There is a lack of studies assessing whether wide excision surgery in hidradenitis suppurativa affected areas is useful for the global control of the hidradenitis suppurativa. We aimed to find whether surgery results were a better global control on the disease activity in both, the area where the surgery is performed and distant areas. We evaluated the disease course of 17 patients with hidradenitis suppurativa who underwent wide excision of complex fistula tracts between October 2018 and January 2022 at the Hospital Universitario de la Princesa, Madrid. We found that wide excision of complex fistulas produces an overall positive effect on the inflammatory activity in hidradenitis suppurativa that may be important to achieve an adequate control of the disease.
No existen estudios que se centren en la utilidad del tratamiento con cirugía amplia para el control global de la hidradenitis supurativa. En el presente estudio hemos evaluado el curso de la enfermedad de 17 pacientes con hidradenitis supurativa a los que se les realizó extirpación de trayectos fistulosos mediante cirugía amplia entre octubre de 2018 y enero de 2022 en el Hospital Universitario de La Princesa. Encontramos como resultado que el tratamiento mediante cirugía amplia produce un beneficio global en la actividad inflamatoria de la enfermedad y puede ser importante para el control de la hidradenitis supurativa.
Hidradenitis suppurativa (HS) is a chronic inflammatory disease characterized by relapsing painful abscesses, scars and sinus tract formation.
The multidisciplinary treatment of the disease includes medical therapies, as well as surgical options.1–3
There is a lack studies assessing the usefulness of wide local excision in the overall control of the disease. The idea that wide excision of chronic and irreversible fistulas may improve the overall activity and course of the disease, reducing flares in the intervention area and other anatomical sites has remained unexplored. We aimed to determine whether surgery results were a better global control on the disease activity and reducing flare ups in both: the area where the surgery is performed, and distant areas.
Case series and methodsWe designed a retrospective study that reviewed all patients with a diagnosis of moderate to severe hidradenitis suppurativa (Hurley score ≥2) who underwent wide excision of complex fistula tracts between October 2018 and January 2022 at our center. Patients were selected as they presented one or two (n=3 patients) predominantly affected areas to perform surgery.
We collected: demographic parameters (age, gender, body weight and smoking history); HS parameters (duration of HS symptoms before surgery, number of flares previous to the surgery, localization of the lesion, previous treatments and number of flares after the surgery); and surgery satisfaction and complications (Table 1). We considered flare ups as the development of new lesions that required intensification or initiation of treatment to control the disease: both as local recurrence and in a distant anatomical site, while analyzing both locations separately.
Demographic and hidradenitis suppurativa data of our patients.
| N | Age | Gender | Localization of the lesion | Hurley (baseline) | Classification of fistulas | Previous treatments | Reconstruction | Follow up(months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 32 | M | Right axilla | III | C | AB+ADA | Local flap | 12 |
| 2 | 43 | F | Right axilla | III | C | AB | Local flap | 12 |
| 3 | 30 | M | Right buttock | III | D | AB | Graf | 12 |
| 4 | 50 | F | Right axilla | III | C | AB+ADA | Local flap | 12 |
| 5 | 57 | F | Left groin | II | B | AB | Direct closure | 12 |
| 6 | 58 | F | Right axilla and left groin | III | B | AB | Direct closure | 12 |
| 7 | 33 | M | Left groin | II | C | AB | Direct closure | 12 |
| 8 | 20 | F | Right and left axilla | III | B/C | AB+ADA | Local flap | 12 |
| 9 | 44 | F | Left axilla | II | B | AB | Local flap | 12 |
| 10 | 53 | F | Right and left axilla | III | C/C | AB | Local flap | 12 |
| 11 | 41 | F | Genital | II | B | AB | Direct closure | 12 |
| 13 | 59 | M | Perianal | II | B | AB | Direct closure | 12 |
| 14 | 21 | F | Right and left axilla | II | B/C | AB | Local flap | 12 |
| 15 | 17 | M | Genital | III | C | AB | Local flap | 6 |
| 16 | 62 | F | Right groin | II | B | AB | Local flap | 12 |
| 17 | 60 | F | Right groin | II | B | AB | Direct closure | 12 |
AB: antibiotic; ADA: adalimumab.
HS severity was assessed with the International Hidradenitis Suppurativa Severity Score System (IHS4) and Martorell ultrasound classification of fistulas.4,5 Data were evaluated at 6, 3 and 1 month before and after the surgical procedure. Sixteen patients completed a 12 month follow up. The surgical technique used was wide local surgical excision, which consisted in: using local or tumescent anesthesia, the removal of an entire affected area, reaching clinically disease free subcutaneous fatty tissue, followed by reconstruction and not by second intention healing (Fig. 1).
Descriptive statistics were performed using SPSS software ver. 22.0 (IBM®, Armonk, NY, USA) and expressed as means and ranges.
ResultsSeventeen patients, who accounted for twenty wide excisions, were included in the study. Mean age was 44 years (21–62 years), 11 patients (64.7%) were woman. Most of the patients were obese (70.59%; 12/17) and had a positive history of smoking (82.35%; 14/17).
The average time between disease onset and surgery was 15.4 years (2–31 years). Regarding disease severity, 58.8% (10/17) of patients presented Hurley stage II and 41.2% (7/17) presented stage III. Most surgeries were performed in the axilla (11) followed by the inguinal (4), genital (3) and gluteal–perineal region (2).
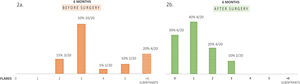
A large proportion of patients (65%; 13/20) presented between 3 and 6 flares within 6 months before surgery and four patients (20%; 4/20) suffered subintrant flares before the surgical intervention (Fig. 2a).
Before surgery, all patients were treated with at least 1 cycle of oral antibiotic and three patients were under treatment with adalimumab. There were several periods of treatment with subsequent discontinuation due to lack of response or disease control: patient 3 (33 months), patient 4 (23 months) and patient 8 (25 months). Ten type B, 9 type C and one type D fistulas were surgically treated. The types of reconstruction performed were either local flap (9/20), direct closure (10/20) or skin graft (1/20). Surgery complications were 2/17 moderate pain that required analgesia, 1/17 seroma and 1/17 wound infection.
With a mean follow up of 11.65 months, local recurrence rate was 10% (2/20), at locations previously affected by the disease, and 15 from 17 patients (88.2%) remained without inflammatory activity (Fig. 2b) and did not need further antibiotic therapy.
At a six month follow up 40% (8/20) remained free of disease globally and 50% (10/20) presented mild activity (IHS4≤3). (Fig. 3).
Reduction of disease severity after surgery. Graph shows percentage of patients with different degrees of disease severity according to the International Hidradenitis Suppurativa Severity Score System (IHS4). (a) Six months prior to surgery (average). (b) At six-month of follow up. (c) Baseline IHS4 and after surgery (6 months).
Regarding satisfaction, all patients were satisfied with the esthetic results and declared that they would undergo the same surgical procedure again if necessary.
DiscussionFistulous tracts are considered as one of the most important signs of severity in HS because of their capacity to generate irreversible structures that require surgical management.2
Previous reports in the literature on the use of wide local excision in HS, was mainly focused on local recurrence.2
At the time of writing wide excision is accepted as an adequate surgical choice, with a lower local recurrence rate (13–33%), depending on the follow up period, surgery location and closure method.6,7 In our case study, the recurrence rate in the intervened area after wide excision of complex fistulas was 10%. Walters et al. were one of the few authors who reported that when performing surgery on both local and distant flare ups also improved in anatomical areas which were different from those that underwent surgery.8
Our results show an important decrease in the inflammatory activity after surgery: flares were reduced a mean of 77.8%. Similarly, disease severity was greatly reduced after surgery: six months after surgery most of the patients did not develop new symptoms [IHS4=0] or maintained mild activity [IHS4≤3]). As a consequence of reduction in flares, the use of antibiotics through follow up was lower than that of the six months prior to surgery. Regarding patient satisfaction, 100% of the patients were satisfied with the outcome of the surgery and claimed that they would undergo the same surgical procedure again if they presented similar lesions to those previously operated.
The present study has some limitations. Firstly, the sample size is small and the follow up is short. Secondly, although HS has an important impact on patient's life,9,10 we did not use questionnaires to assess changes in quality of life.
ConclusionsResults from our series suggest that wide excision of complex fistulas (type B, C and D) improve HS control, by reducing the number of flares at the surgical site and at distant locations. Consequently, the use of oral and topical antibiotics was also reduced. This procedure presents low recurrence and provides high patient satisfaction with the surgery and the aesthetic results. These results warrant further validation studies with larger cohorts and long term follow up.
Conflict of interestsThe authors declare they have no conflict of interest.