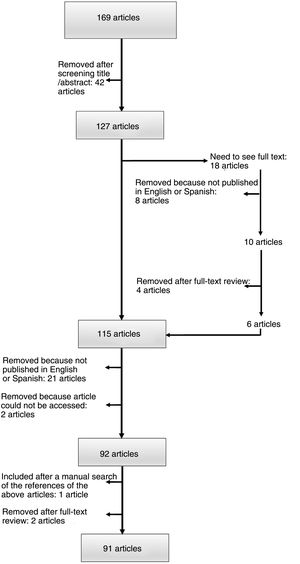
Acne fulminans is a severe and rare form of inflammatory acne. Lesion severity and subsequent scarring has a negative impact on the patient's quality of life. We conducted a narrative review of the literature on acne fulminans based on a search for relevant English- and Spanish-language articles published in Medline. We included case reports and case series. The main aim was to describe the clinical and demographic characteristics of patients with acne fulminans. A secondary aim was to determine whether quality of life was affected by the site or extent of lesions. We reviewed 91 articles describing 212 cases of acne fulminans. The mean age of the patients (91.94% male) was 16.6 years. A personal and family history of acne vulgaris was reported for 97.63% and 54.90% of patients, respectively. A trigger was identified in 44.79% of cases. The main cause was pharmacologic (96.63%) and the main drug isotretinoin (65.28%). The sites most often affected were the face (89.31%), the posterior trunk (77.86%), and the anterior trunk (74.81%). The predominant disease subtype was acne fulminans with systemic symptoms (59.12%), which were mostly general (97.06%). Systemic corticosteroids were the most widely used treatment (81.03%). The impact of the disease on quality of life was reported for two patients. In conclusion, acne fulminans mainly affects the face and trunk of male adolescents with a history of acne vulgaris. The main subtype was acne fulminans with systemic symptoms, and most patients were treated with systemic corticosteroids. The effect of acne fulminans on quality of life is under-reported.
El acné fulminans (AF) es una forma rara y grave de acné inflamatorio. La intensidad de las lesiones cutáneas y las cicatrices secundarias impactan negativamente en la calidad de vida. Presentamos una revisión narrativa de casos de AF publicados en Medline. Se incluyeron artículos escritos en lengua castellana o inglesa, que reportasen casos aislados o series de casos de AF, de los que se recogieron variables clínico-demográficas. El objetivo principal de la revisión fue describir las características clínico-demográficas del AF. Secundariamente se pretendió determinar si la localización o la extensión lesional repercuten en la calidad de vida. Se revisaron 212 casos de AF incluidos en 91 artículos (edad media: 16,6 años, 91,94% varones); 97,63% de los pacientes presentaron acné previo al brote de AF y 54,90% contaba con antecedentes familiares de acné. En 44,79% existió un factor desencadenante de AF (98,63% farmacológico: 65,28% isotretinoína). Las localizaciones más habitualmente afectas fueron cara (89,31%), tronco posterior (77,86%) y anterior (74,81%). El subtipo predominante fue el AF asociado a síntomas sistémicos (59,12%). Entre los síntomas sistémicos destacó la sintomatología general (97,06%). El tratamiento más prevalente fue la corticoterapia sistémica (81,03%). La repercusión del AF en la calidad de vida se reportó en dos pacientes. Como conclusiones, el AF predomina en los varones adolescentes con antecedentes de acné vulgar, afectando fundamentalmente la cara y el tronco. La forma más frecuente es el AF con síntomas sistémicos. Para su tratamiento, los corticoides sistémicos son los fármacos más frecuentemente empleados. La repercusión del AF en la calidad de vida está infrarreportada.
Acne fulminans (AF) is a severe and rare form of inflammatory acne that usually presents as an acute flare characterized by painful hemorrhagic pustules and ulcers with or without systemic manifestations (Fig. 1).1,2 Because of its intense inflammatory activity and scarring, it can cause significantly impaired quality of life.2 AF is most common during adolescence, a period in which perceived body image has a key role in the biopsychosocial sphere.3 It is therefore important to assess the impact of this disease on both psychological and social well-being. The main aim of this study was to review the clinical and demographic characteristics of AF. A secondary aim was to investigate whether quality of life is affected by the site or extent of lesions.
Material and MethodsWe conducted a narrative review of the literature on AF in patients with or without an associated autoinflammatory syndrome. We included English- and Spanish-language case reports and series published in Medline-indexed journals. We excluded articles written in a language other than Spanish or English, articles other than case reports or series, basic research studies, and molecular studies, even those that reported on a case of AF. The search was conducted in PubMed (Medline database) using the search terms “acne” [Medical Subject Headings] AND “fulminans” and targeting all articles published up to January 7, 2022. No initial date limit was established.
The articles were selected by first screening the titles and abstracts of all articles retrieved by the search. When it was not clear if the article was a case report or series, the full article was accessed. Articles not dealing with patients with AF were discarded after a full-text review. All articles were reviewed independently by 2 authors (IT and AB), who then met in a face-to-face meeting to resolve any discrepancies.
Information was collected on each article (author, title, journal, year of publication, and number of patients), demographics (age, sex), clinical characteristics (personal history of acne and duration, family history of skin diseases, time since onset of AF, triggers, lesion site, type of lesions, AF subtype, systemic manifestations, presence of fever, erythrocyte sedimentation rate [ESR], leukocytosis, musculoskeletal involvement, radiologic changes, involvement of other organs or systems, and presence of an autoinflammatory syndrome), treatments administered, and impact of AF on quality of life. Quality of life was assessed using information reported for each patient.
The data were entered into an Excel spreadsheet and analyzed in R (version R i386 3.4.2). We calculated the frequency distribution of qualitative variables and the mean (SD) of quantitative variables. Associations between qualitative variables were analyzed using the χ2 or Fisher exact test.
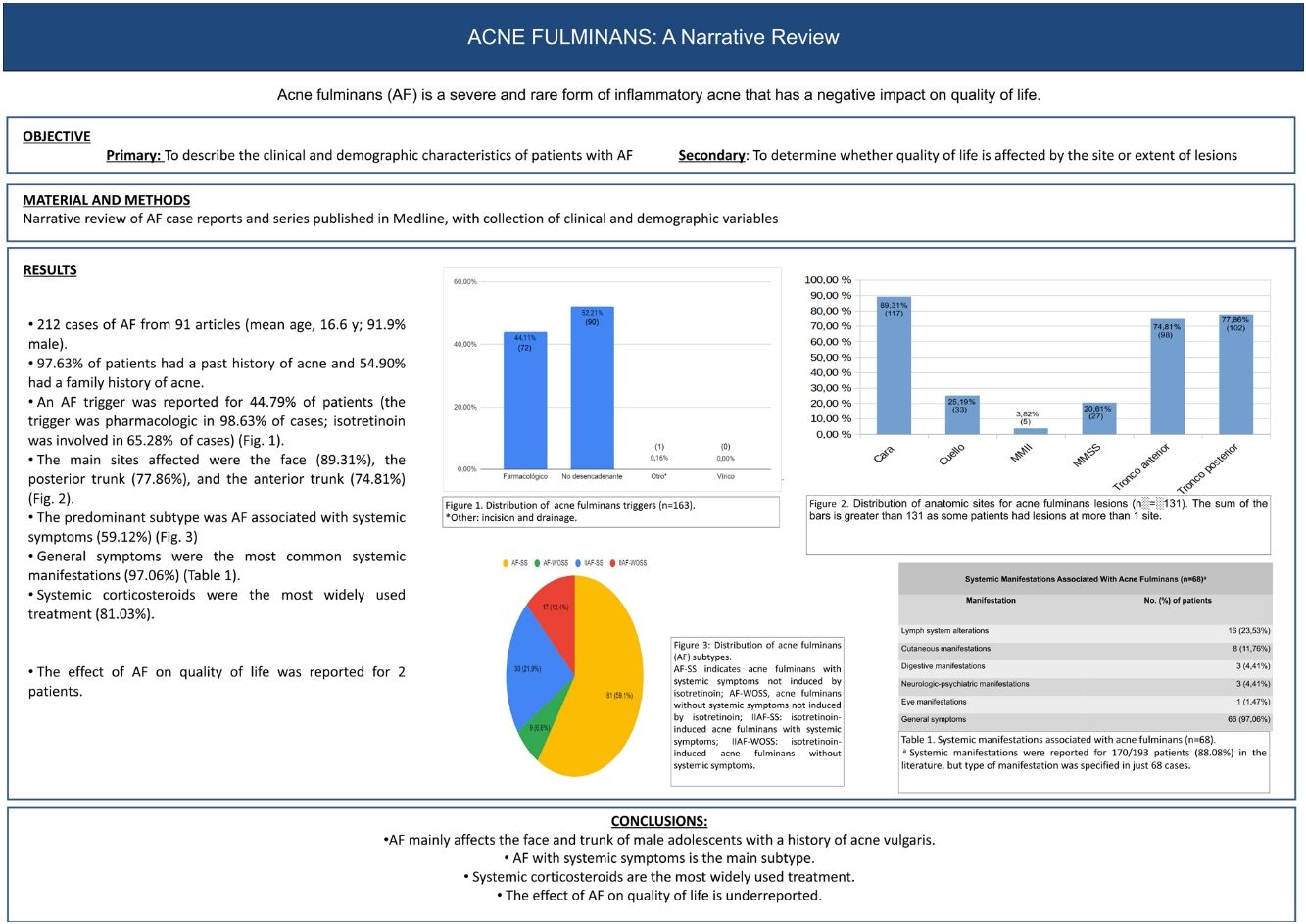
ResultsThe search strategy yielded 169 articles published between 1977 and 2021. The 2 researchers agreed on the initial selection of 79.3% of the articles; 33/169 articles presented discrepancies that required discussion. After discussing the reasons for inclusion or exclusion in a face-to-face meeting, the 2 researchers reached an agreement on all cases. Ninety-one articles were finally included: 74 case reports (1 patient) and 17 case series (≥2 patients) (Fig. 2).
The studies analyzed a total of 212 patients (mean [SD] age, 16.6 [3.63] years; 91.9% male [194/211]). Overall, 165/169 patients (97.6%) had a past history of acne (mean duration, 19.2 [23.4] months) and 14/35 (40%) had had severe acne. A family history of skin disease was mentioned for 29/51 patients (56.9%). Of these 29 patients, 28 (96.6%) had had acne. The most frequently affected family members were siblings (57.9%, 11/19) followed by parents (42.1%, 8/19). Mean time from onset of an AF flare to a physician visit was 4.6 (3.9) weeks.
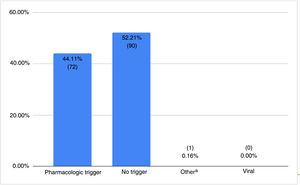
The distribution of AF triggers is shown in Fig. 3. Drugs were mentioned as a trigger in 72/73 patients (98.6%). Isotretinoin was the main drug involved (65.3%, 47/72), followed by tetracycline (16.7%, 12/72).
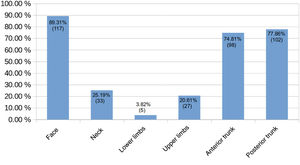
The main sites for AF were the face (89.3%, 117/131), the posterior trunk (77.9%, 102/131), and the anterior trunk (74.8%, 79/131). The other sites are shown in Fig. 4.
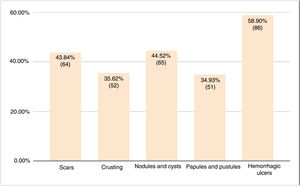
Hemorrhagic ulcers were the most common type of lesion (58.9%, 86/146). The prevalence of the other lesions ranged from 34.9% to 44.5% (Fig. 5).
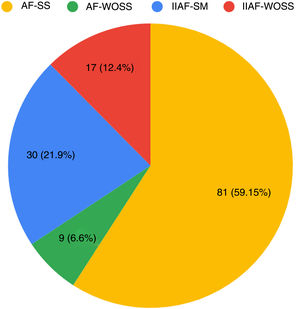
The main subtype of AF was AF with systemic symptoms not induced by isotretinoin (AF-SS) (59.1%, 81/137) (Fig. 6).
Distribution of subtypes of acne fulminans (n=137). AF-SS indicates acne fulminans with systemic symptoms not induced by isotretinoin; AF-WOSS, acne fulminans without systemic symptoms not induced by isotretinoin; IIAF-SS, isotretinoin-induced acne fulminans with systemic symptoms; IIAF-WOSS, isotretinoin-induced acne fulminans without systemic symptoms.
Extracutaneous systemic manifestations were observed in 146/169 patients (86.4%). The manifestations involved a single system in 43/68 patients (63.2%), 2 systems in 22/68 patients (32.4%), and 3 systems in 3/68 patients (4.4%). The most common manifestations were general symptoms (97.1%, 66/68) followed by lymphadenopathy (23.5%, 16/68). The other organs and systems affected are shown in Table 1. Overall, 145/180 patients (80.6%) had fever during the onset of AF, 120/126 (95.2%) had an elevated ESR (mean, 65.4 [28.65]mm/h), and 168/186 (90.3%) had leukocytosis (mean, 15,484.90 [3922.38]×106L−1).
Systemic Manifestations Associated With Acne Fulminans (n=68).a
| Manifestation | No. (%) of patients |
|---|---|
| Enlarged lymph nodes | 16 (23.53) |
| Cutaneous manifestations | 8 (11.76) |
| Digestive manifestations | 3 (4.41) |
| Neurologic-pyschiatric manifestations | 3 (4.41) |
| Eye manifestations | 1 (1.47) |
| General symptoms | 66 (97.06) |
Musculoskeletal involvement was mentioned for 152/172 patients (88.4%); the main manifestation was arthralgia (75.3%, 143/190) followed by myalgia (12.2%, 17/139). Radiologic changes were observed in 73/125 patients (58%). Notable changes were increased uptake in scintigraphy (31.5%, 23/73) and osteolytic lesions (27.4%, 20/73).
An autoinflammatory syndrome was mentioned for 4/146 patients (2.7%): 3 of the patients had SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome and 1 had PAPA (pyogenic arthritis, pyoderma gangrenosum, and acne) syndrome.
Systemic corticosteroids were the treatment of choice for 81% of AF flares (158/195). The next most common treatments were isotretinoin (52.3%, 102/195) and systemic antibiotics (46.2%, 90/195). A combination of systemic corticosteroids and isotretinoin was used in 90/125 patients (46.2%).
Impact of AF on quality of life was reported for just 2 (0.9%) of the 212 patients analyzed. Both patients had depression, and a suicide attempt was mentioned for 1 of them. Due to this very small subgroup, we were unable to investigate the association between quality of life impairment and other variables.
DiscussionThe clinical and demographic characteristics of AF observed in this narrative review are largely consistent with findings to date.
Our results confirm previous reports of a predominance of AF in adolescents and males.4–7 Practically all the patients (97.6%) in our review had a past history of acne, demonstrating that absence of such a history is very rare. Smaller series of 15,4 24,5 25,6 and 267 patients found that 100% of patients with AF had a history of acne.7
An AF trigger was mentioned for 44.8% of patients analyzed in this review. Drugs were the most common trigger (98.6%), with isotretinoin identified in 65.3% of cases. Triggers described in the largest series to date vary considerably. Bocquet-Trémoreux et al.4 reported a pharmacologic trigger in 60% of patients, with isotretinoin responsible for all cases. The rate in the series of 26 patients described by Massa et al.7 was markedly lower, at 12%, and none of the cases were associated with isotretinoin. No triggers were observed for any of the 8 patients described by Goldschmidt et al.8
The most common sites for lesions in the studies reviewed in this series were the face (89.3%), the posterior trunk (77.9%), and the anterior trunk (74.8%). Other authors have reported a similar predominance of facial (100%) and trunk (87%–88%) lesions.4,5 Hemorrhagic ulcers accounted for 58.9% of all AF lesions in our series. The next most common lesions were nodules and cysts and papules and pustules. Massa et al.7 reported necrotic and ulcerating papules in all 26 patients analyzed.7 Scarring was described in 5/5 patients in the series by Meinzer et al.9 and in 0/6 patients in that of Reunala et al.10 In the studies in our review, scarring was reported for 43.8% of patients. These findings must be interpreted with caution, as it can take time for residual scarring to develop after resolution of an AF flare. Karvonen5 indicated that while 82% of patients no longer had active lesions after several years, they did have residual scarring.5
The pooled analysis of AF cases in our review showed that AF-SS was the most common subtype (59.1%), followed by isotretinoin-induced AF with systemic symptoms (Table 2). Other series show a different distribution.4,8–11
Distribution of Subtypes of Acne Fulminans in the Literature and Present Study.
| AF-SS (%) | AF-WOSS (%) | IIAF-SS (%) | IIAF-WOSS (%) | |
|---|---|---|---|---|
| Bocquet-Trémoureux et al. (n=15) | 10 | 30 | — | 60 |
| Reunala et al. (n=6) | 100 | — | — | — |
| Meinzer et al. (n=5) | 60 | — | 40 | — |
| Goldschimdt et al. (n=8) | 100 | — | — | — |
| Pauli et al. (n=5) | 100 | — | — | — |
| Present study (n=212) | 59.12 | 6.57 | 21.90 | 12.41 |
Abbreviations: AF-SS, acne fulminans with systemic symptoms not induced by isotretinoin; AF-WOSS, acne fulminans without systemic symptoms not induced by isotretinoin; IIAF-SS, isotretinoin-induced acne fulminans with systemic symptoms; IIAF-WOSS, isotretinoin-induced acne fulminans without systemic symptoms.
Overall, 86.4% of patients had extracutaneous manifestations, which were general (nonspecific) in 97.1% of cases. Very few series of 5 or more patients in our review specified type of systemic manifestations. Seukeran and Cunliffe6 reported loss of appetite in 17/25 patients (68%) and weight loss in 9/25 (36%).6 All six patients examined by Reunala et al.10 had general malaise.
Fever was present in 80.6% of the patients reviewed. Other series have reported rates ranging from 92%6 to 100%.8,9 Just 9 (35%) of the 26 patients described by Massa et al.,7 however, had fever. Our findings for elevated ESR and peripheral leukocytosis are consistent with rates in the literature of 92%–100%6,7,10,11 and 87.5%–96%,6–8 respectively.
Musculoskeletal manifestations were present in 88.37% of patients evaluated, with a predominance of arthralgia (75.3%). Although arthralgia was clearly less common in the series of 26 patients published by Massa et al.7 (39%) and that of 15 patients published by Bocquet-Trémoreux et al.4 (6.7%), the rates reported in the other series reviewed were similar to ours and in some cases even higher (80%6–100%5,9–11).
Systemic corticosteroids were the most widely used drugs in the management of AF flares (81%), followed by isotretinoin and systemic antibiotics; 46.2% of patients were treated with a combination of systemic corticosteroids and isotretinoin. Systemic corticosteroids were also the main drugs used in most of the larger series analyzed, with rates of 88%6 and 100%.4,7 The rates for corticosteroids plus isotretinoin ranged between 50% and 100%.6,7,9 Oral antibiotics were administered to 23 (95.8%) of the 24 patients in the series by Karvonen,5 although this high usage may have been influenced by the date of the publication (1993).
The current treatment of choice for AF is prednisone monotherapy at a dosage of 0.5–1mg/kg/d for at least 2 to 4 weeks, followed by low doses of isotretinoin (0.1mg/kg/d).3 Alternatives include topical or intralesional corticosteroids, oral antibiotics (although they do not tend to be very effective), tumor necrosis factor inhibitors, interleukin 1 antagonists, and immunosuppressive agents such as azathioprine, cyclosporine, and methotrexate.3 Colchicine, apremilast, dapsone, and photodynamic therapy may also have beneficial effects.12–14 Pulsed dye laser therapy has shown moderate effectiveness, but can cause adverse effects and pain.15
Low-dose prednisone combined with isotretinoin is also recommended for the prevention of isotretinoin-associated AF in patients with severe inflammatory acne. This initial treatment is followed by a gradual increase in isotretinoin over 3 to 5 months that should be managed according to tolerance. In patients with an extremely high risk of AF, prednisone monotherapy could be attempted for 2 weeks before initiation of isotretinoin.1
Patients with AF can experience significant psychological morbidity due to body image concerns and in some cases may even develop body dysmorphic disorder (BDD).16 In a pilot study of BDD and acne, 8.6% of patients with mild acne and 14.8% of those with mild or moderate acne had BBD.17 A follow-up multicenter study of 245 patients with mild acne showed similar results (10.6% prevalence of BDD).18 Rates may be even higher in AF given the severity of lesions. It is therefore advisable to screen for BDD in patients with acne and AF. If a possible case is detected, the patient should be referred to a mental health unit for diagnostic confirmation and treatment.18
Acne, regardless of its severity, has also been linked to depressive syndromes and suicidal ideation.19 Very few of the studies analyzed in our review evaluated quality of life impairment. Just 2 of the 91 articles mentioned the psychological impact of AF,20,21 suggesting that it is underreported.
This review has some limitations. It is based on case reports and series with heterogeneous reporting of clinical data. We also placed no limit on the initial date for publications included. This may have influenced the clinical variables described and treatments used. The strength of this study lies in the number of patients evaluated (n=212), as the largest series reviewed contain between 15 and 26 patients.4–7
ConclusionsBased on the findings of this narrative review, AF is most common in adolescent boys with a previous history of acne vulgaris. It appears suddenly, over a period of days or weeks, and isotretinoin has a key role as a trigger. The face is affected most. Hemorrhagic ulcers predominate, although approximately 50% of patients also experience scarring. AF with systemic symptoms was the main subtype observed. The most common manifestations are fever, elevated ESR, and leukocytosis. Musculoskeletal involvement is also common, in particular arthralgia with or without radiologic changes. Systemic corticosteroids used alone or in combination with isotretinoin are the most widely used treatment.
Quality of life in patients with AF and the psychosocial impact of this disease are underreported. More insights into these issues would help guide the development of action protocols by multidisciplinary teams.
FundingThis work has not received any kind of funding.
Conflicts of InterestThe authors declare that they have no conflicts of interest.