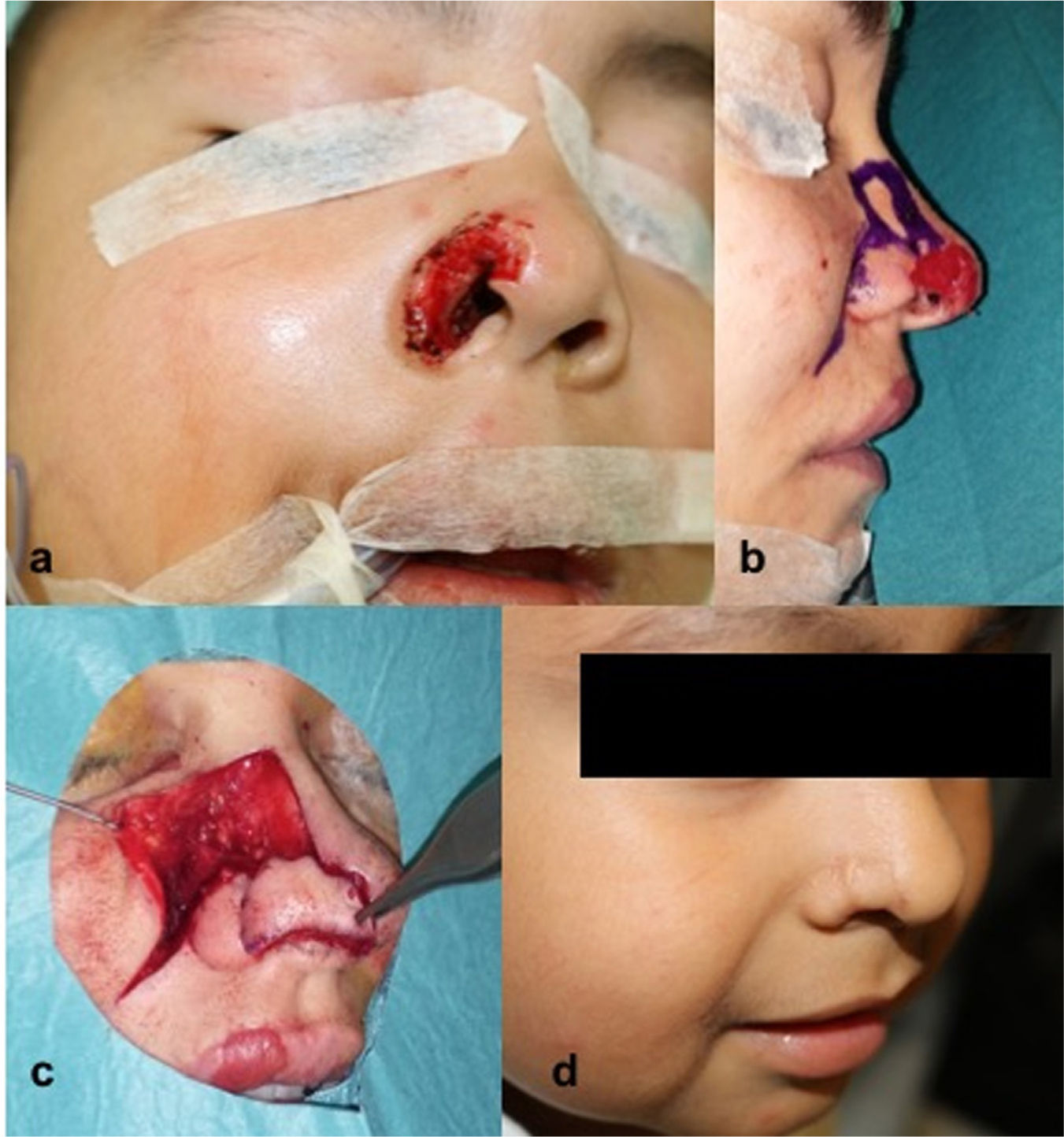
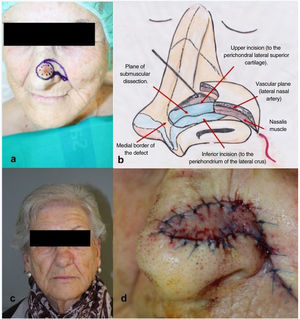
Technique for obtaining the flapUnder local anesthetic, a triangular flap is designed, whose base coincides with the superomedial border of the defect and the apex is positioned laterally (Fig. 4a). The lower border is located in the alar groove and the upper border extends from the defect in a lateral direction until reaching the lower border of the pattern. The height of the flap has to be the same as that of the defect. The lower border is then cut until reaching the perichondrium of the lateral crus (Fig. 4b). The upper cutaneous incision can be made via the skin and subcutaneous tissue or, if a larger advancement is needed, the cut is made through the nasalis muscle until reaching the perichondrium of the upper lateral cartilage. The borders of the flap are then released by blunt dissection in the subcutaneous plane. Dissection of the lateral border of the flap has to be done carefully to preserve the superior alar artery, located close to the alar base. With the help of a hook, the medial border of the flap is raised and carefully detached from the fibrocartilaginous base, below the nasalis muscle, until the desired advancement is achieved (Fig. 4b). Once the dissection is completed, the flap is held in place with resorbable subcutaneous suture and nonresorbable percutaneous suture. The defect in the donor area is closed with a V-Y pattern (Fig. 4d).12
IndicationsThe nasalis musculocutaneous flap enables reconstruction of superficial defects of up to 1.5cm, located on the distal nasal wall, where the tip and nasal ala meet. Unlike the bilobulated flap, there is no risk of obliteration of the alar groove, the dorsal vascularization of the nose is respected, dissection is less extensive, and some of the scarring is hidden in the alar groove.13 The esthetic and functional outcomes are therefore satisfactory.
Lateral wall nasalis flapAnatomyThe lateral wall nasalis flap is a revolving door island flap that includes skin, subcutaneous cell tissue, and the transverse part of the nasalis muscle. It has an axial vascularization from the lateral nasal artery, a branch of the angular artery (Fig. 2).14
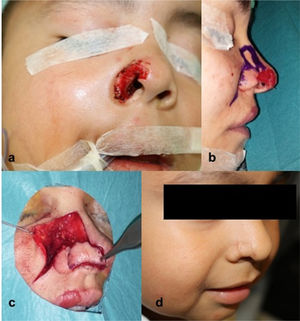
Technique for obtaining the flapA cutaneous island is designed above the defect, with larger dimensions than this, on the lateral nasal wall. In most cases, the lower border is designed following a tangential extension to the upper border of the defect in superomedial direction. The remaining borders are drawn, adapting to the morphology of the defect (Fig. 5b). The flap is dissected in the cephalocaudal direction from the medial border, below the transverse portion of the nasalis muscle. When the muscle has been raised, an incision is made in the skin of the lateral border until the cutaneous island is complete. The flap is rotated 90–180° to bring it to the primary defect (Fig. 5c). The secondary defect generated in the donor area is closed by an advancement flap of skin from the cheek.
Illustration of the surgical technique of the lateral wall nasalis musculocutaneous nasal flap. (a) Excision of the lesion from the right nasal ala with partial removal of the soft triangle. (b) Design of the flap adapted to the morphology of alar ridge. (c) Rotation of the flap over the vascular pedicle. (d) Postoperative outcome after 21 days.
The lateral wall nasalis flap allows reconstruction of small and medium-sized defects located in the lower third of the nose, particularly those on the nasal ala. Small modifications to the flap allow the defects on the tip and nasal soft triangle to be reached. Unlike the nasolabial flap, which requires 2 sessions, the lateral wall nasalis flap allows alar defects to be reconstructed in a single intervention, without the risk of obliteration of the nasolabial fold, conserving the dorsal vascularization of the nose.14,15
ConclusionsMusculocutaneous flaps are a useful tool in the reconstruction of small- and medium-sized nasal defects. These are reliable and safe flaps, thanks to the incorporation of a muscle component. They can be designed by adapting to the morphology of the defect. Their great versatility makes them the flap of choice for covering defects located in more challenging sites, with good esthetic and functional results. The procerus flap is indicated for covering defects of the upper third of the nasal pyramid and inner canthus. Their design avoids displacement of neighboring structures such as the lower eyelid or eyebrow as closure is achieved without tensing the donor area. For reconstruction of defects in the lower third, we could use the nasalis musculocutaneous V-Y flap and the lateral wall nasalis flap. The former is indicated for defects of the nasal tip. The latter enables, in a single intervention, defects of the nasal ala to be reconstructed without risk of obliterating the nasolabial fold.
FundingThis study did not receive any funding.
Conflicts of interestThe authors declare that they have no conflicts of interest.