These are the case reports of 2 women, aged 32 and 45, with a past medical history of atopic dermatitis and no other significant medical history who presented with nearly identical clinical signs. Both reported the appearance of a pruritic lesion on their breast apparently unrelated to any specific trigger. They were not breastfeeding and denied any family history of breast cancer.
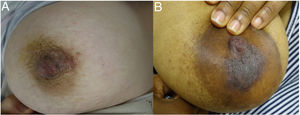
Physical examinationPatient #1. The lesion had appeared almost a month ago. The physical examination revealed the presence of an erythematous, scaly, verrucous-looking plaque on the right nipple, with minimal exudation and no signs of scratching (Fig. 1A).
Patient #2. Patient with phototype V, with a brownish, scaly plaque affecting the left breast areola-nipple complex, with poorly demarcated borders and no palpable induration (Fig. 1B).
Neither one of the 2 patients had underlying breast masses or axillary lymphadenopathy.
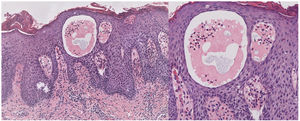
HistopathologyThe histopathological examination of a punch biopsy identified the presence of psoriasiform epidermal hyperplasia, along with pale cytoplasm keratinocytes and eosinophilic exocytosis (Fig. 2).
Supplementary testsBoth patients had normal previous ultrasounds and/or mammograms.
What is the diagnosis?DiagnosisEczematous nipple dermatitis with clear cell acanthoma dermoscopy pattern, or pseudoxanthoma of clear cells.
Evolution and treatmentSince these were eczemas with special histopathological features, they were treated with medium-potency topical corticosteroids and antibiotics, leading to complete resolution 1 month after starting treatment. The patients remain lesion-free to this date, using moisturizing creams for atopic skin as maintenance therapy. However, 1 of them continues to experience mild dermatitis flare-ups at other sites.
CommentClear cell acanthoma (CCA) was first described by Degos et al. in 1962 as a benign epidermal tumor. It often occurs on the lower limbs in middle-aged individuals and presents as a solitary reddish papule or nodule with vascular dots inside (referred to as “pearl-necklace pattern” in dermatoscopy). However, atypical, multiple, and even spontaneous regression sites and clinical forms have been reported. Along with its histopathological features, this has led to suggesting that CCA could be a reactive hyperplasia to chronic inflammation.1,2
The histopathology of CCA is very typical with well-demarcated regions of psoriasiform epidermal hyperplasia, along with pale cytoplasm keratinocytes and neutrophilic exocytosis. The periodic acid-Schiff (PAS) staining often confirms the presence of glycogen in the pale cells.3
CCA of the areola-nipple complex has been reported in the medical literature in less than 20 patients, mostly young Asian women, although it can also affect men as well.
Except for 1 case that was probably a true CCA, these lesions often present as pruritic eczematous and unilateral plaques, or else bilateral in up to 50% of the cases.4 The lesions appear on the mammary areola but can also compromise the nipple. Therefore, differential diagnosis must include Paget's disease, erosive adenomatosis of the nipple, or nipple and areola hyperkeratosis, among other causes of persistent nipple eczema. Unlike traditional CCA, the inflammatory infiltrate and exocytosis from eosinophils are both significant findings at histopathological level.
Given its association with atopic dermatitis in 25% to 43% of the cases, the presence of eosinophils at histopathological level, and healing with topical corticosteroids, it should be considered a non-neoplastic inflammatory disease and called eczematous nipple/areola dermatitis with a CCA pattern.5
We believe it is important to raise awareness of this condition to avoid aggressive therapies such as surgical procedures in these patients due to the location and future functional, aesthetic, and sexual implications.
Conflicts of interestNone declared.