Neurocristic harmatoma is a type of dermal melanocytosis that includes various pigmented lesions resulting from the abnormal development of neural crest melanocytes that migrate to the dermis.1
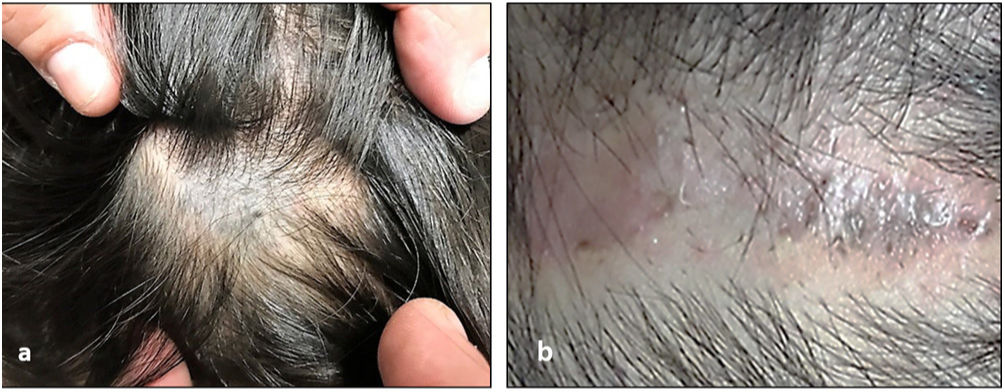
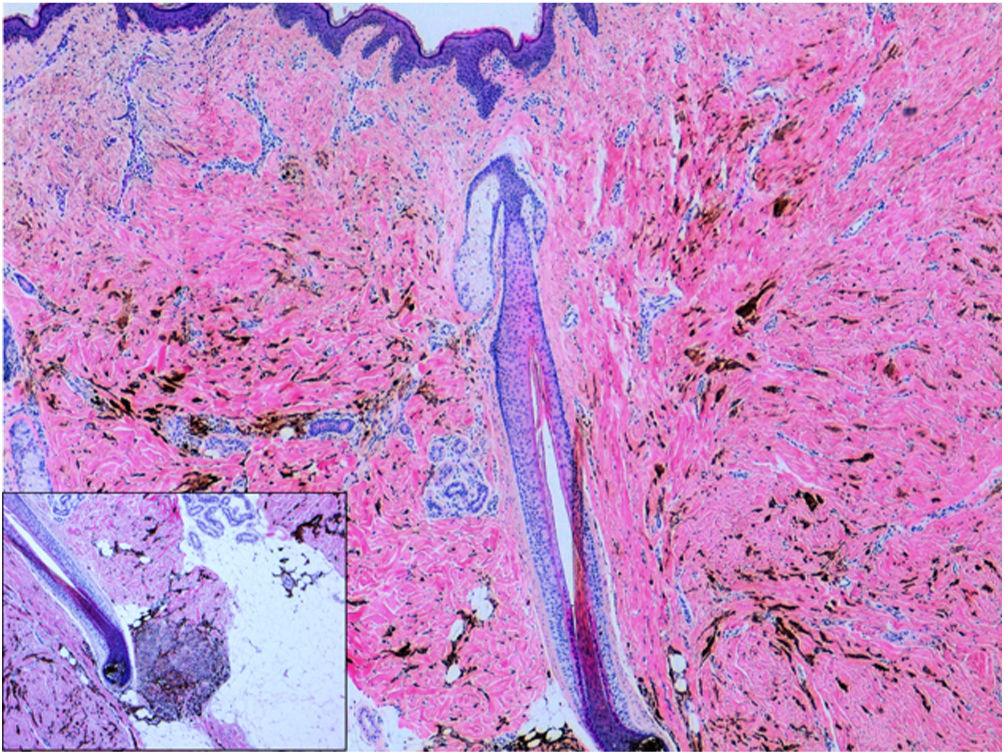
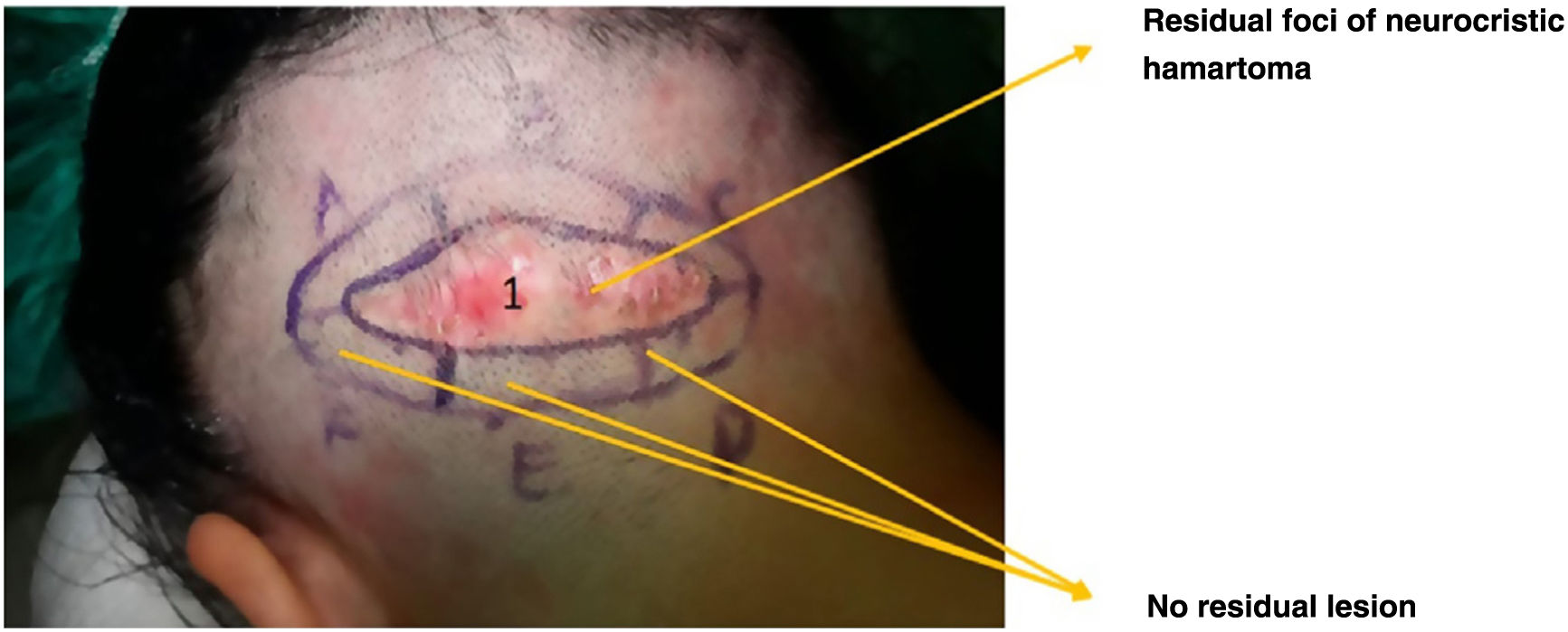
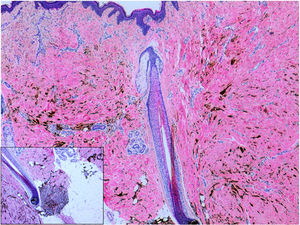
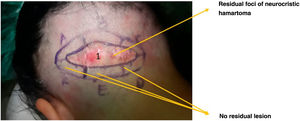
A 9-year-old girl attended the clinic for complete excision of a poorly defined, grayish-blue, plaque-type lesion on the occipital area of the scalp. It was unknown when the lesion first appeared, and there were no associated signs or symptoms (Fig. 1A). A previous attempt had been made to remove the lesion (Fig. 1B). Histology revealed neurocristic hamartoma that reached the borders, based on a previous biopsy that had led to a diagnosis of blue nevus with areas of dermal melanosis. After discussion with dermatology and histopathology, we performed no further tests and, in light of the histology findings (Fig. 2), we opted for excision using slow Mohs surgery owing to the size of the lesion (6cm×3cm), with placement of a skin graft. After removal with Mohs surgery (Fig. 3) and verification of the tumor-free margins, the wound was closed without tension 5 months later (Fig. 4A–D). No recurrences were observed in the following 2 years.
Neurocristic hamartoma mainly affects the scalp, although it can affect other parts of the body surface.2 It is a rare condition that should be differentiated from other pigmented lesions such as melanotic schwannoma and neurofibroma, pigmented dermatofibrosarcoma, and desmoplastic malignant melanoma.3 It may be bluish in color, as in the present case, and is sometimes confused with blue nevus, although unlike blue nevus, neurocristic hamartoma can transform to melanoma over a variable period of time (from 1 to 67 years).4
Therefore, the evaluation of “blue lesions” in association with dermal melanosis should always include an analysis of clinical and dermoscopy findings. Moreover, in the case of an absence of correlation, increase in size, difficulty for follow-up, or, as in the patient we report here, suspicion of malignancy, complete excision is mandatory.3
Histology findings vary from one case to another, although highly pigmented dendritic melanocytes are always found in the dermis, with a characteristic follicular distribution. These cells are stained using immunohistochemistry (e.g., protein S-100 or HMB45), which are useful for defining the borders of the lesion and ensuring complete excision.
Mohs micrographic surgery is the treatment of choice for many cutaneous tumors, since it enables optimal preservation of healthy tissue with a sufficient safety margin, thus minimizing the possibility of recurrence. It is particularly useful in tumors in which local growth is destructive, for example, basal cell and squamous cell carcinoma on cosmetically and functionally sensitive areas such as the H-zone of the face, especially on the eyelids, nose, and cheeks. This approach is also useful for management of tumors in immunodepressed patients or in lesions with poorly defined margins,5 as in the present case.
Despite its advantages over conventional surgery, micrographic surgery is rarely used in children, although it has the same indications as for adults.5–7
In children, cutaneous neurocristic hamartoma should be included in the differential diagnosis of a “bluish” plaque on the scalp. The first step should involve biopsy. If the histology result is positive, complete surgical resection should be performed. Slow Mohs surgery could be an excellent therapeutic approach.
Conflicts of InterestThe authors declare that they have no conflicts of interest.