Deep dissecting hematomas and necrotizing fasciitis require early debridement, often leading to large skin defects.1,2 Closure of these ulcers by secondary intention usually entails painful dressing changes and delays complete resolution. Topical negative pressure (TNP) therapy has been classically used to promote the formation of granulation tissue and improve the ulcer bed, but is also useful to secure skin grafts.3 Application of negative pressure to the graft can increase adhesion, remove exudate, and reduce maceration.4 We present 4 cases of patients with ulcers on the legs who underwent this technique after debridement of a deep dissecting hematoma or necrotizing fasciitis.
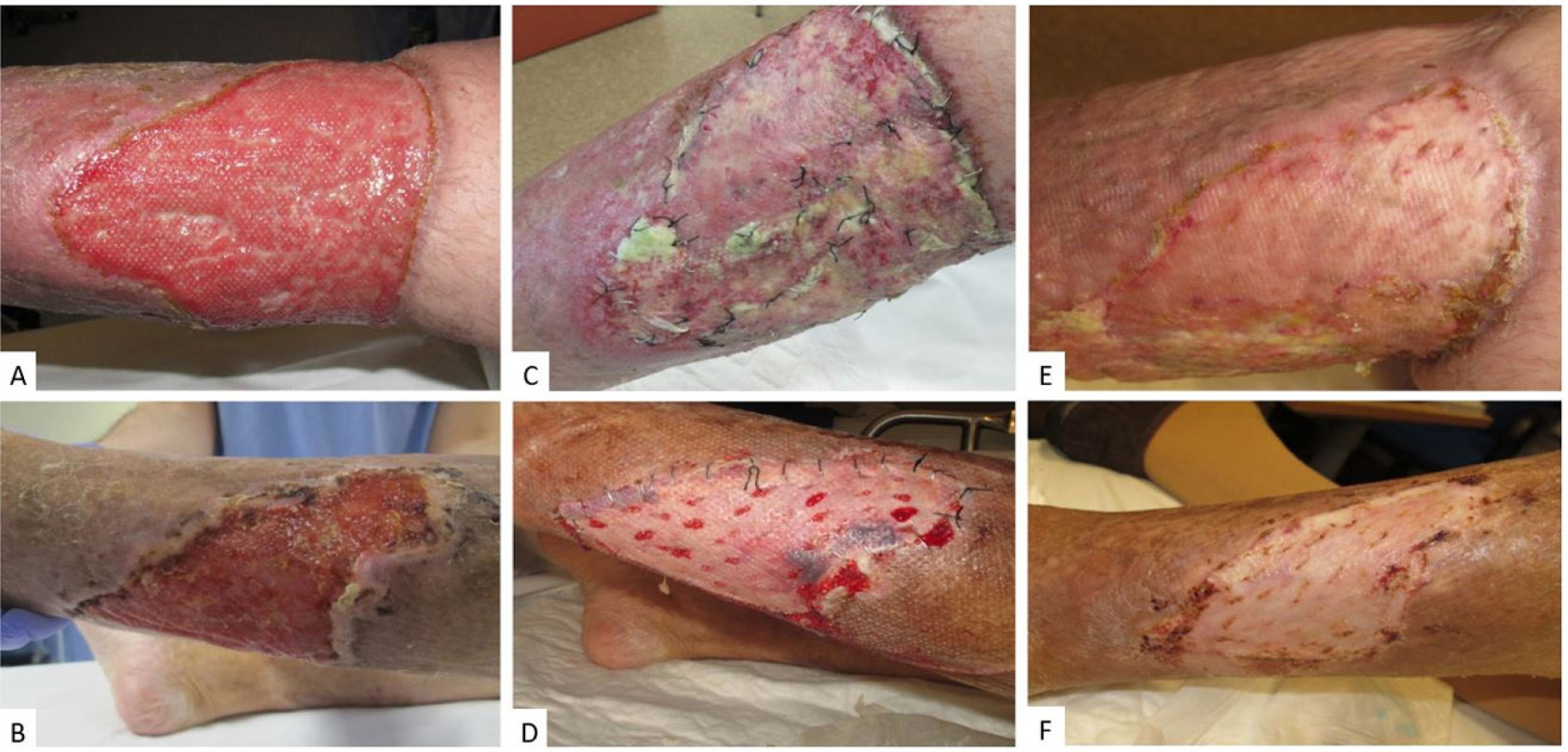
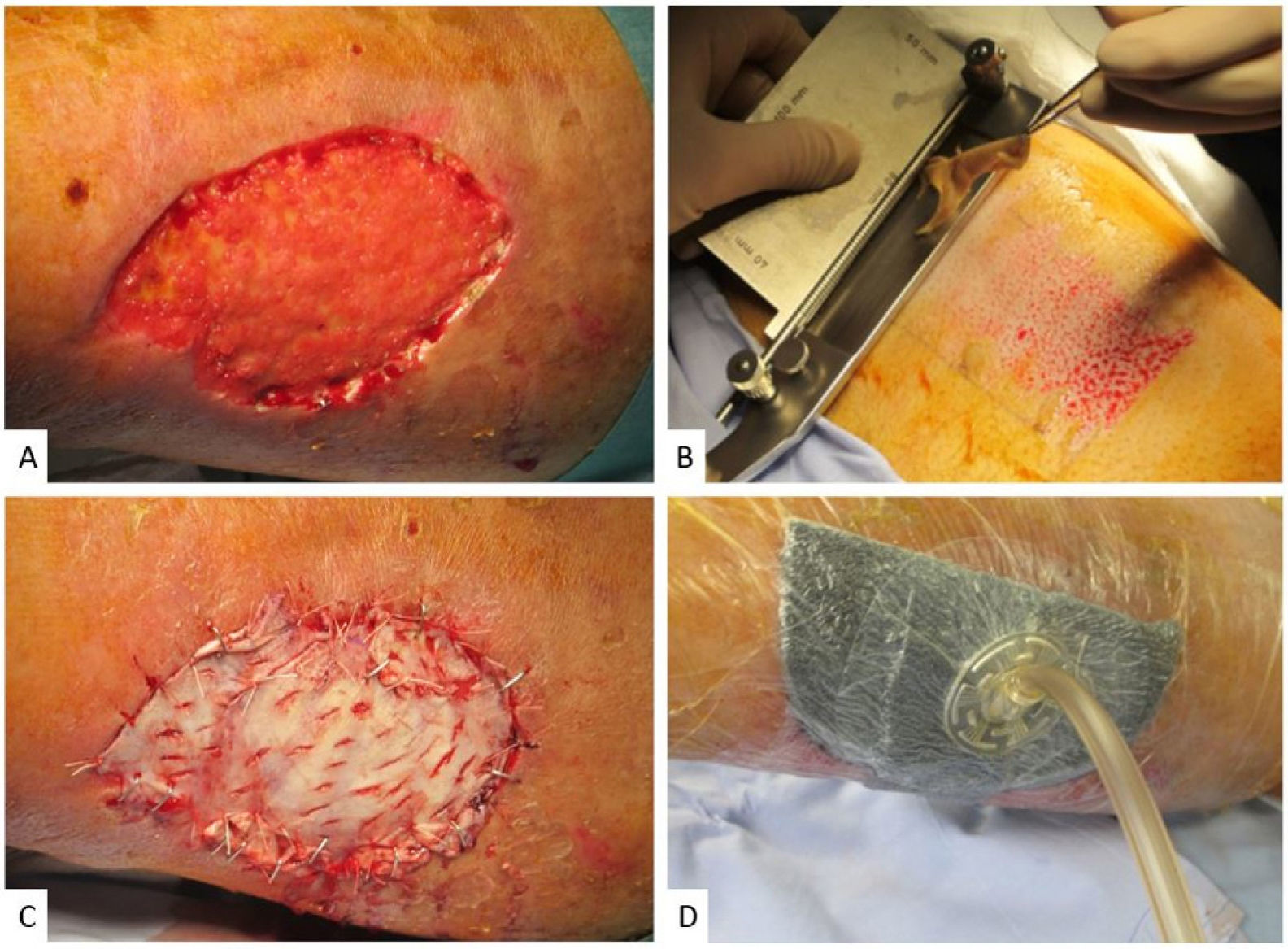
The characteristics of the patients, their ulcers, and the type of graft are shown in Table 1. All patients had ulcers on the legs that ranged in size from 65cm2 to 210cm2 (Fig. 1A, B). The type of graft was selected according to the size of the ulcer and the experience of the dermatologist. A lamellar graft was used in 3 of the 4 cases. A nonadhesive dressing (Atrauman) was applied and the entire area was sealed with a TNP system (VAC [vacuum assisted closure]; Fig. 2). The TNP system was programmed at a continuous pressure of −75mmHg. All patients were hospitalized for 5 days, without requiring any additional cure. On the fifth postoperative day, the TNP system was removed and the patients were switched to an alternate-day outpatient schedule using conventional dressings and compression, depending on the appearance of the graft. In all patients, the graft took on the fifth day (Table 1, Fig. 1C and D) and complete resolution of the ulcer was achieved by postoperative day 30 (Fig. 1E and F). Complications occurred in 3 of the 4 patients, and were minor in 2 cases, as summarized in Table 1. In Patient 2 the donor site became infected with Pseudomonas aeruginosa, which was treated with silver dressings and oral ciprofloxacin and had no impact on the final outcome of the intervention.
Patient Characteristics, Type of Ulcer, and Complications.
| Patient | Sex | Age | Cause of defect | OAC | Other | Size/area | Previous TNP | Graft type | Viable graft | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 91 | Deep dissecting hematoma | Yes | AHTDL | 12×10cm/120cm2 | Yes | Lamellar | Yes | Maceration of the margins |
| 2 | M | 79 | Necrotizing fasciitis | Yes | AHTCVI | 15×14cm/210cm2 | Yes | Lamellar | Yes | Infection of donor site with P. aeruginosa |
| 3 | F | 85 | Deep dissecting hematoma | Yes | AHTDMCKDPAD | 13×5cm/65cm2 | None | Full thickness | Yes | Donor-site hematoma |
| 4 | M | 57 | Necrotizing fasciitis | No | AHTCVI | 12.5×7cm/87.5cm2 | Yes | Lamellar | Yes | None |
Abbreviations: AHT, arterial hypertension; CKD, chronic kidney disease; CVI, chronic venous insufficiency; DL, dyslipidemia; DM, diabetes mellitus; F, female; M, male; OAC, oral anticoagulants; PAD, peripheral arterial disease; TNP, topical negative pressure.
Surgical debridement of deep dissecting hematoma and necrotizing fasciitis results in large, usually full-thickness skin defects. Repair of the lost tissue is initiated by granulation tissue, which permits subsequent epithelial covering.5 TNP can be used to stimulate the formation of granulation tissue,6 while skin grafts replace the epithelial lining and accelerate the healing process.7 It is therefore essential to know how to maximize graft viability while minimizing surgical complications. The pressure and duration of TNP on the graft are the main variables in this technique. Data indicate that a continuous negative pressure of −75mmHg on skin grafts causes less inflammation and increases fibrinogen production compared with higher pressures or no pressure at all.8 However, there are no data to indicate the optimal duration of TNP on the graft. In the majority of cases, TNP is removed between 4 and 7 days after the intervention.7
The increase in cost with respect to a conventional graft without TNP is around $400 (€338.72).9 The value of this approach is that is allows for reductions in other costs (e.g. those associated with increased admission time and repeated surgical interventions). A recent meta-analysis showed that TNP increases the likelihood of graft viability and reduces the rate of reoperation.10 However, these results should be interpreted with caution given the heterogeneity of the studies included in this meta-analysis, and in particular the variability in ulcer etiology across studies.
The main limitations of our study are the small patient population and the absence of a control group.
In summary, we present 4 cases in which a skin graft was fixed with TNP in patients with ulcers secondary to deep dissecting hematoma or necrotizing fasciitis. This is a simple procedure based on techniques that are familiar to dermatologists, and constitutes an alternative to the traditional technique. However, more studies are required to confirm its efficacy and efficiency in this type of ulcer.