Malassezia folliculitis is an under-recognizedentity commonly affecting the face and upper trunk. Clinical picture mimics acne vulgaris and diagnosis is challenging at times. 10% potassium hydroxide examination is usually performed to confirm the diagnosis. This study sought to describe the dermoscopic features in Malassezia folliculitis. Patients diagnosed clinically with Malassezia folliculitis and confirmed by 10% potassium hydroxide preparation were included in the study. Dermoscopy was performed with a videodermatoscope [Dinolite AM413ZT; Polarising] from the most representative lesion. A total of 45 patients (M:F = 1:0.8 ) were recruited. All patients had monomorphic papulo-pustular lesions. Itching was present in 64.4% patients. Dermoscopy reveled folliculocentricity (100%), perilesional background erythema (100%), dotted/linear/tortous vessels (88.9%), dirty white scaling (77.8%), hypo pigmentation of hair follicle (64.4%), coiled/looped hairs (57.8%) and broken hairs (13.3%).
In conclusion, dermoscopy shows typical features in Malassezia folliculitis and can serve as a office based tool for identification of this entity.
La foliculitis por Malassezia es una entidad que no está debidamente reconocida y que afecta normalmente a la cara y tronco superior. El cuadro clínico remeda el acné vulgar, siendo a veces difícil su diagnóstico. Normalmente se realiza un examen con hidróxido de potasio al 10% para confirmar el mismo. El objetivo de este estudio fue describir las características dermatoscópicas de la foliculitis por Malassezia, incluyéndose en el mismo a los pacientes diagnosticados clínicamente y confirmados mediante aplicación de hidróxido de potasio al 10%. La dermatoscopia fue realizada con un videodermatoscopio [Dinolite AM413ZT; Polarising] en la lesión más representativa. Se incluyó a un total de 45 pacientes (V:M = 1:0.8). Todos los pacientes tenían lesiones monomórficas papulopustulosas. El 64% de los pacientes presentó prurito. La dermatoscopia reveló foliculocentricidad (100%), eritema circundante perilesional (100%), vasos punteados/lineales/tortuosos (88,9%), escamas de color gris parduzco (77,8%), hipopigmentación del folículo piloso (64,4%), pelos en espiral/enrollados (57,8%) y rotura del pelo (13,3%).
En conclusión, la dermatoscopia muestra las características típicas de la foliculitis por Malassezia, pudiendo servir de ayuda en consulta como herramienta para la identificación de esta entidad.
Malassezia (Pityrosporum) folliculitis presents as monomorphic papule and pustules on the upper back, chest, shoulders and face in adolescents.1,2 It results from the overgrowth of Malassezia yeast present in the normal cutaneous flora. Malassezia folliculitis is usually associated with acne and can persist as monomorphic papules and pustules after complete resolution of acne with typical acne medications. Eruptions may also be associated with immunosuppression and antibiotic use.1 Diagnosis is based on clinical and microbiological examination.1–3 Dermoscopy can serve as an auxiliary tool in the initial assessment of Malassezia folliculitis.4 In this observational study, we describe the dermoscopic features of this common and probably under-reported entity.
ReportThis observational study was conducted at a tertiary care centre, North Delhi Municipal Corporation Medical College & Hindu Rao Hospital, at New Delhi, India in the department of Dermatology; and Microbiology for duration of 6 months. Based on clinical examination, 69 consecutive patients were suspected for having Malassezia folliculitis. All patients underwent 10% potassium hydroxide (KOH) mount examination to detect the presence of hyphae and spores, which generally exhibit the characteristic appearance of “Spaghetti and Meatballs”.5,6 A total of 45 patients out of 69 patients were found to have a positive KOH mount and were included in the study. Patients with negative KOH examination and history of anti fungal medication in past 6 weeks were excluded from the study. Dermoscopy was performed with a universal serial bus (USB) dermatoscope [Dinolite AM413ZT; 50-200X; Polarising]. Dermoscopy was done at 50× and 200× magnification. Based on previous available literature, following dermoscopic parameters were evaluated: folliculocentricity of the lesions, perilesional background erythema, dotted/linear/tortous vessels, dirty white scaling, hypo pigmentation of hair follicle, coiled/looped hairs and any other additional feature.4
The mean age of the patients was 15.7+/-4.3 years with a male to female ratio of 1:0.8. All patients presented with monomorphic papule and pustules [Fig. 1]. Pruritus was complaint by 29 patients (64.4%). Upper trunk was the most common site of involvement (88.9%) followed by shoulders and arms (68.9%) and face (15.5%). Seborrheic dermatitis and pityriasis versicolor was concurrently seen in 22.2% and 17.8% patients, respectively. Overall, 39 patients gave history of acne vulgaris and/or anti-acne medication. Out of these 39 patients, 21 had active acne at the time of examination. Oral antibiotics were received by 32 patients at some time during their treatment for acne.
Dermoscopy reveled folliculocentricity of the lesion in all cases (100%) with perilesional background erythema (100%) [Fig. 2]. There was a mix pattern of the morphology of vessels in and around the lesions. Dotted/linear/tortous vessels were seen in 88.9% of the lesions observed under dermatoscope. Dirty white scaling (lesional and perilesional) was noted in 77.8% of the lesions. Involvement of the hair shaft was noted as hypo pigmentation of proximal or complete hair shaft in 64.4% patients and 57.8% patients also showed coiled to looped hairs (keratosis pilaris like features). Broken Hairs were seen in 13.3 % of the patients.
DiscussionMalassezia (Pityrosporum) folliculitis (MF), an acneiform eruption, was first described by Weary et al in 1969 and recognized by Potter in 1973 as a specific disease.6 It is often misdiagnosed as acne vulgaris, making it easy to miss and thus is likely an under-diagnosed entity. MF is a benign disorder that results from an overgrowth of the Malassezia yeast present in the normal cutaneous flora, secondary to occlusion of the follicle or disturbance of normal cutaneous flora.7,8 As it thrives on the lipid composition of sebum, this yeast is primarily found in the infundibulum of the sebaceous glands. It uses its own enzymes like lipases and phospholipases to cause hydrolyisis of triglycerides from sebum into free fatty acids for their own nutritive lipid source, thus leading to growth and proliferation.1 The complex interaction of a unicellular eukaryotic organism (Malassezia) with a multicellular organism’s tissue (skin) makes understanding of the interactions and development of disease a compound process.7
Malassezia folliculitis often appears in the upper trunk, i.e., shoulders, back, and chest, and occlusion is a common predisposing factor with pruritus as a frequent symptom.8 The condition is also associated with immunosuppression; however, in these patients, it may appear with less distinct pruritus.1 Diagnosis is done by Wood's lamp examination, confirmed mycologically by using 10% KOH, cultivation on Sabouraud's dextrose agar and modified Dixon agar. Performing lactophenol cotton blue mount can do speciation.5 Other tests include urease test, catalase test, esculin hydrolysis, temperature tolerance test and utilization of Tween 20, 40, 60 and 80.5 In our study, diagnosis was confirmed by 10% KOH examination.
Dermoscopy has become a valuable tool in the diagnosis of a number of dermatoses. There is increasing literature regarding its utility in the diagnosis of Malassezia and dermatophytic infections.4,9 Folliculocentricity of the lesions and surrounding erythema has been described as a uniform feature in Malassezia folliculitis.4 In addition, in this study dermoscopy revealed various vascular structures in the form of dotted, linear and tortuous vessels. Individual lesion showed more than one morphology of vessel (dotted/linear/tortuous) in the erythematous background. The pattern of the morphology and arrangement of vessels was non-uniform and non-specific. Lesional and peri-lesional dirty white scaling again showed no specific arrangement and pattern. Infection of the hair follicle by the Malassezia has been suggested in the pathogenesis of Malassezia folliculitis.10 Hypopigmentation of the proximal hair shaft has been proposed as the dermoscopic counterpart of the same.4 Our study also showed this dermoscopic feature in a considerable number (64.4%) of patients. The coiled or looped hairs on dermoscopy possibly depicts weakening of the hair shaft due the invasion of the hair follicle by Malassezia thus leading to the coiling of the hair shaft. Broken hairs, again, depicts the invasion of hair shaft by Malassezia. Broken hairs are mentioned as a dermoscopic feature of tinea capitis and this is the first report of their presence in Malassezia infection. Comedones, which are a feature of acne vulgaris, were not seen in our study.4
Differential diagnosis for Malasezzia folliculitis includes acne vulgaris, bacterial folliculitis and pseudofolliculitis. Dermoscopy of acne vulgaris shows comedone as brown-yellow hard central plug; inflammatory acne as round structured lesions with white centre, thin brown borders and erythematous periphery; and pustular acne as dull white-yellow lesions with erythematous periphery.4 Dermoscopy of bacterial folliculitis shows non-specific features like central round pustule with peripheral sparse dotted vessels.11 Dermoscopy of pseudofolliculitis shows an ingrown hair and surrounding erythema.11
To conclude, dermoscopy shows peculiar features in Malassezia folliculitis. Presence of these features on dermosocpy should prompt a dermatologist to consider antifungal treatment with or without anti-acne treatment for complete resolution of lesions.



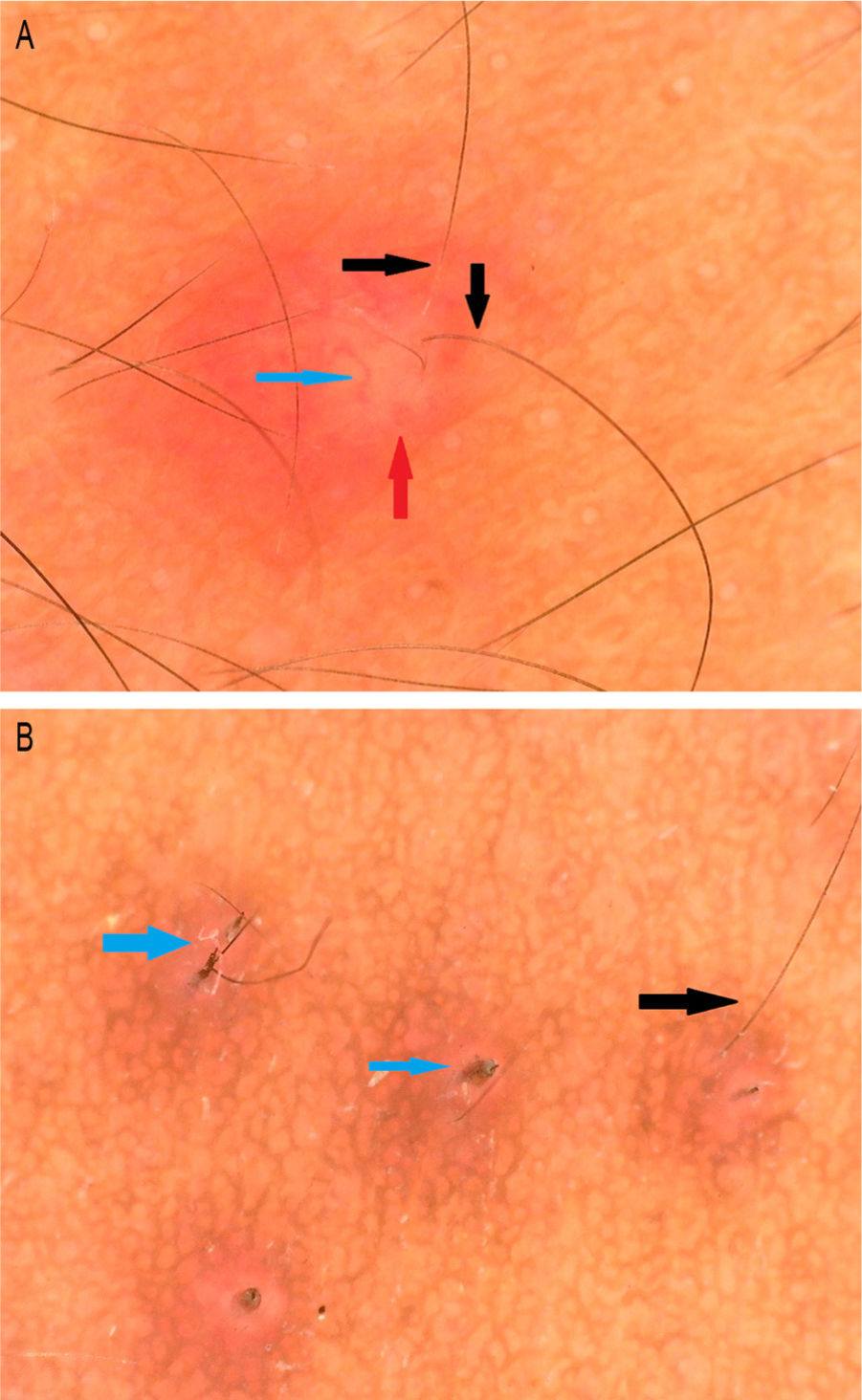

![a) Folliculocentric lesion with surrounding erythem (red arrow), tortuous vessel (blue arrow) and hypopigmentation of the proximal hair shaft (black arrow); b) broken hairs (blue arrow) and hypopigmentation of proximal hair shaft. [Dinolite AM4115ZT; 150X; polarizing]. a) Folliculocentric lesion with surrounding erythem (red arrow), tortuous vessel (blue arrow) and hypopigmentation of the proximal hair shaft (black arrow); b) broken hairs (blue arrow) and hypopigmentation of proximal hair shaft. [Dinolite AM4115ZT; 150X; polarizing].](https://static.elsevier.es/multimedia/00017310/0000011300000001/v2_202202160543/S0001731022000151/v2_202202160543/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



