Smooth muscle hamartoma (SMH) is a rare lesion, and is typically congenital, although some cases manifest in the first years of life. Several clinical forms are described: the first and most frequent is characterized by a smooth indurated plaque, which can be skin colored or hyperpigmented with hypertrichosis; while the second manifests as multiple papules with a follicular distribution, without hypertrichosis, occupying a circumscribed area. The less common clinical variant consists of more generalized lesions with prominent skin folds reminiscent of “Michelin baby”. These lesions are predominantly located in the lumbar area, and less commonly on the thighs, arms, face, or mammary region. The condition follows a benign course and the lesions, including hypertrichosis, usually attenuate with age.1
An 8-year-old girl and her 10-year-old sister each presented with an asymptomatic congenital lesion in the right pectoral area (Figs. 1 and 2). They were 2 daughters of nonconsanguineous parents and had no other siblings. The patients’ parents reported the absence of any similar lesions in the girls’ relatives, including themselves, their uncles, and their grandparents. Physical examination revealed a plaque composed of small hyperpigmented papules with a follicular distribution. The older sister's lesions had become increasingly flattened in the preceding years, coinciding with puberty.
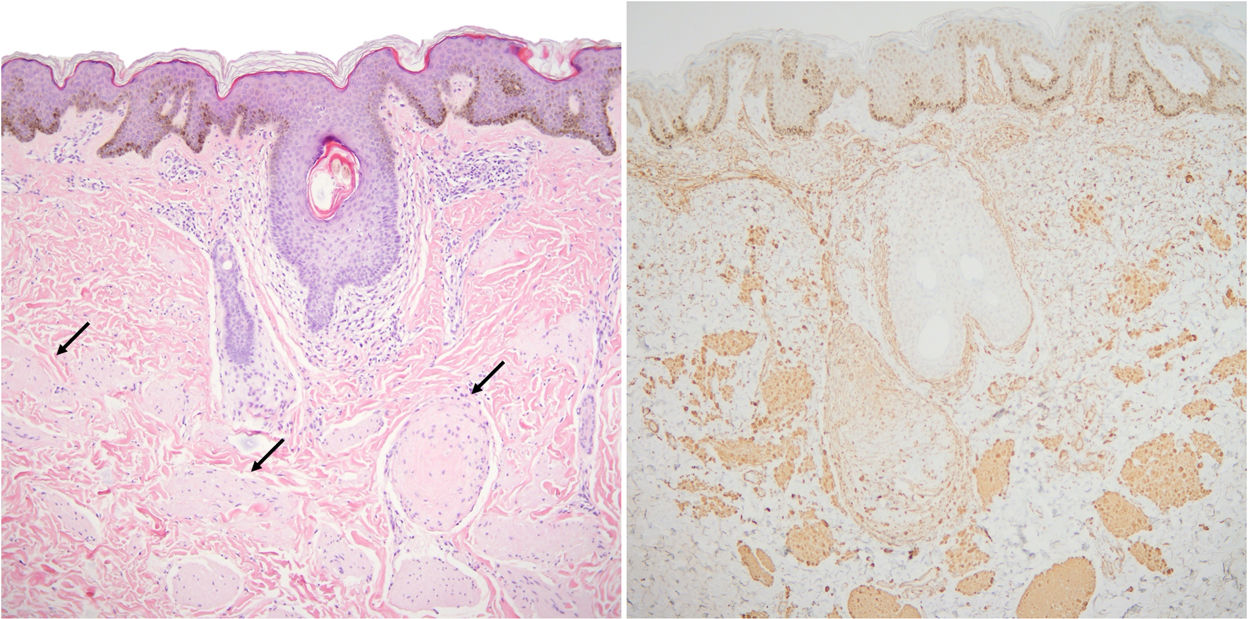
The younger sister underwent a biopsy at the level of the anterior axillary line. This showed minimal epidermal acanthosis, hyperpigmentation of the basal layer, and proliferation in the reticular dermis of multiple muscle fibers that showed no defined orientation and expressed smooth muscle actin (Fig. 3). Based on these findings, a diagnosis of SMH was established. The older sister's lesions were not biopsied as they appeared practically identical to those of her sister, caused no symptoms, and were located in a cosmetically sensitive location with a high probability of pathological scarring.
Histological image of the biopsy performed on the 8-year-old patient. A, Multiple smooth muscle fibers (black arrows) are distributed with no defined orientation in the dermis, beneath a slightly acanthotic epidermis (hematoxylin–eosin, original magnification ×10). B, Fibers stained for smooth muscle actin.
Due to morphological overlap, in some cases SMH and Becker nevus (BN) are considered to represent 2 poles on the same spectrum of developmental disorders.2 In our patients, the diagnosis of SMH was based on the papular appearance and the abundance of muscle fibers in the dermis. BN is caused by postzygotic mutations in the β-actin gene (ACTB) that are detected only in dermal smooth muscle fibers.3 These mutations are lethal when expressed in the germ line, and are therefore not heritable.4 Mutations in the same ACTB gene have recently been described in SMH.5
Two other cases of SMH have been described in siblings, in which, curiously, the location of the lesions also coincided, as in our patients.6,7 Several cases of BN have also been published in various members of the same family (familial BN).8–11 Although paradominance has been proposed to explain these cases, the discovery in BN of these mutations, which are dominant and lethal when they occur in the germ line, rules out this mechanism.4 Although coincidence cannot be ruled out, the manner in which the clinical presentation is replicated between parents and children and between siblings is indeed striking.
In conclusion, we describe the cases of 2 sisters with SMH with coinciding lesions. As also described for other familial cases of hamartoma, coincidence of the same lesion in the same site is unusual, and challenges current understanding of genetic mosaicism.
Conflicts of InterestThe authors declare that they have no conflicts of interest.