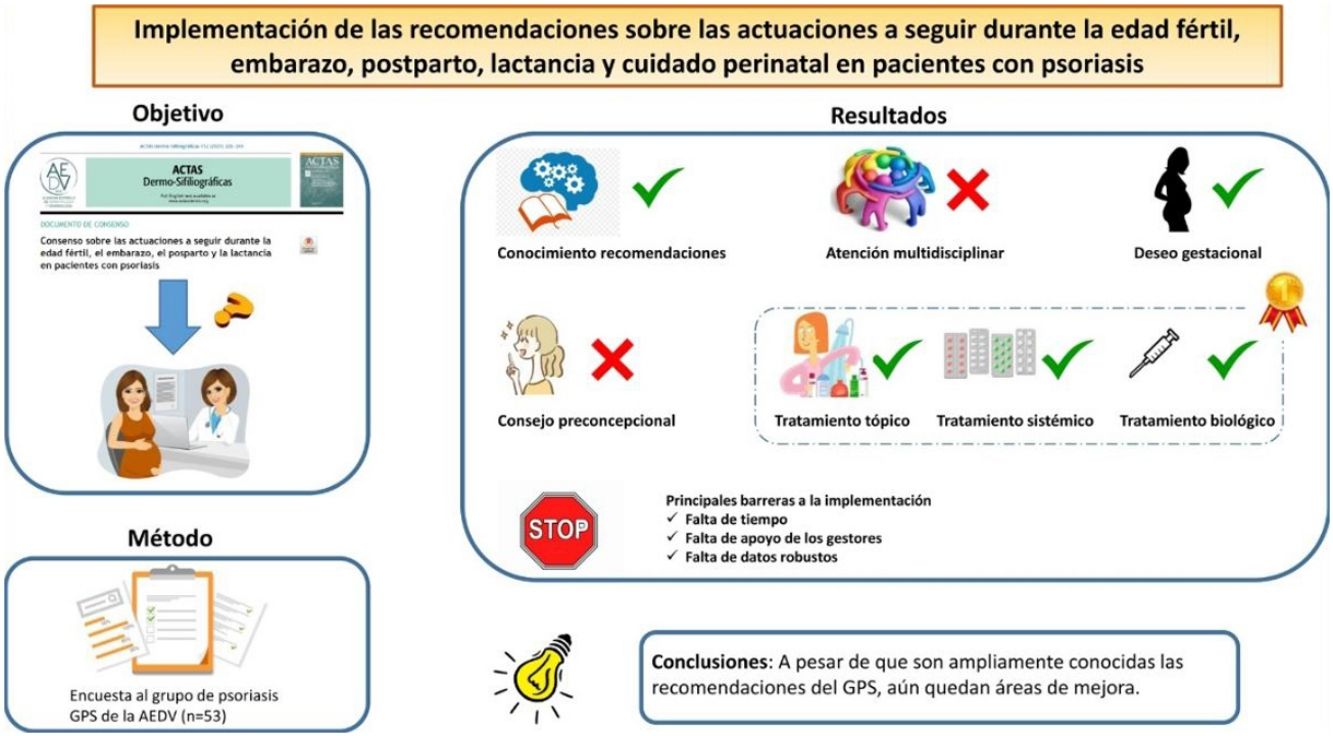
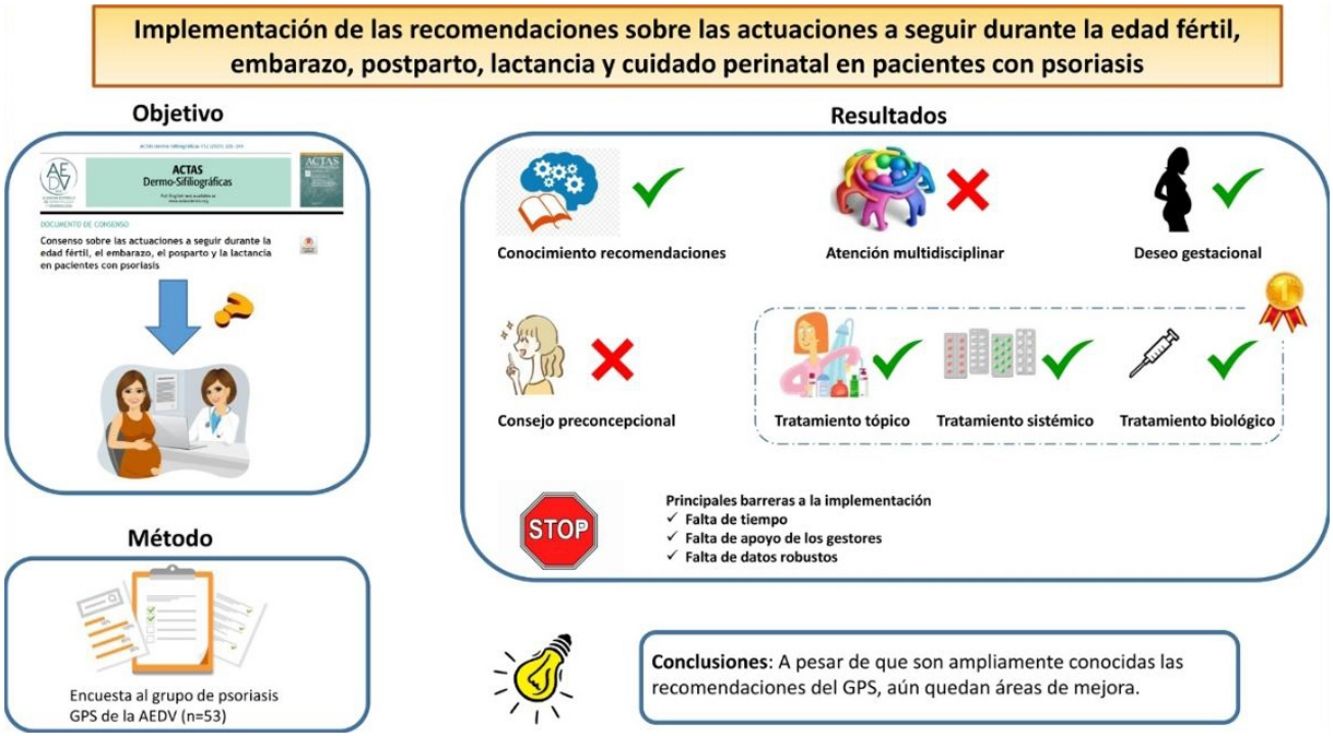
To analyze degree of implementation of recommendations on the management of psoriasis during preconception, pregnancy, postpartum, breastfeeding, and perinatal care published by the Psoriasis Working Group of the Spanish Academy of Dermatology and Venereology (AEDV).
MethodsWe designed a structured online survey consisting of closed questions. A link was emailed to all the members of the Psoriasis Working Group to collect their anonymous responses. We also collected sociodemographic, professional, and practice-related data related to the goals of the study and then compiled descriptive statistics to analyze the survey findings.
ResultsWe received 53 responses for analysis. Overall, 96% of respondents were familiar with the recommendations, but very few of them worked in multidisciplinary maternity care units or had access to specific protocols on the management of psoriasis before, during, and after pregnancy in their departments. Seventy percent of dermatologists regularly ask their patients about pregnancy plans, but only 46% ask both men and women. Women also receive more preconception advice than men (54% vs. 19%). Significant variations were observed in the type of advice given. Ninety percent of the dermatologists interrupt topical treatments during pregnancy, and nearly all suspend conventional systemic drugs with the exception of cyclosporin A. Most biologics are also being discontinued in the third trimester, with the exception of certolizumab pegol. Almost all the respondents indicated that they use topical treatments, phototherapy, and certolizumab pegol in breastfeeding mothers. The main barriers to implementing the working group's recommendations are a lack of time, a lack of support, and a lack of robust data.
ConclusionsAlthough the AEDV psoriasis working group's recommendations are widely known, areas for improvement remain.
Analizar el grado de implementación de las recomendaciones del Grupo de Psoriasis (GPS) sobre las actuaciones a seguir durante la edad fértil, el embarazo, el posparto, la lactancia y el cuidado perinatal en la psoriasis.
MétodosSe diseñó y envió una encuesta cerrada, estructurada y anónima, en formato electrónico a miembros del GPS a través del correo electrónico. Se recogieron las variables sociodemográficas y profesionales de los participantes, y otras relacionadas con los objetivos propuestos. Se realizó un análisis descriptivo.
ResultadosSe analizaron 53 encuestas. El 96% de los participantes conocen las recomendaciones del GPS, pero su nivel de participación en unidades de atención multidisciplinar o la disposición de protocolos específicos en los servicios es muy baja. El 70% pregunta de forma regular sobre el deseo gestacional, aunque solo el 46% lo pregunta a varones y mujeres. Se ofrece consejo preconcepcional más a mujeres que a varones (54 vs. 19%). Gran variabilidad en cuanto a los consejos ofrecidos. El 90% suspende tratamientos tópicos durante el embarazo, y prácticamente el 100% los tratamientos sistémicos salvo la ciclosporina A. En el tercer trimestre se suspenden la mayoría de las terapias biológicas a excepción de certolizumab pegol. Los tratamientos tópicos, fototerapia y certolizumab pegol son usados casi por el 100% de los encuestados en la lactancia. La falta de tiempo, de apoyo de los gestores y de datos robustos son las principales limitaciones a la implementación de las recomendaciones.
ConclusionesA pesar de que son ampliamente conocidas, las recomendaciones del GPS aún quedan áreas de mejora.
Psoriasis is a very common chronic inflammatory disease that can affect both fertility and pregnancy, postpartum, and breastfeeding (and vice versa).1–4
Several studies have described a possible association between psoriasis and fertility problems in both men and women.5–7 In the case of pregnancy, an estimated 40% to 88% of women experience a worsening of psoriasis several weeks after giving birth.8 In addition, children born to mothers who have been treated with monoclonal antibodies that cross the placental barrier during the third trimester are at an increased risk of infection and require specific monitoring and management.9 Finally, some of the treatments used in psoriasis, including tazarotene and acitretin, are potentially teratogenic and are therefore contraindicated in pregnancy.10,11
Health care professionals involved in the care of psoriasis patients must have detailed knowledge of the above and have the necessary expertise and skills to prevent or treat problems both early and efficiently.12 These issues are also very relevant to patients.12 In view of the above, the Psoriasis Working Group (GPs in its Spanish acronym) of the Spanish Academy of Dermatology and Venereology (AEDV) published a consensus statement in 2020 containing recommendations aimed at improving the management of patients of reproductive age. The recommendations covered aspects relating to fertility, pregnancy, postpartum, breastfeeding, and perinatal care.13
More than a year after the publication of this consensus statement, the GPs launched a survey to analyze the degree of implementation of its recommendations and examine perceived barriers and facilitators.
MethodologyThis study, initiated by the GPs, involved an online survey that was emailed to members of the GPs. It complied with good clinical practice standards and the ethical principles of the latest version of the Declaration of Helsinki regarding medical research involving human subjects.14
Survey Design and VariablesWe conducted a cross-sectional study using an anonymous online survey designed by a working group of 6 dermatologists with methodological support. The survey items were selected based on the 2020 GPs recommendations.13 The survey was then generated online (using SurveyMonkey) and consisted of a structured questionnaire with closed questions.
The survey was divided into sections to collect information on the following: 1) sociodemographic and professional characteristics of the respondents, including age, sex, place of residence (autonomous community), hospital (name and type), years working as a dermatologist, work in a dedicated psoriasis clinic; 2) general variables related to the management of psoriasis before, during, and after pregnancy, including participation in multidisciplinary maternity care units/teams; access to specific protocols in their departments; familiarity with national and international guidelines and recommendations; knowledge (rated on a scale of 1 [low] to 10 [high]) about the effects of pregnancy and postpartum on psoriasis, the effects of psoriasis on pregnancy (conception and course) and breastfeeding, and the teratogenic potential of common psoriasis drugs and their effects on breastfeeding; 3) variables related to actions taken prior to pregnancy, such as active inquiry about pregnancy plans and use of safe contraception; preconception counseling and types of advice; pregnancy planning; availability of protocols, documents, and guidelines on reproductive care and/or pregnancy planning; aspects that should be taken into account regarding a possible pregnancy; and provision of patient education material on preconception; 4) variables related to pregnancy and follow-up, including availability of related protocols, documents, and guidelines; changes to follow-up; provision of educational material on psoriasis and pregnancy; use of topical treatments, phototherapy, conventional systemic drugs (methotrexate, cyclosporin, acitretin, dimethyl fumarate), and biologics (tumor necrosis factor [TNF] inhibitors, interleukin [IL] 12/23 inhibitors, IL-17 inhibitors, IL-23 inhibitors, etc.); psoriasis control before and during pregnancy; and steps taken in the event of a flare-up during pregnancy; 5) variables related to postpartum, breastfeeding, and perinatal care, including changes to follow-up; use of drugs; adherence to specific protocols or documents; provision of patient education material and recommendations on breastfeeding and perinatal care; and 6) perceived barriers and facilitators to the implementation of the GPs recommendations.
Participant Selection and Survey DatesIn view of the characteristics of the survey and its goals, we selected a convenience sample of GPs, who were sent an email inviting them to answer the survey. They survey ran online from October 1 to October 31, 2021. The link was sent by email and was followed up with 2 reminders to increase the response rate.
Data Processing and Statistical AnalysisThe survey responses were downloaded from SurveyMonkey in an Excel spreadsheet (Microsoft Word) and analyzed in Stata 12 (Stata Corporation). The findings were summarized using descriptive data. Quantitative variables are expressed as mean (SD) and qualitative variables as numbers and percentages.
ResultsFifty-three dermatologists answered the survey. Their sociodemographic and professional characteristics are summarized in Table 1. In brief, 53% were women aged 46–55 years, 81% worked in a tertiary care hospital, and 79% worked in a dedicated psoriasis unit.
Sociodemographic and Clinical Data.
| Variable | Result |
|---|---|
| Female sex, No. (%) | 28 (53) |
| Current age, % | |
| 25–35 y | 15 |
| 36–45 y | 26 |
| 46–55 y | 30 |
| 56–65 y | 25 |
| >65 y | 4 |
| Type of hospital, No. (%) | |
| Primary care hospital (outpatient care) | 0 (0.00) |
| Secondary care hospital (regional hospital or specialized center) | 9 (17.31) |
| Tertiary care hospital (general hospital, referral hospital, hospital with a higher level of complexity) | 42 (80.77) |
| Private clinic | 1 (1.92) |
| Do not know | 0 (0.00) |
| Years working as a dermatologist, mean (SD) | 15 (2.83) |
| Working in dedicated psoriasis unit, No. (%) | 42 (79) |
The vast majority of respondents (96%) were familiar with the GPs recommendations on the management of psoriasis before, during, and after pregnancy, but just over 5% formed part of a multidisciplinary maternity care unit or team. Almost three-quarters reported a lack of specific protocols related to psoriasis and pregnancy in their departments. The use of educational material other than verbal advice and information, such as pamphlets, videos, and web-based tools, was uncommon. The dermatologists, however, were very knowledge about the effects of psoriasis on pregnancy and breastfeeding (and vice versa) and the effects of psoriasis treatments, with mean scores ranging from 7.70 (1.41) to 8.84 (0.71) on a scale of 1 to 10.
Preconception (Supplementary Data)Almost 71% of survey respondents routinely ask patients about pregnancy plans, but just 46% ask both men and women. Women are also more likely than men to be offered frequent (always or often) preconception advice (54% vs. 19%). The most common guidance provided was related to the effects of psoriasis and psoriasis treatments on pregnancy and postpartum (83% of those surveyed) and pregnancy planning (79%). Family planning discussions were more likely to be held with certain groups of patients, such as those on systemic treatments (64.5%), those who ask for advice (60.4%), and those with moderate to severe psoriasis (52%). Many of the respondents said that it is sometimes impossible to have these discussions, as the patient is often pregnant by the time she consults. Systemic treatments (including biologics) and severity of disease were highlighted as important aspects to consider in the management of psoriasis during preconception, and were mentioned by 94% and 83% of respondents, respectively.
Pregnancy (Supplementary Data)A majority of respondents considered that women should be in remission or have low disease activity before becoming pregnant (74%) and while pregnant (almost 85%).
Changes to follow-up are made in approximately 80% of pregnancies. The main steps taken following confirmation of pregnancy are discussions with the patient about the effects of pregnancy on psoriasis and vice versa (81%) and assessment of treatment (79%).
Almost 90% of those surveyed interrupt topical treatments during pregnancy, although the percentages varied significantly from one treatment to the next, with a range extending from 6.4% for topical corticosteroids to 81% for salicylic acid (Table 2). Nearly all the respondents suspend systemic treatments with the exception of cyclosporin A. None of them suspend narrowband UV-B phototherapy. Just 12% discontinue certolizumab pegol following confirmation of pregnancy or a wish to become pregnant. The rates for the other biologics varied, with 37% of respondents stating that they interrupt treatment when informed of the wish to become pregnant, 18% to 33% on confirmation of pregnancy, and 29% to 44% at the start of the third trimester (Table 3).
Management of Drugs in Pregnant Patients with Psoriasis.
| Variable | ResultNo. (%) |
|---|---|
| Topical treatments interrupted on confirmation of pregnancy | |
| Calcipotriol | 28 (59.57) |
| Salicylic acid | 38 (80.85) |
| Topical PUVA therapy | 35 (74.47) |
| Topical corticosteroids | 3 (6.38) |
| Topical calcineurin inhibitors | 24 (51.06) |
| I do not interrupt topical treatments | 4 (8.51) |
| I leave the decision to gynecologists/obstetricians | 0 (0.00) |
| Conventional systemic treatments/phototherapy interrupted on (or before) confirmation of pregnancy | |
| Acitretin and other systemic retinoids | 47 (100.00) |
| PUVA | 44 (93.62) |
| Narrowband UV-B | 0 (0.00) |
| Apremilast | 44 (93.62) |
| Dimethyl fumarate | 42 (89.36) |
| Methotrexate | 47 (100.00) |
| Cyclosporin A | 20 (42.55) |
| I do not interrupt systemic treatments | 0 (0.00) |
| I leave the decision to gynecologists/obstetricians | 0 (0.00) |
Abbreviation: PUVA, psoralen plus UV-A.
Interruption of Biologic Therapy in Pregnant Women.
| Drug | On confirmation of wish to become pregnantNo. (%) | On confirmation of pregnancyNo. (%) | Third trimesterNo. (%) | Not interrupted during pregnancyNo. (%) |
|---|---|---|---|---|
| Infliximab | 16 (37.21) | 11 (25.58) | 15 (34.88) | 1 (2.33) |
| Adalimumab | 15 (33.33) | 8 (17.78) | 20 (44.44) | 2 (4.44) |
| Etanercept | 16 (36.36) | 9 (20.45) | 18 (40.91) | 1 (2.27) |
| Certolizumab pegol | 2 (4.35) | 1 (2.17) | 3 (6.52) | 40 (86.96) |
| Ustekinumab | 16 (37.21) | 13 (28.89) | 15 (33.33) | 1 (2.22) |
| Secukinumab | 16 (37.21) | 15 (32.61) | 14 (30.43) | 1 (2.17) |
| Brodalumab | 16 (37.21) | 15 (32.61) | 13 (28.89) | 1 (2.22) |
| Ixekizumab | 16 (37.21) | 15 (32.61) | 14 (30.43) | 1 (2.17) |
| Guselkumab | 16 (37.21) | 15 (32.61) | 13 (28.89) | 1 (2.22) |
| Risankizumab | 16 (37.21) | 15 (32.61) | 13 (28.89) | 1 (2.22) |
| Tidrakizumab | 16 (37.21) | 15 (32.61) | 13 (28.89) | 1 (2.22) |
The main factors affecting treatment decisions in pregnant patients with psoriasis, rated on a scale of 1–5, are disease characteristics (mean, 4.28 [0.85]) and summary of product characteristic information (mean score, 4.21 [0.74]) (Table 4).
Factors That Influence Treatment Decisions in Pregnant Patients With Psoriasis and Their Weighting From 1 (Small) to 5 (Large).
| Variable | 1No. (%) | 2No. (%) | 3No. (%) | 4No. (%) | 5No. (%) | Mean (SD) |
|---|---|---|---|---|---|---|
| Patient characteristics | 0 (0.00) | 4 (8.70) | 4 (8.70) | 23 (50.00) | 15 (32.61) | 4.08 (0.86) |
| Psoriasis characteristics | 0 (0.00) | 1 (2.17) | 6 (13.04) | 21 (45.65) | 18 (39.13) | 4.21 (0.74) |
| Summary of product characteristics | 0 (0.00) | 2 (4.44) | 6 (13.33) | 14 (31.11) | 23 (51.11) | 4.28 (0.85) |
| International recommendations | 1 (2.17) | 0 (0.00) | 10 (21.74) | 20 (43.48) | 15 (32.61) | 4.04 (0.85) |
| National and regional recommendations | 0 (0.00) | 3 (6.67) | 11 (24.44) | 13 (28.89) | 18 (40.00) | 4.02 (0.95) |
| Hospital pharmacotherapeutic guidelines | 7 (15.91) | 10 (22.73) | 13 (29.55) | 6 (13.64) | 8 (18.18) | 2.95 (1.31) |
| Usual clinical practice in my department | 3 (6.82) | 6 (13.64) | 13 (29.55) | 13 (29.55) | 9 (20.45) | 3.43 (1.15) |
| Patient opinion | 2 (4.35) | 5 (10.87) | 6 (13.04) | 23 (50.00) | 10 (21.74) | 3.73 (1.05) |
Different options are used to treat flare-ups during pregnancy, including, in descending order of frequency, UV-B phototherapy, topical treatments, biologic treatments (certolizumab pegol), and cyclosporin A.
Postpartum and Breastfeeding (See Supplementary Data)Fifty-three percent of survey respondents systematically check for postpartum flare-ups, and 94% return to usual follow-up practices. Eighty-one percent recommend breastfeeding and almost 50% take specific steps to monitor children born to mothers exposed to biologic therapies (which cross the placental barrier throughout pregnancy or at least during the last trimester).
Drugs are largely not used to treat psoriasis during breastfeeding, with the exception of topical treatments (98%), narrowband UV-B therapy (100%), and certolizumab pegol (98%) (Table 5).
Drug use During Breastfeeding in Patients with Psoriasis.
| Variable | Results | |
|---|---|---|
| YesNo. (%) | NoNo. (%) | |
| Topical treatments | 45 (97.83) | 1 (2.17) |
| UV-B phototherapy | 45 (100.00) | 0 (0.00) |
| Acitretin and other systemic retinoids | 2 (4.88) | 39 (95.12) |
| PUVA therapy | 2 (4.88) | 39 (95.12) |
| Apremilast | 3 (7.32) | 38 (92.68) |
| Dimethyl fumarate | 1 (2.44) | 40 (97.56) |
| Methotrexate | 0 (0.00) | 41 (100.00) |
| Cyclosporin A | 10 (25.00) | 30 (75.00) |
| Infliximab | 12 (28.57) | 30 (71.43) |
| Adalimumab | 23 (52.27) | 21 (47.73) |
| Etanercept | 16 (38.10) | 26 (61.90) |
| Certolizumab pegol | 40 (97.56) | 4 (9.09) |
| Ustekinumab | 16 (37.21) | 27 (62.79) |
| Secukinumab | 15 (34.88) | 28 (65.12) |
| Brodalumab | 15 (34.88) | 28 (65.12) |
| Guselkumab | 15 (34.88) | 28 (65.12) |
| Ixekizumab | 15 (34.88) | 28 (65.12) |
| Risankizumab | 15 (34.88) | 28 (65.12) |
| Tildrakizumab | 15 (34.88) | 28 (65.12) |
| Whatever the pediatrician considers appropriate | 15 (45.15) | 18 (54.55) |
Abbreviation: PUVA, psoralen plus UV-A.
The main barriers and facilitators to the implementation of the GPs recommendations are summarized in Table 6. The main or most common barriers mentioned were a lack of time, a lack of robust data from clinical studies, particularly in relation to drug treatments, and a lack of support from health care managers/directors. The main facilitators mentioned were improved communication between disciplines, support from nursing staff, and development of educational material. The options considered easiest to implement were nursing support (36%) and educational material (23%).
Barriers to the Implementation of GPs Recommendations on Pregnancy, Postpartum, Breastfeeding, and Perinatal Care Rated on a Scale of 1 (Not a Common/Important Barrier) to 5 (Common/Important Barrier) and Facilitators Graded on a Scale Of 1 (Not an Important Need) to 5 (Very Important Need)a
| Barrier | Answer |
|---|---|
| Lack of dissemination of GPs consensus statement | 2.67±1.16 |
| Lack of knowledge about many aspects related to fertility, pregnancy, and breastfeeding | 2.71±1.17 |
| Lack of robust data from clinical studies, especially in relation to drug use | 3.38±1.17 |
| Lack of experience in the management of patients in this situation | 3.06±1.09 |
| Lack of time during visits | 3.41±1.26 |
| Little collaboration between disciplines | 3.32 (1.19) |
| Lack of support from health care managers/directors | 3.35 (1.04) |
| Loss to follow-up of pregnant patients (they go to the gynecologist/obstetrician and come back some time later after giving birth) | 2.93 (1.04) |
| Many of these aspects are not a dermatologist's responsibility | 2.61 (1.32) |
| Lack of resources in general | 3.06 (1.21) |
| Facilitators | Answer |
|---|---|
| Nursing support | 4.12 (0.92) |
| Greater communication between disciplines | 4.24 (0.69) |
| More specific training for dermatologists | 4.04 (0.84) |
| Development of patient education material | 4.08 (0.95) |
| Patient/patient association opinions | 3.26 (1.10) |
| Specific research projects, specific research records | 3.95 (0.95) |
| Development of local consensus-based protocols | 3.91 (0.98) |
| Greater support from new technologies (video calls, electronic medical records. etc.) | 3.34 (1.18) |
This survey was designed to analyze the degree of implementation of the 2020 GPs recommendations on the management of cutaneous psoriasis during preconception, pregnancy, postpartum, breastfeeding, and perinatal care.13 Our findings were mixed. Although the dermatologists surveyed were familiar with and highly knowledgeable about the aspects covered in the GPs consensus statement, implementation of some of the recommendations was low.
At the more general level, few dermatologists (or at least few of those surveyed) form part of multidisciplinary maternity care units or teams, even though 98% of the panel members who drew up the GPs recommendations agreed on the importance of collaborating with other specialists.13 Greater participation in multidisciplinary care has been observed in other disciplines, such as rheumatology.15 The survey also showed that very few dermatology departments have protocols tailored to specific care practices and available resources. Use of educational material other than verbal advice and information (pamphlets, videos, web-based tools, etc) is also uncommon. More work could probably be done in this area.
Almost a third of those surveyed do not routinely inquire about pregnancy plans, and less than 50% ask both men and women, showing that implementation of the GPs recommendation to regularly discuss family planning with all patients is far from optimal.13 Type of preconception advice offered also varies significantly. Very few dermatologists, for example, offer genetic counseling or discuss the potential impacts of psoriasis and psoriasis treatment on fertility. Although the GPs statement recommends routinely assessing pregnancy plans among all patients of reproductive age,13 the survey indicates that dermatologists tend to focus on specific groups of patients, such as women on systemic therapy and women with more severe forms of psoriasis. Another relevant finding to emerge from the survey was that it is often impossible to plan for pregnancy as many patients come to be seen when already pregnant. In view of the above, we consider that there is also room for improvement in preconception management of psoriasis. More widespread implementation of the GPs recommendations for managing psoriasis patients of reproductive age would improve numerous aspects, including, most notably, pregnancy planning.
Implementation of the GPs recommendations was greatest for psoriasis management during pregnancy, especially in relation to disease activity (being in remission or having as little disease activity as possible) and the use of topical, systemic, and biologic treatments. As recommended by the GPs, pregnant women are closely monitored using a tailored approach and appropriate actions in the event of a flare-up.
GPs recommendations relating to postpartum care and breastfeeding are also quite widely implemented according to the survey findings, although dermatologists tend to resume usual follow-up practices quite rapidly. More frequent monitoring during this period would be advisable given the risk of flare-ups.
Of note from our findings on barriers and facilitators for the implementation of the GPs recommendations13 is that nursing support and patient education material were perceived as being the easiest-to-implement interventions for improving the management of psoriasis before, during, and after pregnancy. Although it may currently be difficult to find more time or secure more support from nursing services, improving patient education material and tools is feasible.
Our study has a series of limitations, including some design issues. Because the survey was sent to GPs members, there is a risk of selection bias, as dermatologists who are members of this group may have more interest and experience in the management of psoriasis in relation to pregnancy, and accordingly, may be more familiar with and likely to implement the GPs recommendations. Nevertheless, the low degree of implementation observed for certain recommendations in this same group would suggest that implementation is even lower among dermatologists with less experience or interest in psoriasis. That said, the survey was conducted just a year after the recommendations were published online, and more time may be needed for their dissemination and implementation. Nonetheless, all the recommendations can, in theory, be quickly implemented in clinical practice as they are not affected by resource constraints or other limitations.
In summary, variable degrees of implementation of the GPs recommendations on managing psoriasis in relation to fertility, pregnancy, postpartum, breastfeeding, and perinatal care were observed, with high levels largely seen for treatment-related recommendations and lower levels seen for preconception-related recommendations. Other areas for improvement included greater participation in multidisciplinary maternity care units or teams and development of department-specific protocols and patient education materials. Continued efforts are needed to improve the implementation of the GPs recommendations, particularly in certain areas.
FundingThis project was initiated and funded by the AEDV with an unlimited grant from UCB.
Conflicts of InterestThe authors declare that they do not have any conflicts of interest in relation to this article.
The authors would like to thank the following dermatologists for participating in the survey: Mateu Puchades, Noemi Eiris Salvado, Jose Carlos Ruiz Carrascosa, Manel Sánchez Regaña, Alberto Conde Taboada, Rosario Fátima Lafuente Urrez, Manel Velasco, Silvia Pérez Barrio, Rosa Taberner, Ofelia Baniandrés Rodríguez, Conrad Pujol Marco, Alexandre Docampo Simón, Sabela Rodríguez Blanco, Javier Mataix Díaz, Eva Vilarrasa, Francisco Gómez, Laura Salgado-Boquete, Almudena Mateu Puchades, Anna Isabel Lázaro Simó, Mar Llamas, Susana Armesto, José Manuel Fernández Armenteros, Ana Morales Callaghan, Laura García Fernández, Álvaro González Cantero, Rubén del Río Gil, Anna López Ferrer, Josep Manel Casanova Ceuma, Patricio López, José Suárez Hernández, Montse Salleras Redonnet, Mercedes Hospital Gil, Diana Ruiz Genao, Beatriz Pérez Suárez, Elena Martínez, Asunción Vicente, Daniel Jesús Godoy Díaz, María Luisa Alonso Pacheco, Gregorio Carretero, Almudena Fernández Orland, Ricardo Ruiz-Villaverde, and Sergio Santos Alarcón.