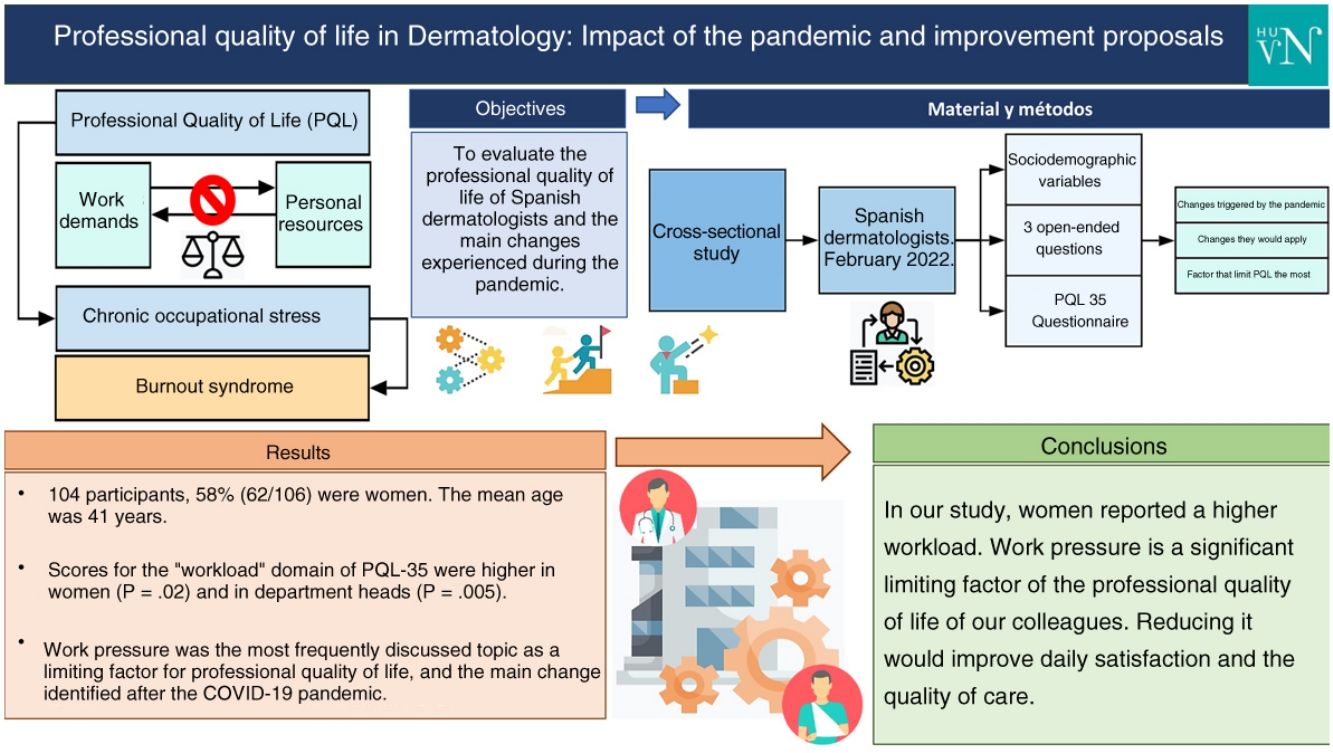
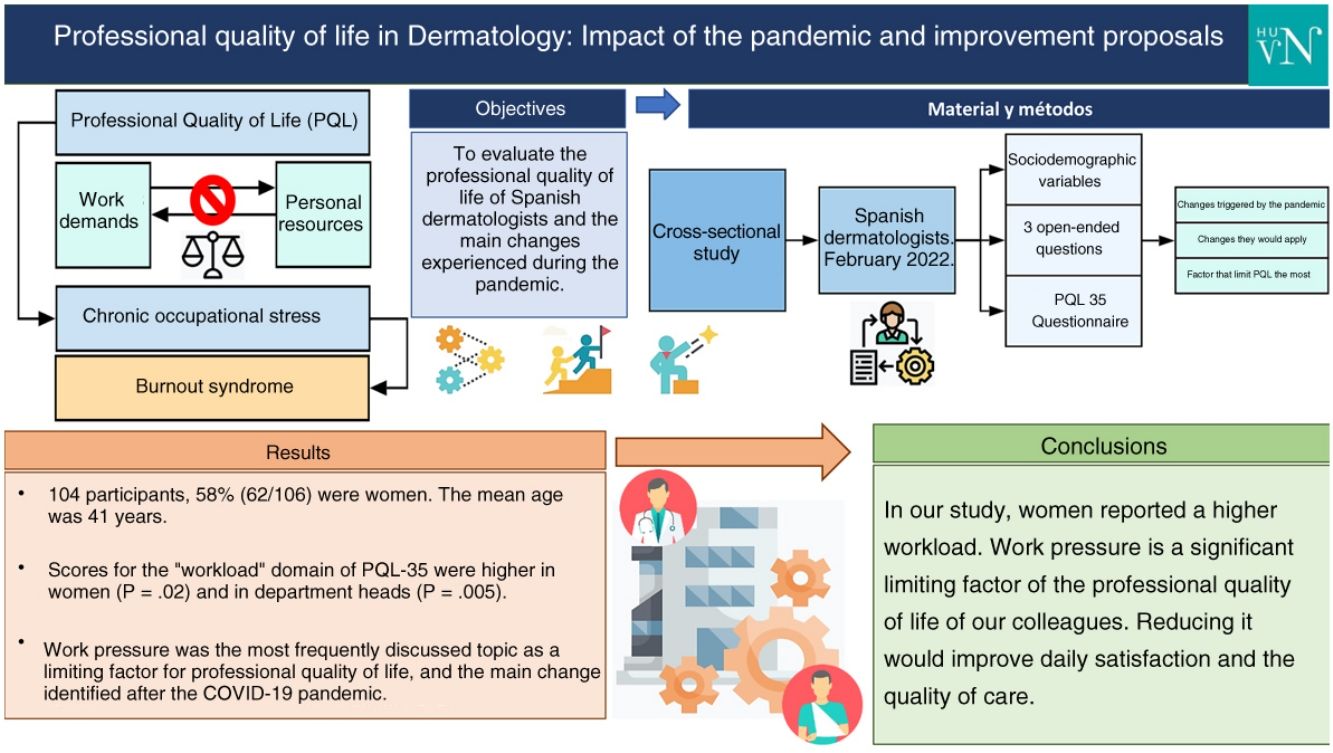
Quality of professional life (QPL) is defined as a sense of well-being derived from a balance between the challenges of work and the resources available to deal with them. Impaired QPL can contribute to burnout. The aim of this study was to evaluate QPL in Spanish dermatologists using a validated questionnaire.
Material and methodsWe designed a cross-sectional study in which Spanish dermatologists were invited to complete an online questionnaire sent out by messaging applications. The dermatologists were asked to provide sociodemographic information, answer 3 open questions, and complete the 35-item Spanish QPL questionnaire (Spanish abbreviation, CVP-35).
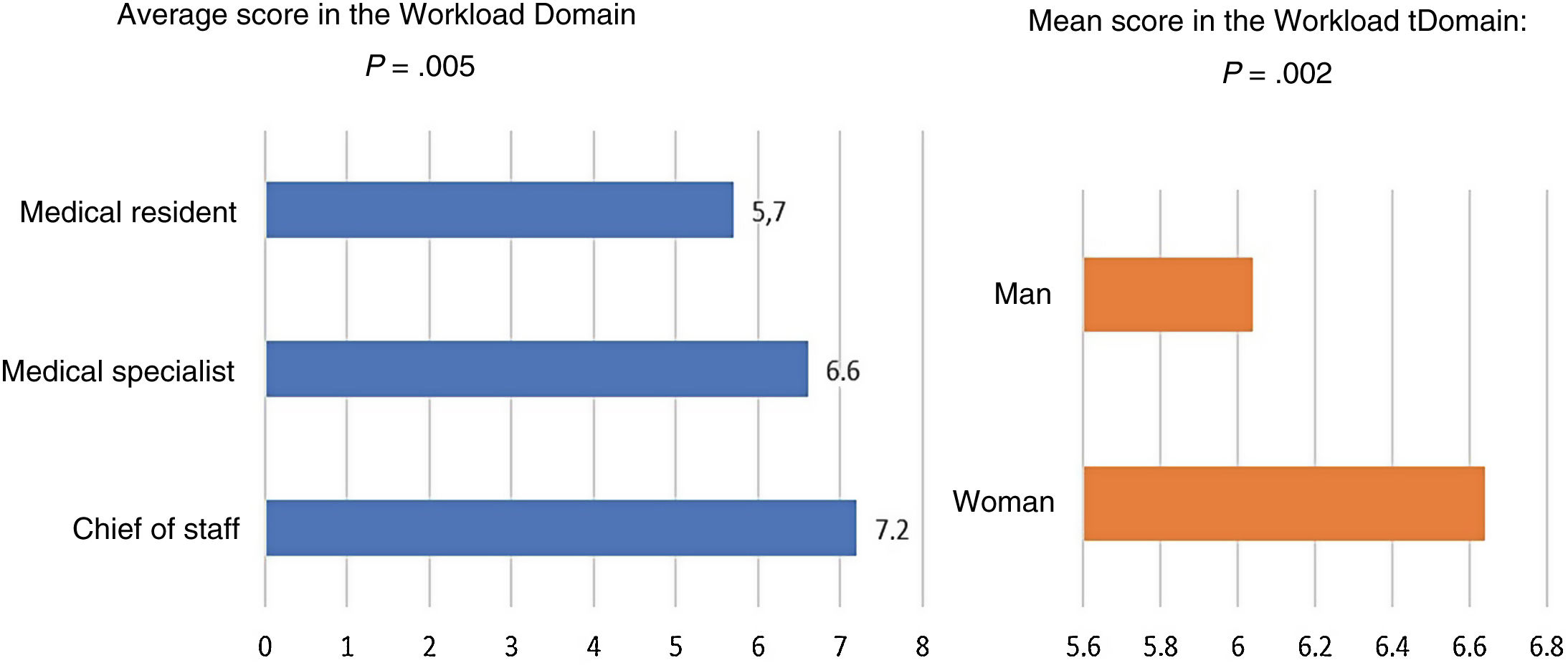
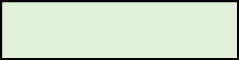
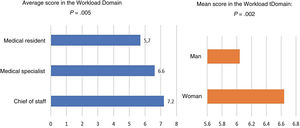
ResultsWe analyzed the information submitted by 106 dermatologists (62 women, 58%) with a mean age of 41 years (95% CI, 43.3-38.8 years). Women and department heads scored significantly higher in the workload domain of the questionnaire (P=.02 and P=.005, respectively). A heavy caseload was mentioned as the main factor contributing to impaired QPL and the main change in the wake of the COVID-19 pandemic.
ConclusionsFemale dermatologists reported heavier workloads. Heavy caseloads and more remote work were the main changes identified after the COVID-19 pandemic. Heavy caseloads have a significant impact on the QPL of dermatologists in Spain. Reducing caseloads would improve general job satisfaction and quality of care provision.
La calidad de vida profesional se define como el bienestar derivado del equilibrio entre las exigencias del ámbito laboral y los recursos para afrontarlas, el deterioro de la calidad de vida profesional puede contribuir en el síndrome de burnout o del profesional quemado. El objetivo de este estudio consiste en evaluar mediante cuestionario validado la calidad de vida profesional de los dermatólogos españoles.
Material y métodosSe diseñó un estudio transversal que incluyó dermatólogos españoles que respondieran a un formulario autoadministrado enviado a través de aplicaciones de mensajería online. El formulario incluyó datos sociodemográficos, 3 preguntas de respuestas abiertas y el Cuestionario de Calidad de Vida Profesional (CVP-35).
ResultadosSe incluyó a 106 participantes en este estudio, siendo un 58% (62/106) mujeres. La edad media fue de 41 años (intervalo de confianza [IC] del 95%: 43,3-38,8). Las puntuaciones para el dominio «carga de trabajo» de CVP-35 fueron superiores en las mujeres (p=0,02) y en los jefes de servicio (p=0,005). La presión asistencial fue el tema tratado con más frecuencia como factor limitante de la calidad de vida laboral, y el principal cambio identificado tras la pandemia de COVID-19.
ConclusionesEn nuestro estudio las mujeres refirieron una mayor carga de trabajo. El incremento de carga asistencial y de trabajo a distancia fueron los principales cambios por la pandemia de COVID-19. La presión asistencial es una gran limitante de la calidad de vida profesional de nuestros compañeros, reducirla mejoraría la satisfacción diaria y la calidad asistencial.
Professional quality of life (ProQOL) is defined as the well-being derived from the balance between the demands of the working environment and the resources available (psychological, organizational, and social) to cope with them.1 An imbalance between these factors can lead to work-related stress, which, if sustained over time, can contribute to the development of the so-called burnout syndrome:2 a psychological syndrome in response to “chronic interpersonal tensions at work” that can lead to “unrelenting exhaustion, feelings of cynicism and detachment from work, and a sense of inefficacy and depersonalization.”3 On the other hand, the degree of job satisfaction among health professionals is related to the quality of care provided,1,2 which is why job satisfaction consistently appears in every assessment of the overall quality of an organization.1,2,4
The fact that schedules are often more compatible with out-of-hospital life and that the number of critical patients is lower compared to that of other medical specialties creates the illusion that the ProQOL in dermatology is so good that dermatologists cannot suffer from the so-called burnout syndrome.5 However, while it is true that burnout rates are lower in dermatology compared to other medical specialties, the prevalence remains increasingly high.6 Beyond having a schedule compatible with our interests outside of medicine, factors such as the progressive bureaucratization of medical work and the increasing use of technology in day-to-day activities are also present in the daily routine of dermatologists, negatively impacting their quality of work life and having been identified as contributing factors to burnout in our specialty.6
While several studies have examined ProQOL in health professionals in Spain,1,2,7,8 there is limited information on the ProQOL of dermatologists in our field of expertise. Therefore, the objective of this study is to evaluate the ProQOL of Spanish dermatologists and the main changes experienced during the COVID-19 pandemic.
Materials and methodsDesign: This was cross-sectional study of dermatologists (both medical specialists and residents) who responded to a self-administered questionnaire sent via online instant messaging applications during February 2022.
Inclusion criteria: Being a medical specialist or medical resident in medical-surgical dermatology and venereology and practicing in Spain during the study period.
Exclusion criteria: Refusal to participate in the study, submitting the completed questionnaire more than once.
Measurement instrument: The CVP-35 questionnaire (CVP-35) was used to assess ProQOL. The CVP-35 has been validated in Spanish to be used with doctors (including medical residents) and to be sent via online.3,9 The CVP-35 scale assesses ProQOL through 35 questions scored from 0 to 10; these questions are categorized into 3 domains: workload, support from supervisors, and intrinsic motivation. Question #34 is independent and assesses the overall quality of the job at stake. The scores given to each question can be categorized as “none” (1 and 2), “some” (3, 4, and 5), “quite a bit” (6, 7, and 8), and “a lot” (9 and 10).1.
Thematic analysis: The questionnaire included 3 short questions on changes occurred in the work environment following the COVID-19 pandemic—the main limitation to ProQOL—and changes that participants would implement to improve their ProQOL. The answers were analyzed by 2 independent researchers and coded by common themes found. In case of disagreement while coding a response, a third researcher was called to solve the mismatch.
Statistical analysis: Data were analyzed using the SPSS® statistical software package for Windows, version 24.0 Chicago: SPSS Inc. Quantitative variables were compared using the ANOVA test, with Tukey's HSD post hoc correction test. Qualitative variables were compared using the chi-square test. P values <.05 were considered statistically significant in two-tailed tests.
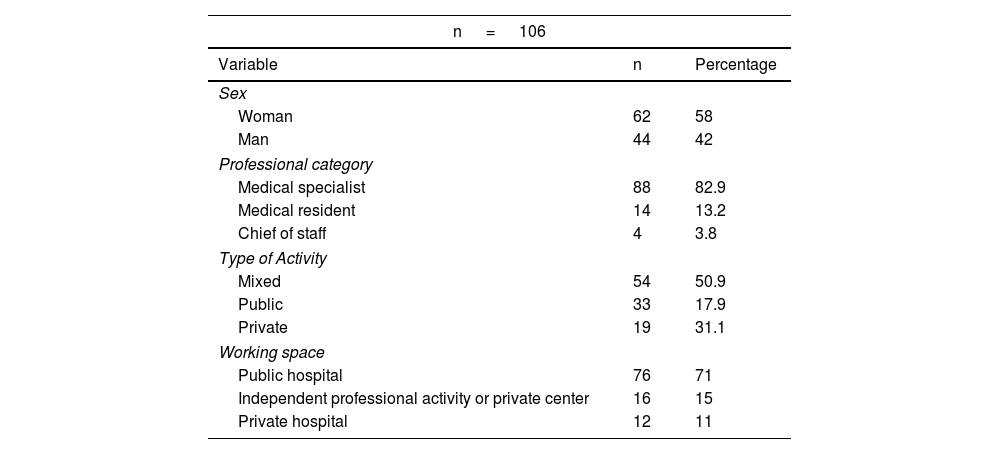
ResultsThis study included a total of 106 participants, 62 of whom were women (58.5%). The mean age was 42 years (range, 25-66). The most common professional category was medical specialist (82.9%, 88/106), and the most common medical practice was a mixed format (50.9%, 54/106). A total of 71% of respondents (76/106) spent most of their time working in public hospitals. The mean weekly working hours were 41 (10.1) The descriptive results of the sample are shown in Table 1. Sixty-three participants gave the name of the province in which they practiced [most came from Madrid (23.8%, 15/63), followed by Granada (19%, 12/63)].
Distribution of sociodemographic variables.
| n = 106 | ||
|---|---|---|
| Variable | n | Percentage |
| Sex | ||
| Woman | 62 | 58 |
| Man | 44 | 42 |
| Professional category | ||
| Medical specialist | 88 | 82.9 |
| Medical resident | 14 | 13.2 |
| Chief of staff | 4 | 3.8 |
| Type of Activity | ||
| Mixed | 54 | 50.9 |
| Public | 33 | 17.9 |
| Private | 19 | 31.1 |
| Working space | ||
| Public hospital | 76 | 71 |
| Independent professional activity or private center | 16 | 15 |
| Private hospital | 12 | 11 |
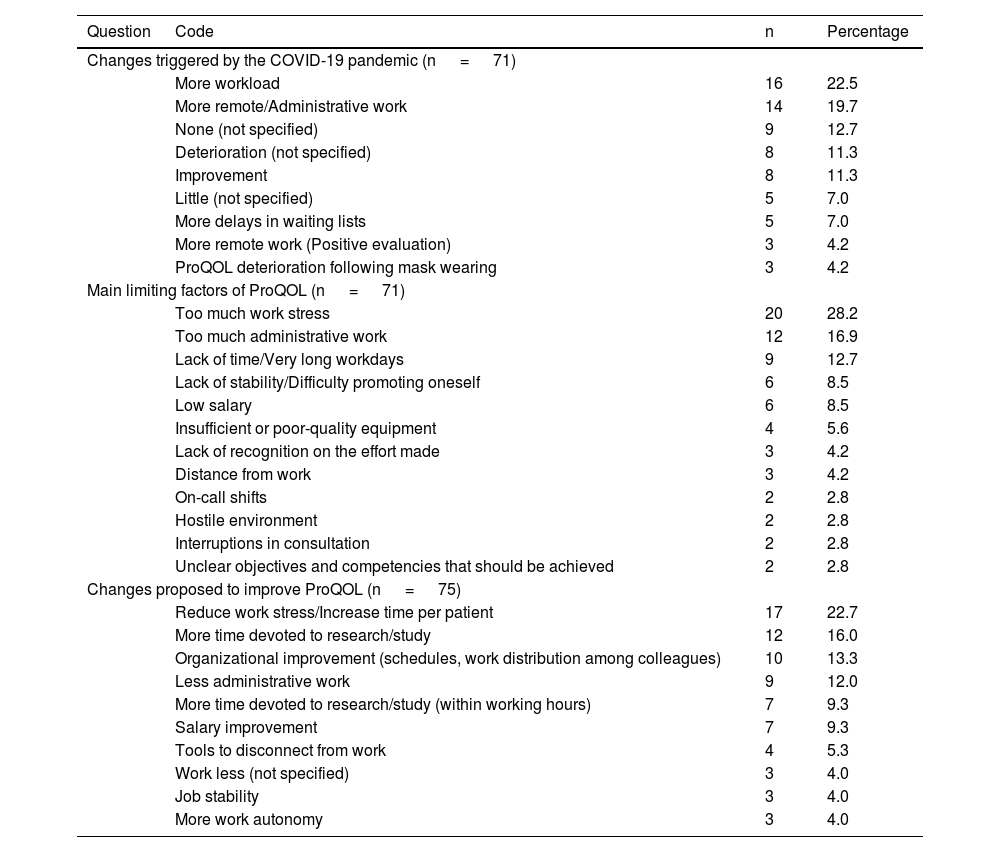
In the thematic analysis of responses to the 3 short questions asked, the main change triggered by the COVID-19 pandemic was an increased workload, followed by more remote work. The most limiting factor for ProQOL identified was excessive work stress, followed by excessive administrative work. Finally, the main changes proposed by the participants to improve their ProQOL were to reduce their workload and increase the time allocated for research and study. The different codes associated with the different thematic responses and the number of responses assigned to them can be found in Table 2.
Codes of the responses given according to identified themes.
| Question | Code | n | Percentage |
|---|---|---|---|
| Changes triggered by the COVID-19 pandemic (n = 71) | |||
| More workload | 16 | 22.5 | |
| More remote/Administrative work | 14 | 19.7 | |
| None (not specified) | 9 | 12.7 | |
| Deterioration (not specified) | 8 | 11.3 | |
| Improvement | 8 | 11.3 | |
| Little (not specified) | 5 | 7.0 | |
| More delays in waiting lists | 5 | 7.0 | |
| More remote work (Positive evaluation) | 3 | 4.2 | |
| ProQOL deterioration following mask wearing | 3 | 4.2 | |
| Main limiting factors of ProQOL (n = 71) | |||
| Too much work stress | 20 | 28.2 | |
| Too much administrative work | 12 | 16.9 | |
| Lack of time/Very long workdays | 9 | 12.7 | |
| Lack of stability/Difficulty promoting oneself | 6 | 8.5 | |
| Low salary | 6 | 8.5 | |
| Insufficient or poor-quality equipment | 4 | 5.6 | |
| Lack of recognition on the effort made | 3 | 4.2 | |
| Distance from work | 3 | 4.2 | |
| On-call shifts | 2 | 2.8 | |
| Hostile environment | 2 | 2.8 | |
| Interruptions in consultation | 2 | 2.8 | |
| Unclear objectives and competencies that should be achieved | 2 | 2.8 | |
| Changes proposed to improve ProQOL (n = 75) | |||
| Reduce work stress/Increase time per patient | 17 | 22.7 | |
| More time devoted to research/study | 12 | 16.0 | |
| Organizational improvement (schedules, work distribution among colleagues) | 10 | 13.3 | |
| Less administrative work | 9 | 12.0 | |
| More time devoted to research/study (within working hours) | 7 | 9.3 | |
| Salary improvement | 7 | 9.3 | |
| Tools to disconnect from work | 4 | 5.3 | |
| Work less (not specified) | 3 | 4.0 | |
| Job stability | 3 | 4.0 | |
| More work autonomy | 3 | 4.0 | |
ProQOL, professional quality of life.
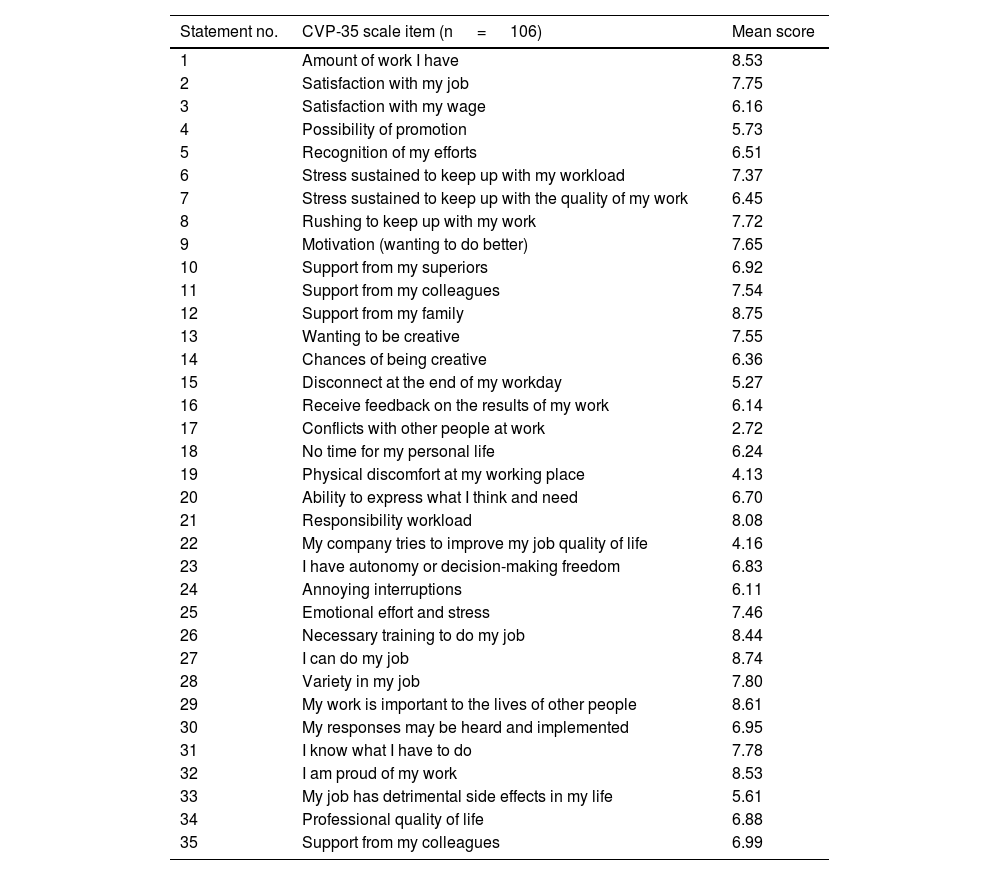
Regarding the results obtained by domain in the CVP-35 scale (Table 3), support from supervisors had a mean score of 6.58 points (1.67), which could be interpreted as quite a bit of support from the supervisors. The workload domain had a mean score of 6.4 points (1.2, quite a bit of workload), while the intrinsic motivation domain had the highest score of all with 8.25 points (1, quite a bit of intrinsic motivation). Regarding the extreme scores of each domain for supervisor support, the highest-scored item was “variety in my work” (7.8 ± 1.9 points), and the lowest-scored one, “my company tries to improve the quality of my job” (4.24 ± 2.8 points). Regarding the workload domain, the highest-scored item was “amount of work I have” (8.6 ± 1.18 points), and the lowest-scored one, “conflicts with other people” (2.7 ± 2.27 points). In the motivation domain, the highest-scored item was “support from my family” (8.75 ± 1.5 points), and the lowest-scored one, “desire to be creative” (7.54 ± 2 points). The independent question “quality of my professional life” scored a mean 6.9 (2.12) points.
Mean scores for each item of the CVP-35 questionnaire.
| Statement no. | CVP-35 scale item (n = 106) | Mean score |
|---|---|---|
| 1 | Amount of work I have | 8.53 |
| 2 | Satisfaction with my job | 7.75 |
| 3 | Satisfaction with my wage | 6.16 |
| 4 | Possibility of promotion | 5.73 |
| 5 | Recognition of my efforts | 6.51 |
| 6 | Stress sustained to keep up with my workload | 7.37 |
| 7 | Stress sustained to keep up with the quality of my work | 6.45 |
| 8 | Rushing to keep up with my work | 7.72 |
| 9 | Motivation (wanting to do better) | 7.65 |
| 10 | Support from my superiors | 6.92 |
| 11 | Support from my colleagues | 7.54 |
| 12 | Support from my family | 8.75 |
| 13 | Wanting to be creative | 7.55 |
| 14 | Chances of being creative | 6.36 |
| 15 | Disconnect at the end of my workday | 5.27 |
| 16 | Receive feedback on the results of my work | 6.14 |
| 17 | Conflicts with other people at work | 2.72 |
| 18 | No time for my personal life | 6.24 |
| 19 | Physical discomfort at my working place | 4.13 |
| 20 | Ability to express what I think and need | 6.70 |
| 21 | Responsibility workload | 8.08 |
| 22 | My company tries to improve my job quality of life | 4.16 |
| 23 | I have autonomy or decision-making freedom | 6.83 |
| 24 | Annoying interruptions | 6.11 |
| 25 | Emotional effort and stress | 7.46 |
| 26 | Necessary training to do my job | 8.44 |
| 27 | I can do my job | 8.74 |
| 28 | Variety in my job | 7.80 |
| 29 | My work is important to the lives of other people | 8.61 |
| 30 | My responses may be heard and implemented | 6.95 |
| 31 | I know what I have to do | 7.78 |
| 32 | I am proud of my work | 8.53 |
| 33 | My job has detrimental side effects in my life | 5.61 |
| 34 | Professional quality of life | 6.88 |
| 35 | Support from my colleagues | 6.99 |
When the association between the different domains of the CVP-35 scale and the sociodemographic variables was analyzed, we found that being chief of staff was associated with higher workload scores (P=.005), same as being a woman (P=.02) (Fig. 1). No significant differences were found between domain scores and the type of hospital, province, or contract.
DiscussionIn our study, most participants were attending physicians who practiced in a mixed activity format and developed most of their work in public hospitals. Work stress was identified as the main factor limiting ProQOL—the primary change experienced during the pandemic—and the main factor that should be addressed. Intrinsic motivation was the highest-scored domain in the CVP-35 scale, although scores in all 3 domains were high.
The primary change identified after the COVID-19 pandemic was an increased pressure at work and remote work. Post-pandemic increased pressure at work has been reported by health professionals across several studies.10–12 Also, we should mention that the increased amount of remote work has often been identified as a negative change, unlike what health care workers from other studies have reported in the past.12 More pressure at work has been identified as the main limitation of ProQOL, followed by excessive bureaucratic/administrative work, being administrative tasks identified by dermatologists—both residents and attending physicians—as a factor limiting ProQOL in former studies,.5,6,13,14 After reducing pressure at work, the participants from our study suggested increasing the time allocated to research to improve their ProQOL, since the lack of time for research had already been identified by dermatologists as a factor limiting the quality of work.14
The scores obtained for the 3 domains of the CVP-35 scale were higher than those identified when the questionnaire was submitted to primary care colleagues in our setting.1,15–17 Differences were more pronounced in the supervisor support domain (6.58 in our study vs 4.66; 4.78; 4.8),1,15,16 while the scores obtained in the workload domain were similar to those reported by primary care physicians (6.4 vs 6.4; 6.03; 6.06).1,15,16 The highest-scored domain was intrinsic motivation for Spanish dermatologists and primary care physicians alike.1,15,17 We should mention that many of the studies that used the CVP-35 scale in primary care were conducted before the pandemic, so the limiting factors of ProQOL and the changes experienced at work could not be the same.
In our study, being chief of staff was associated with a higher reported workload score compared to other professional categories. This result is consistent with a study that used the CVP-35 questionnaire among Spanish primary care physicians.1 In this study, residents did not report a higher workload compared to the remaining categories, as seen in a systematic review of 41 articles that evaluated the burnout syndrome in surgical specialties.18 Other publications, however, have found a reverse correlation between age or years worked and the professional burnout syndrome.19,20 Since an increased administrative workload was seen as a limiting factor of ProQOL by our participants, it seems reasonable to believe that the chiefs of staff have a higher volume of administrative/organizational responsibilities, which may explain the higher workload score reported by the latter. We should mention that, despite the statistical significance of the results, the number of chiefs of staff is small, meaning that further studies will be needed to confirm our findings.
The workload score reported was higher in women. Within the scientific literature reviewed, we only found 1 publication with results that were consistent with ours.21 Contrary to the aforementioned findings, numerous studies have debunked the notion that women have a lower quality of life, or more chances of experiencing the burnout syndrome.1,18,22,23
In addition to the inherent limitations of a cross-sectional design, our study had a limited participant recruitment period, as well as a limited participation in short questions. Also, the use of online messaging services may have biased the characteristics of all participants. Finally, the overlapping sociodemographic variables such as the professional category or the workplace may have also blurred the boundaries between those who work exclusively in the private sector and those from the public sector, thus complicating the identification of statistically significant differences. We think it is necessary to conduct additional studies with larger participant samples, including tools to diagnose the burnout syndrome, and assess anxiety and depression to analyze the potential association between ProQOL and its psychological impact on dermatologists.
ConclusionsIn our study, being a woman was associated with a higher reported workload, although we did not find consistent support in the medical literature currently available on gender differences. Work stress is the main change identified after the COVID-19 pandemic—the main limiting factor of ProQOL—and the primary change that should be addressed. Surveyed dermatologists reported a significant workload, but also considerable supervisor support and even higher intrinsic motivation to work. The periodic use of validated instruments to determine ProQOL is useful to identify room for improvement in the workplace.