A 40-year-old man, with no relevant past personal history, with a 5-month history of erythema, itching, and diffuse infiltration of the right mammary areola, without any triggering factor or associated systemic symptoms.
Physical examinationPhysical examination revealed the presence of an erythematous-violaceous, thickened, infiltrated right mammary areola, palpable on touch (fig. 1), with no locoregional lymphadenopathy or other lesions elsewhere on the skin integumentary system.
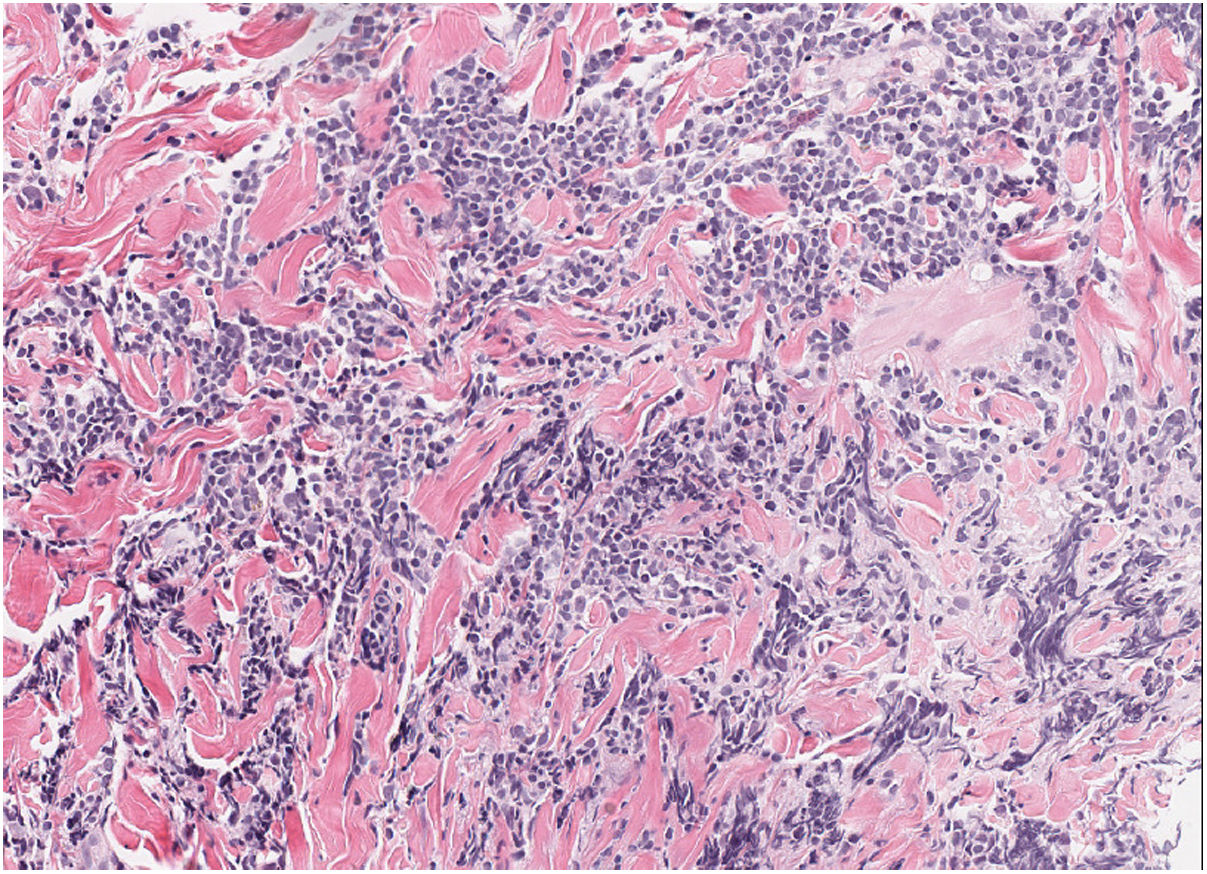
HistopathologySkin biopsy showed a dense dermal lymphoid infiltrate composed of intermediate-sized cells with occasional large cells, and a few accompanying eosinophils (fig. 2). Presence of non-confluent germinal centers in deep dermis. Immunophenotypic study: mixed infiltrate of T cells (CD3+, CD4+, CD7+) CD30− with occasional PD1+ cells, and B cells (CD20+, CD79a+) bcl2− with focal positivity for CD10 and CD21. No restriction of light chains of immunoglobulins by in situ hybridization was observed. Rearrangement of T-cell receptor genes and immunoglobulin heavy chains: polyclonal pattern.
Other additional testsComplete blood count, standard count, formula, and biochemistry showed no changes. Breast ultrasound revealed thickening of the cutaneous complex of the areola-nipple, with no identification of fibroglandular tissue or underlying focal lesions.
What is your diagnosis?.
DiagnosisReactive cutaneous lymphoid hyperplasia.
Course of the disease and treatmentUpon further questioning, the patient reported having traveled to Sweden 6 months prior to the consultation, admitting to having suffered several tick bites. Serologies for Borrelia burgdorferi were requested, showing negative IgM antibodies, weakly positive IgG antibodies, and positive PCR for B. burgdorferi (OspA gene) in the skin biopsy, leading to the diagnosis of lymphocytoma cutis due to Borrelia. A 2-week regimen of doxycycline 100 mg every 12 hours was initiated with complete resolution of the clinical picture.
CommentReactive cutaneous lymphoid hyperplasias (RCLH) or cutaneous pseudolymphomas constitute a heterogeneous group of benign hyperplastic lymphoproliferative reactions that clinically and/or histologically mimic a malignant lymphoproliferative process.1
Lymphocytoma cutis (LC) is considered the prototype of nodular cutaneous B-cell pseudolymphoma with follicular pattern. LC can be induced by various antigenic stimuli, including arthropod bites, drugs, and vaccines. In endemic regions, B. burgdorferi is the main causative agent, being rare in our environment. Borrelia-induced LC is a rare cutaneous sign of Lyme disease that occurs weeks or months after the bite of an Ixodes tick. It is usually observed in children and young adults with a slight predominance in women. There are several descriptions in the literature of cases similar to the one presented here.2-4
Clinically, it presents as a painless erythematous-violaceous nodule or plaque that mainly affects the earlobe, the areola-nipple complex, or the scrotum.5 It is usually accompanied by regional lymphadenopathy.
Histopathological examination shows a nodular lymphoid infiltrate, without cellular atypia, affecting the entire dermis, with formation of large and confluent germinal centers with a reduced or absent mantle zone. The infiltrate consists of plasma cells, eosinophils, reactive T lymphocytes, and macrophages with apoptotic cells phagocytized inside (tingible bodies). Immunophenotyping demonstrates lymphoid proliferation with predominance of B-cell germinal center cells, positive for CD20, CD10, and Bcl-6 and negative for Bcl-2, with polytypic light chains expression of immunoglobulins.6
The diagnosis of Borrelia-induced LC is clinical and requires a high level of suspicion.7 The presence of diffuse infiltration of the mammary areola, with histopathological findings of nodular dermal lymphoid infiltration with germinal center formation, should raise suspicion of the diagnosis of a B-cell RCLH with nodular pattern and, within the appropriate epidemiological context, due to B. burgdorferi. Diagnosis is confirmed by histopathological examination, serologies, and/or detection of B. burgdorferi DNA in tissue by PCR.
The clinical differential diagnosis is established with primary or secondary cutaneous lymphomas, sarcoidosis, nodular gynecomastia, urticarial follicular mucinosis, lupus mastitis, and other etiologies of RCLH.
Treatment includes the administration of doxycycline 100 mg twice a day, or amoxicillin 500 mg every 8 hours for 2-3 weeks.8
FundingNone declared.
Conflicts of interestNone declared.