Cutaneous squamous cell carcinoma is the second most common tumor in humans. Its incidence is growing and remains underestimated. In Spain, the gross incidence is estimated at 38.16 cases per 100 000 persons per year1. Cutaneous squamous cell carcinoma is the second most common cause of death from skin cancer after melanoma and is responsible for most deaths from skin cancer in persons aged >85 years2.
In dermatologic surgery, second-intention healing is an alternative to reconstruction via direct closure, flaps, or grafts. In surgical treatment of skin cancer, second-intention healing has the advantage of not involving movement of adjacent planes and facilitating detection of recurrence at deeper levels. The main disadvantage of this technique is the longer time to wound healing. Second-intention healing may be a useful option in the surgery of squamous cell carcinomas located on the scalp of elderly patients with comorbid conditions that increase the risks associated with surgery.
Bone wax is a biologically inert material that does not cause skin allergy or irritant dermatitis. It is not absorbed and remains in the wound without adhering to it. It is also very malleable after heating with the hands before application. These qualities make it effective as a sterile dressing for the formation of granulation tissue in surgery involving exposure of bone and cartilage3.
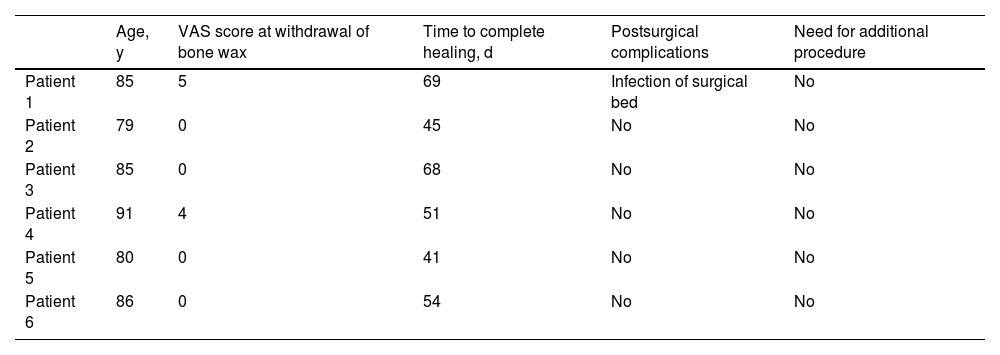
We analyzed a series comprising 6 elderly patients with cutaneous squamous cell carcinoma measuring between 2 and 4 cm on the scalp. The tumors were removed, with exposure of the bone, including the periosteum, in all 6 cases. Closure was by second intention and compression with gauze attached to the skin using staples (Fig. 1). The patients’ age varied from 79 to 91 years. All 6 patients had cardiovascular comorbidity (American Society of Anesthesiologists III-IV). Free margins were achieved in all cases, and no subsequent procedures for definitive coverage with a skin graft were necessary. Surgery took less than 15 minutes in all cases. The mean score on the visual analog scale for pain (0 to 10) on withdrawal of the bone wax at 2 and 3 weeks after surgery was 1.5. Moist wound healing was performed every 72 hours with mupirocin ointment after cleaning the wound with saline solution and applying a silicone mesh dressing (Mepitel). The mean time to complete scarring was 54.6 days. As for postsurgical complications, no patients required the compressive dressing to be removed early, and no bleeding was recorded. Infection of the surgical bed by Staphylococcus aureus was recorded in only 1 patient. This was treated satisfactorily with oral antibiotics (Table 1).
A, Skin tumor measuring >2 cm on the scalp. B, Surgical defect after removal of a tumor involving exposure of the bone. C, Application of bone wax molded into the surgical wound. D, Occlusive compressive dressing with metal staples. E, Complete granulation on withdrawal of bone wax 30 days after the surgery. F, Complete healing of the surgical wound.
Characteristics of Patients Who Underwent Second Intention Closure With a Bone Wax Dressing.
| Age, y | VAS score at withdrawal of bone wax | Time to complete healing, d | Postsurgical complications | Need for additional procedure | |
|---|---|---|---|---|---|
| Patient 1 | 85 | 5 | 69 | Infection of surgical bed | No |
| Patient 2 | 79 | 0 | 45 | No | No |
| Patient 3 | 85 | 0 | 68 | No | No |
| Patient 4 | 91 | 4 | 51 | No | No |
| Patient 5 | 80 | 0 | 41 | No | No |
| Patient 6 | 86 | 0 | 54 | No | No |
Abbreviation: VAS, visual analog scale.
In conclusion, we would like to highlight that second intention healing with bone wax as a sterile dressing could be an alternative for removal of cutaneous squamous cell carcinoma in elderly patients for whom surgery may be high-risk. This approach reduces the duration of surgery and obviates the need for more complex techniques with potentially greater morbidity.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ortiz-Prieto A, Padial-Gomez A, Márquez-Enríquez J. Utilidad de la cera para huesos en la cirugía del carcinoma epidermoide cutáneo del cuero cabelludo en pacientes con alto riesgo quirúrgico. Actas Dermosifiliogr. 2022;113:216–218.