Bleeding complications during dermatologic surgery are uncommon and usually minor, but bleeding occasionally leads to infection, wound dehiscence, or flap/graft necrosis. This review covers the keys to preventing, recognizing, and treating excessive bleeding during and after surgery.
Las complicaciones por hemorragia quirúrgica en la cirugía dermatológica son infrecuentes y poco relevantes en la mayoría de los casos. En algunas ocasiones la hemorragia quirúrgica puede conllevar infección de la herida quirúrgica, dehiscencia de sutura o necrosis del colgajo/injerto. En esta revisión se muestran los aspectos más importantes para prevenir, reconocer y tratar este tipo de complicaciones durante el acto quirúrgico y tras él.
While complications in dermatological surgery are infrequent, a considerable proportion are due to major perioperative or postoperative bleeding (i.e. bleeding that does not subside with compression measures). In a study of a large series of patients who underwent Mohs micrographic surgery, complications occurred in approximately 2% of patients, and corresponded to postsurgical bleeding in 40% of cases.1 Although this complication does not usually have major implications (a decrease in hematocrit requiring blood transfusion occurred in very few cases), it can occasionally lead to infection of the surgical wound, suture dehiscence, or necrosis of the flap or graft.1
Bleeding is defined as a noncircumscribed accumulation of blood that infiltrates tissues after rupture of a blood vessel wall. A hematoma is defined as the localized collection of usually coagulated blood in an organ, space, or tissue due to rupture of a blood vessel wall. Hematoma formation consists of 4 stages: early formation (I), gelatinous (II), organized (III), and liquefaction (IV) stages.1 It is important to detect the hematoma as early as possible to avoid the aforementioned complications.
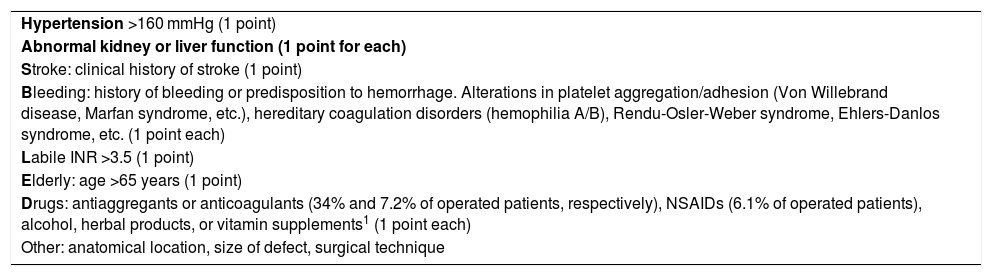
It is essential to recognize the possibility of bleeding both during and after the intervention, and to perform a meticulous medical history and physical examination in the consultation before surgery. Indices such as the HAS-BLED2 are useful to assess a patient’s risk of bleeding (Table 1).
HAS-BLED Scoring System.
| Hypertension >160 mmHg (1 point) |
| Abnormal kidney or liver function (1 point for each) |
| Stroke: clinical history of stroke (1 point) |
| Bleeding: history of bleeding or predisposition to hemorrhage. Alterations in platelet aggregation/adhesion (Von Willebrand disease, Marfan syndrome, etc.), hereditary coagulation disorders (hemophilia A/B), Rendu-Osler-Weber syndrome, Ehlers-Danlos syndrome, etc. (1 point each) |
| Labile INR >3.5 (1 point) |
| Elderly: age >65 years (1 point) |
| Drugs: antiaggregants or anticoagulants (34% and 7.2% of operated patients, respectively), NSAIDs (6.1% of operated patients), alcohol, herbal products, or vitamin supplements1 (1 point each) |
| Other: anatomical location, size of defect, surgical technique |
Abbreviations: INR, international normalized ratio; HT, hypertension; NSAID, nonsteroidal anti-inflammatory drugs.
HAS-BLED evaluates the risk of bleeding complications based on the indicated parameters.
Significant risk of intervention-related bleeding if score ≥3.
Other factors to take into account are the anatomical location and the surgical technique performed, although some authors have reported no significant differences in bleeding risk between different surgical procedures.5 Larger defect size, administration of perioperative antibiotics, and a history of hidradenitis suppurativa are associated with an increased risk of bleeding.6
Three specific regions are associated with a higher risk of bleeding: the frontotemporal region, where the temporal artery is located; the mandibular rim, over which the facial artery runs; and the area adjacent to the nose, where the angular artery runs.1 Other regions that in our experience are associated with a greater risk of bleeding include the genital region (especially in interventions involving the scrotum and vulva) and the flexures (armpits and groin). Furthermore, in areas such as the periorbital or cervical regions formation of a hematoma entails significant risk of compression of neighboring structures due to the mass effect (and greater risk of tissue necrosis or surgical wound dehiscence).1
PreventionDifferent measures can be taken before the intervention to prevent both perioperative and postoperative bleeding. Twenty years ago, anticoagulant and antiplatelet treatments were withdrawn to prevent bleeding in most patients undergoing dermatological surgery. Nowadays, the trend is to maintain these therapies, especially in cases of minor outpatient surgery. Given the usually minor implications of surgical bleeding complications and the serious consequences of thromboembolic phenomenon after surgical intervention when anticoagulant therapy is withdrawn (despite the low frequency of these episodes), we recommend making the decision to withdraw treatment on a case-by-case basis.
Acetylsalicylic acid does not appear to increase the risk of surgical bleeding, and therefore withdrawal of antiplatelet therapy is not recommended. Patients who take clopidogrel have a higher risk of bleeding than those not receiving anticoagulation or antiplatelet therapy. Nonetheless, given the low severity of bleeding episodes, continuation of this treatment or replacement with acetylsalicylic acid is recommended.3 For patients receiving dual antiplatelet therapy (e.g. acetylsalicylic acid + clopidogrel) there is no clear consensus on the appropriate course of action. In these patients the risk of bleeding appears to be greater than in patients receiving antiplatelet monotherapy, and therefore it is recommended to reduce antiplatelet therapy to a single agent if possible.7
In patients receiving anticoagulant therapy, the international normalized ratio (INR) should first be assessed, when possible, as in the case of acenocoumarol (Sintrom), and postponement of the intervention should be considered if the value exceeds 3.5.8
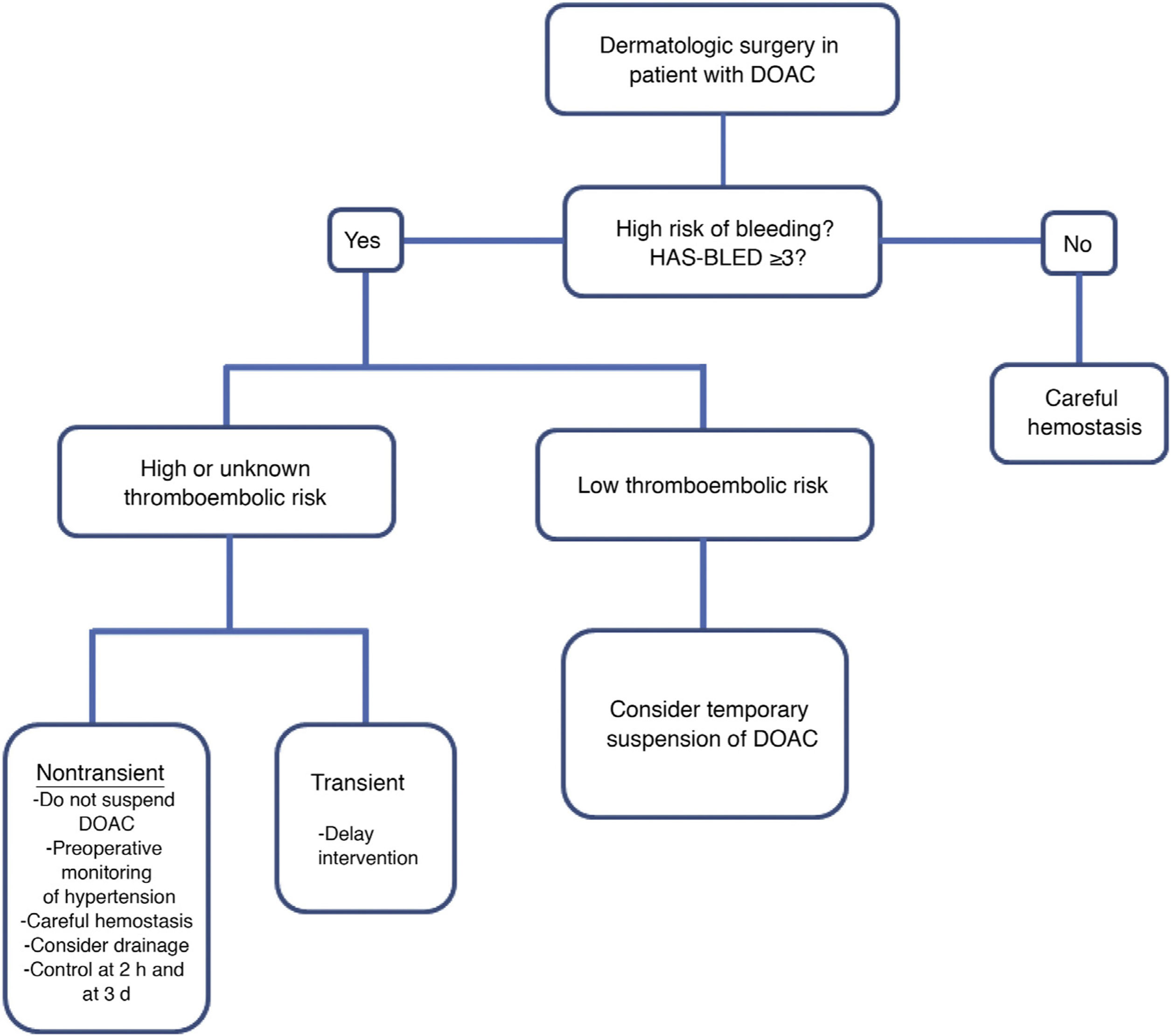
There is little information on the preoperative management of patients being treated with new direct oral anticoagulants, which are prescribed with increasing frequency. Figure 1 shows the algorithm for the management of patients undergoing treatment with these drugs.2
Dermatological surgery: management of patients receiving direct oral anticoagulation therapy. *High thromboembolic risk in patients with any of these characteristics: recent venous thromboembolism (<90 days), active malignancy, severe thrombophilia, atrial fibrillation with a CHADS2 score of 5–6 or a CHADS2-VASc score of 7–9, stroke <90 days or mechanical heart valve (mitral or aortic, tipping disc or balloon type, multiple mechanical valves, or recent cerebral ischemia [<6 months]). Abbreviations: DOAC, direct oral anticoagulants.
Modified from Cabezas Calderón et al.2
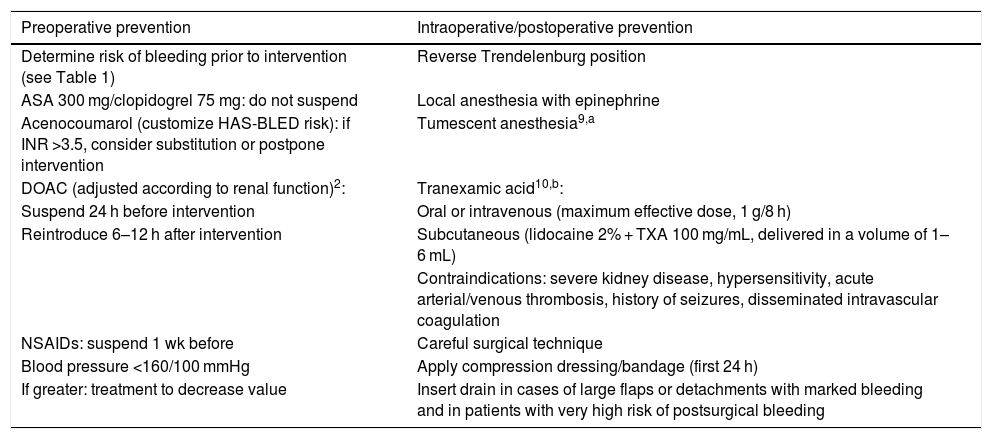
As mentioned above, nonsteroidal anti-inflammatory drugs (NSAIDs) are widely used to control pain and inflammation. Given the potential risk of bleeding caused by this type of drug, it is recommended to discontinue treatment 1 week before surgery until up to 2 days after the intervention. It is advisable to manage postoperative pain with paracetamol or metamizole.1
Given that blood pressure (BP) is a risk factor for bleeding, it is recommended to perform the intervention provided the patient has a systolic BP ≤ 160 mmHg or a diastolic BP ≤ 100 mmHg (BP monitoring before and during the intervention is advisable). If the patient’s BP exceeds the aforementioned values, the intervention should ideally be postponed until values are brought to within the recommended range.1,2
Table 2 lists the points that should be taken into account to prevent intraoperative bleeding.
Preoperative, Intraoperative, and Postoperative Prevention of Surgical Bleeding.
| Preoperative prevention | Intraoperative/postoperative prevention |
|---|---|
| Determine risk of bleeding prior to intervention (see Table 1) | Reverse Trendelenburg position |
| ASA 300 mg/clopidogrel 75 mg: do not suspend | Local anesthesia with epinephrine |
| Acenocoumarol (customize HAS-BLED risk): if INR >3.5, consider substitution or postpone intervention | Tumescent anesthesia9,a |
| DOAC (adjusted according to renal function)2: | Tranexamic acid10,b: |
| Suspend 24 h before intervention | Oral or intravenous (maximum effective dose, 1 g/8 h) |
| Reintroduce 6–12 h after intervention | Subcutaneous (lidocaine 2% + TXA 100 mg/mL, delivered in a volume of 1–6 mL) |
| Contraindications: severe kidney disease, hypersensitivity, acute arterial/venous thrombosis, history of seizures, disseminated intravascular coagulation | |
| NSAIDs: suspend 1 wk before | Careful surgical technique |
| Blood pressure <160/100 mmHg | Apply compression dressing/bandage (first 24 h) |
| If greater: treatment to decrease value | Insert drain in cases of large flaps or detachments with marked bleeding and in patients with very high risk of postsurgical bleeding |
Abbreviations: ASA, acetylsalicylic acid; DOAC, direct oral anticoagulants; INR, international normalized ratio; NSAIDs, non-steroidal anti-inflammatory drugs; TXA, tranexamic acid.
In our experience, patients who undergo general anesthesia may experience an increase in BP in the recovery room after the intervention, with a consequent increase in the risk of bleeding due to improperly ligated or coagulated vessels. For this reason, we believe it is useful to evaluate the intervened area a few minutes after surgery to rule out the presence of postoperative bleeding.
It is also advisable to apply a compression bandage during the first 24 hours in at-risk patients or after risky interventions. After 24 hours the efficacy of this measure likely decreases. It is also important to instruct the patient about correct care of the postoperative wound and any warning signs about which the surgeon should be notified (e.g. bleeding or hematoma, necrosis of the flap or graft, dehiscence, or infection). Ideally the patient should not consume alcohol in the first 7 days after the intervention owing to its vasodilatory effect.11
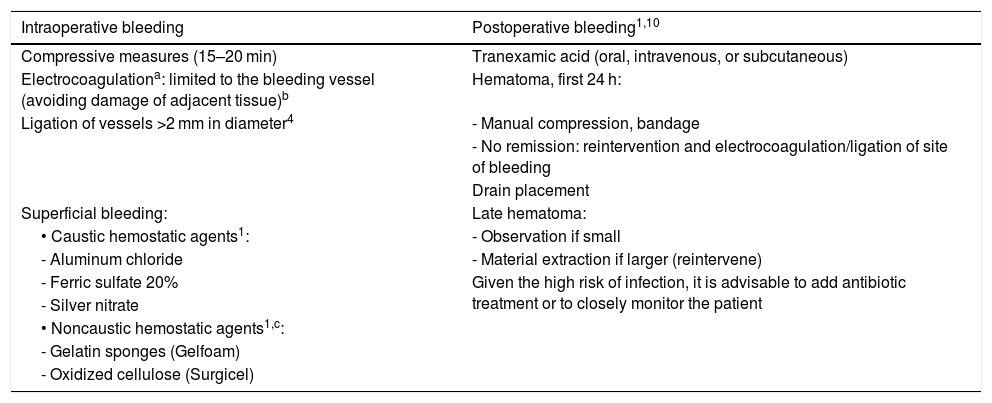
TreatmentAs mentioned above, bleeding in dermatological surgery does not usually have major implications, and in most cases can be controlled using compression for a maximum of 15 to 20 minutes. In cases of severe bleeding the affected vessel can be compressed. This allows time for platelet adhesion and initiation of the coagulation cascade, as well as application of other techniques to stop the bleeding.4 As indicated in Table 3, other therapeutic options in cases of intraoperative bleeding include ligation or electrocoagulation of the affected vessel.
Treatment of Bleeding.
| Intraoperative bleeding | Postoperative bleeding1,10 |
|---|---|
| Compressive measures (15–20 min) | Tranexamic acid (oral, intravenous, or subcutaneous) |
| Electrocoagulationa: limited to the bleeding vessel (avoiding damage of adjacent tissue)b | Hematoma, first 24 h: |
| Ligation of vessels >2 mm in diameter4 | - Manual compression, bandage |
| - No remission: reintervention and electrocoagulation/ligation of site of bleeding | |
| Drain placement | |
| Superficial bleeding: | Late hematoma: |
| • Caustic hemostatic agents1: | - Observation if small |
| - Aluminum chloride | - Material extraction if larger (reintervene) |
| - Ferric sulfate 20% | Given the high risk of infection, it is advisable to add antibiotic treatment or to closely monitor the patient |
| - Silver nitrate | |
| • Noncaustic hemostatic agents1,c: | |
| - Gelatin sponges (Gelfoam) | |
| - Oxidized cellulose (Surgicel) |
In the case of patients with a pacemaker or implantable automatic defibrillator, it is recommended to use a bipolar electric scalpel, which has a greater safety profile (the current flows between 2 electrodes placed in the area of application, and does not flow through the patient).12.
A case series of 9154 operated patients found that 7.4% presented some form of postoperative bleeding, which in most cases (87.5%) was controlled by applying pressure or replacing bandages.6 Intervention by a dermatologist was required in 12.5% of postoperative bleeding cases; electrocautery was used to stop bleeding in 10% of cases; and bleeding was considered severe in only 2.2% of patients.6Table 3 describes the management of patients with postsurgical bleeding, differentiating between hematoma within the first 24 hours and late hematoma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Iglesias Zamora ME, Aróstegui Aguilar J. Seguridad en procedimientos dermatológicos: hemorragia quirúrgica en cirugía dermatológica. Cómo reconocerla, prevenirla y tratarla. Actas Dermosifiliogr. 2022;113:67–71.

![Dermatological surgery: management of patients receiving direct oral anticoagulation therapy. *High thromboembolic risk in patients with any of these characteristics: recent venous thromboembolism (<90 days), active malignancy, severe thrombophilia, atrial fibrillation with a CHADS2 score of 5–6 or a CHADS2-VASc score of 7–9, stroke <90 days or mechanical heart valve (mitral or aortic, tipping disc or balloon type, multiple mechanical valves, or recent cerebral ischemia [<6 months]). Abbreviations: DOAC, direct oral anticoagulants. Modified from Cabezas Calderón et al.2 Dermatological surgery: management of patients receiving direct oral anticoagulation therapy. *High thromboembolic risk in patients with any of these characteristics: recent venous thromboembolism (<90 days), active malignancy, severe thrombophilia, atrial fibrillation with a CHADS2 score of 5–6 or a CHADS2-VASc score of 7–9, stroke <90 days or mechanical heart valve (mitral or aortic, tipping disc or balloon type, multiple mechanical valves, or recent cerebral ischemia [<6 months]). Abbreviations: DOAC, direct oral anticoagulants. Modified from Cabezas Calderón et al.2](https://static.elsevier.es/multimedia/00017310/0000011300000001/v2_202202160543/S0001731022000060/v2_202202160543/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



