No recent data on health care resources and medical and surgical activity in Spanish dermatology departments are available in the literature. The aim of this study was to compile this information for 2019.
Material and methodsCross-sectional study based on an online survey sent to the heads of dermatology departments at public hospitals in Spain.
ResultsOf the 162 department heads contacted, 59 answered the survey (participation rate, 36.4%). General findings included a shortage of staff, especially dermatologists, in hospitals of low and medium complexity. The main reason given for the shortage of dermatologists was a lack of interested applicants. Large hospital complexes had more infrastructure and equipment. Over 50% of the departments surveyed used a combination of in-person and virtual visits. Psoriasis units were the most common specialized care units. Approximately 75% of the hospitals had operating rooms with an anesthetist. More complex procedures such as sentinel lymph node biopsy and Mohs micrographic surgery were performed more often in large hospital complexes. Hospitalization and the presence of dermatology residents working call shifts were also more common in these hospitals. Teaching and research activity differed according to hospital complexity.
ConclusionsWe have mapped health care resource availability and medical and surgical activity in Spanish dermatology departments prior to the COVID-19 pandemic. Our findings could be useful for improving clinical management and defining future actions and areas for improvement.
No existen datos actualizados sobre los recursos asistenciales ni la actividad médico-quirúrgica de los servicios de dermatología españoles. El objetivo de esta investigación es conocer la situación y actividad de dichos servicios durante el año 2019.
Material y métodosEstudio transversal mediante cuestionario online distribuido a los jefes de servicio de dermatología de hospitales públicos españoles.
ResultadosDe los 162 jefes de servicio encuestados, se obtuvo una participación del 36,4% (59/162). Se observó un déficit de personal generalizado, especialmente de dermatólogos en hospitales de complejidad media-baja. La principal causa del déficit de dermatólogos fue la ausencia de profesionales interesados. Las infraestructuras y equipamiento disponibles fueron superiores en los grandes complejos hospitalarios. La atención mixta presencial-telemática estuvo presente en más de la mitad de los centros. En el ámbito de las consultas monográficas, la de psoriasis fue la más implementada. Aproximadamente el 75% de los centros contaron con quirófanos con anestesista. Procedimientos quirúrgicos de mayor complejidad como la biopsia selectiva de ganglio centinela o la cirugía de Mohs se realizaban con mayor frecuencia en los grandes complejos hospitalarios. La hospitalización de pacientes y la presencia de dermatólogos residentes de guardia fue igualmente más habitual en estos hospitales. La actividad docente e investigadora también se relacionó con la complejidad del hospital.
ConclusionesNuestros resultados describen la situación de los servicios de dermatología españoles justo antes de la pandemia por COVID-19, y pueden ser útiles para la gestión clínica y para definir líneas de trabajo y áreas de mejora.
Dermatology is a medical–surgical specialty where most of the caseload involves care for patients in the outpatient clinic. The White Paper of the Spanish Academy of Dermatology and Venereology (Academia Española de Dermatología y Venereología [AEDV]) provided an initial picture of sociodemographic data, resources, structure, clinical activity, training, and teaching and research in dermatology in Spain in 2008.1 Subsequent investigations covered activity in outpatient clinics, admissions to hospital, and research activity in Spanish dermatology departments.2–6 However, we do not have updated information on staffing, infrastructures, equipment, or other aspects of the activity of dermatology departments, such as surgery, appointment scheduling, and teaching activity. This information could prove to be very important for clinical management when identifying needs and future actions. The objective of the present study was to investigate current care resources and medical–surgical activity in the dermatology departments of public hospitals in Spain during the year 2019.
Material and methodsDesignWe designed a cross-sectional study using an online survey sent by email to the heads of dermatology departments in Spanish public hospitals. The list of heads of department and their e-mail addresses were obtained from the registry of the AEDV. We requested the cooperation of the regional chairs in order to obtain updated information on heads of department. The questionnaire was designed in October 2019. Distribution was delayed until May 2020 owing to the COVID-19 pandemic, with reminders sent every 5 days (up to 4 in total). In September 2020, the survey was resent to those heads of department who did not respond. The data requested were for 2019. The survey was designed, and data were collected and managed using the research electronic data capture platform (REDCap) via the AEDV Research Unit.7,8
Variables of interestWe recorded general information on the departments (complexity of the hospital according to the relevant cluster/group (Table 1), age of the department, quality accreditation, personnel, vacancies/leave not covered and the reasons, staff shortages), infrastructure and equipment (availability of physical space and various devices), medical–surgical activity (activity in the clinic and in operating rooms), teaching and research activity (presence of residents, monthly clinical sessions, presence of university staff, articles published, research projects, possible areas for improvement in the department's research activity), and other activities (admissions to hospital, interdepartmental consultation concerning patients admitted to other departments, participation in multidisciplinary committees, channels for communication with primary care, citizen engagement activity, on-call shifts).
Classification of hospitals into clusters according to complexity.
| Group/cluster 1: Small regional hospitals, <150 beds on average. Scarcely any high technology, few physicians, and low complexity |
| Group/cluster 2: Basic general hospitals, mean size <200 beds, with minimal technology, some teaching capacity, and somewhat higher complexity |
| Group/cluster 3: Area hospitals, with around 500 beds on average. More than 50 residents in training and an average of 269 doctors. Medium complexity (1.5 complex departments and case mix of 1.01) |
| Group/cluster 4: Large hospital complexes, although more heterogeneous in terms of equipment, size, and activity. Notable teaching activity (more than 160 residents in training) and high complexity (mean of 4 complex services and case mix >1.20) |
| Group/cluster 5: Hospitals with a large structure and considerable activity. Complete range of services. More than 680 doctors and around 300 residents in training. Includes large hospital complexes |
The normality of the distribution was verified using the Shapiro–Wilk test and histograms. Descriptive statistics were used to explore the characteristics of the sample. Continuous variables were expressed as mean (SD) in the case of a normal distribution and as the median (interquartile range [IQR]) in the case of a nonnormal distribution. Qualitative variables were expressed as absolute and relative frequencies. The t test was used to analyze differences between the groups in the case of parametric quantitative variables and the Mann–Whitney test in the case of nonparametric qualitative quantitative variables. The χ2 (or Fisher exact test) was used in the case of qualitative variables. Statistical significance was set at P<.05 (all tests, 2-tailed). The statistical analyses were carried out using STATA (Version 16.0; StataCorp).
EthicsGiven the characteristics of our research and the fact that the units of study were dermatology departments and not humans or animals, no ethics committee approval was required.
ResultsA total of 162 department heads were invited to participate in the study. Of these, 59 (36.4%) responded to the survey. Given the limited number of departments from low-complexity hospitals (3 from cluster 1 and 6 from cluster 2), these centers were grouped together with medium-complexity hospitals (cluster 3).
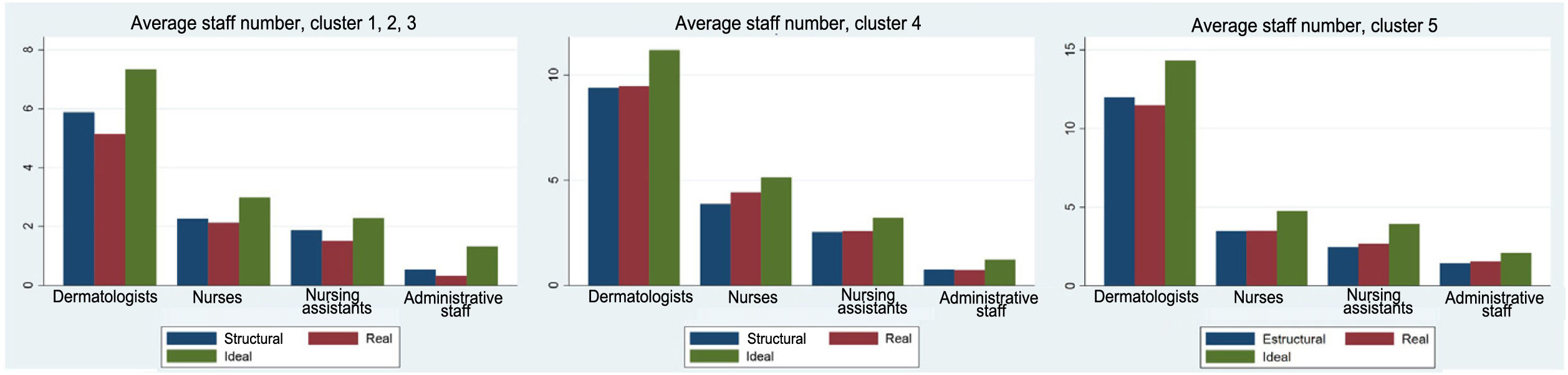
General informationLow and medium complexity hospitals had 5 dermatologists, high-complexity hospitals had 9.5, and large hospital complexes had 11.4. The greatest staff shortage, both in structural and in ideal terms, was observed in hospitals of low and medium complexity, especially with respect to dermatologists and administrative staff. High-complexity hospitals and large hospital complexes were generally not characterized by staff shortages in structural terms; however, there were differences with respect to what department heads considered the ideal number of staff, especially in the case of dermatologists (Fig. 1).
Departments in hospitals of low and medium complexity and high-complexity hospitals were characterized by an increasing trend in terms of vacancies/leave not covered, whereas in the large hospital complexes, these variables remained stable. The main reason why vacancies were not covered was the lack of interested and/or available applicants.
The mean age of dermatologists was 44.7 years. Most of the departments created in the last 15 years were in hospitals of low and medium complexity, whereas the departments in large hospital complexes were created more than 15 years ago. A quality accreditation had been achieved in 5 of 18 departments in large complexes (27.8%) and 4 of 25 departments in institutions of low and medium complexity, although none of the high-complexity hospitals had such an accreditation. Most of the high-complexity hospitals and large complexes had their own dermatology department, whereas in almost one-third of hospitals of low and medium complexity, dermatology was part of another department (Table 2).
Personnel and characteristics of dermatology departments in Spanish hospitals.a
| Hospitals of low and medium complexity | High-complexity hospitals | Large hospital complexes | P value | |
|---|---|---|---|---|
| Vacancies/leave not covered | ||||
| 2017 | ||||
| None | 18/24 (75%) | 10/15 (66.7%) | 10/17 (58.8%) | .54 |
| One | 4/24 (16.7%) | 2/15 (13.3%) | 2/17 (11.8%) | |
| Two or more | 2/24 (8.3%) | 3/15 (20%) | 5/17 (29.4%) | .28 |
| 2018 | ||||
| None | 18/24 (75%) | 8/15 (53.3%) | 9/17 (52.9%) | .22 |
| One | 4/24 (16.7%) | 3/15 (20%) | 2/17 (11.8%) | |
| Two or more | 2/24 (8.3%) | 4/15 (26.7%) | 6/17 (35.3%) | |
| 2019 | ||||
| None | 14/25 (56%) | 8/16 (50%) | 10/17 (58.8%) | |
| One | 8/25 (32%) | 4/16 (25%) | 1/17 (5.9%) | |
| Two or more | 3/25 (12%) | 4/16 (25%) | 6/17 (35.3%) | |
| Reasons for vacancies not covered | ||||
| Administrative/management decision | 1/12 (8.3%) | 1/9 (11.1%) | 2/8 (25%) | .38 |
| No interested applicants | 11/12 (91.7%) | 8/9 (88.9%) | 5/8 (62.5%) | |
| Other | – | – | 1/8 (12.5%) | |
| Mean age of dermatologists in the department, y | 43.2 (5.5) | 45.7 (4.5) | 45 (3.7) | .27 |
| Age of the department | ||||
| <5 y | 1/25 (4%) | 0/16 (0%) | 0/18 (0%) | .42 |
| 5–15 y | 3/25 (12%) | 2/16 (12.5%) | 0/18 (0%) | |
| >15 y | 21/25 (84%) | 14/16 (87.5%) | 18/18 (100%) | |
| Quality accreditation | ||||
| Yes | 4/25 (16%) | 0/16 (0%) | 5/18 (27.8%) | .21 |
| ISO | 3/4 (75%) | – | 1/5 (20%) | |
| ACSA | 1/4 (25%) | – | 4/5 (80%) | |
| No | 21/25 (84%) | 16/16 (100%) | 13/18 (72.2%) | |
| Dermatology is: | ||||
| A department | 17/25 (68%) | 16/16 (100%) | 17/18 (94.4%) | <.01 |
| Part of another department | 8/25 (32%) | 0/16 (0%) | 1/18 (5.6%) | |
Abbreviations: ACSA, Agencia de Calidad Sanitaria de Andalucía (Health Care Quality Agency of Andalusia); ISO, International Organization for Standardization.
The median number of consulting rooms (physical spaces) was 4 in hospitals of low and medium complexity, 6.5 in high-complexity hospitals, and 7 in large hospital complexes, whereas the equivalent number in outpatient centers was 1, 4, and 3.5, respectively. Treatment rooms were more readily available in high-complexity hospitals and large complexes. The median number of operating rooms was 1 in all types of hospital. Access to the medical and surgical day hospital, ward, and lecture room was easier in high-complexity institutions and large complexes; the differences were significant in the case of the lecture rooms. The mean number of available beds and the presence of a library were greater in larger complexes (Table 3).
Infrastructure.a
| Hospitals of low and medium complexity | High-complexity hospitals | Large hospital complexes | P Value | |
|---|---|---|---|---|
| No. of hospital clinics/outpatient departments | 4 (3–6) | 6.5 (2.5–8.5) | 7 (4–9) | .11 |
| No. of outpatient clinics | 1 (0–3) | 4 (2–5) | 3.5 (1–5) | <.01 |
| No. of treatment rooms | 1 (1–2) | 2 (1–2.5) | 1.5 (1–2) | .26 |
| No. of operating rooms | 1 (1–1) | 1 (1–1.5) | 1 (1–2) | .37 |
| Access to medical day hospital | ||||
| Yes | 21/25 (84%) | 15/16 (93.8%) | 16/18 (88.9%) | .64 |
| No | 4/25 (16%) | 1/16 (6.2%) | 2/18 (11.1%) | |
| Access to surgical day hospital | ||||
| Yes | 17/25 (68%) | 14/16 (87.5%) | 16/18 (88.9%) | .16 |
| No | 8/25 (32%) | 2/16 (12.5%) | 2/18 (11.1%) | |
| Wards | ||||
| Yes | 7/25 (28%) | 10/16 (62.5%) | 10/18 (55.6%) | .06 |
| No | 18/25 (72%) | 6/16 (37.5%) | 8/18 (44.4%) | |
| Mean no. of beds | 2 (1–4) | 2 (1–4) | 4 (2–4) | .3 |
| Lecture rooms | ||||
| Yes | 13/25 (52%) | 16/16 (100%) | 17/18 (94.4%) | <.001 |
| No | 12/25 (48%) | 0/16 (0%) | 1/18 (5.6%) | |
| Library | ||||
| Yes | 9/25 (36%) | 7/16 (43.8%) | 12/18 (66.7%) | .13 |
| No | 16/25 (64%) | 9/16 (56.2%) | 6/18 (33.3%) | |
Most departments in all the types of hospitals studied (>80%) were equipped with patch testing, electrosurgery devices, Wood lamps, and photodynamic therapy devices. All departments provided cryotherapy, with differences in the number of devices, which was greater in high-complexity hospitals and large hospital complexes. Similarly, all departments provided phototherapy, with statistically significant differences for the hospitals of low and medium complexity; narrow-band UV-B and psoralen UV-A devices were the most common. Statistically significant differences were also recorded for availability of a laser, which was more common in high-complexity hospitals and large complexes, with CO2 being the most frequent, and in the availability of optical microscopes, which were more common in large complexes. More novel techniques, such as confocal microscopy and electrochemotherapy, were limited mainly to departments in large complexes. The only devices that were less available in these centers were iontophoresis devices for self-management (Table 4).
Equipment.a
| Hospitals of low and medium complexity | High-complexity hospitals | Large hospital complexes | P value | |
|---|---|---|---|---|
| Patch tests | ||||
| Yes | 21/25 (84%) | 13/16 (81.3%) | 16/17 (94.1%) | .52 |
| No | 4/25 (16%) | 3/16 (18.2%) | 1/17 (5.9%) | |
| Electrosurgery | ||||
| Yes | 21/25 (84%) | 15/16 (93.8%) | 18/18 (100%) | .17 |
| No | 4/25 (16%) | 1/16 (6.2%) | 0/18 (0%) | |
| No. of devices | 2 (1–5) | 3 (2–4) | 2.5 (2–4) | .74 |
| Wood lamp | ||||
| Yes | 23/25 (92%) | 15/16 (93.8%) | 18/18 (100%) | .48 |
| No | 2/25 (8%) | 1/16 (6.2%) | 0/18 (0%) | |
| No. of devices | 2 (1–2) | 3 (1–5) | 1 (1–3) | .15 |
| Photodynamic therapy | ||||
| Yes | 20/24 (83.3%) | 14/16 (87.5%) | 18/18 (100%) | .2 |
| No | 4/24 (16.7%) | 2/16 (12.5%) | 0/18 (0%) | |
| No. of devices | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.8 |
| Cryosurgery | ||||
| Yes | 25/25 (100%) | 16/16 (100%) | 18/18 (100%) | – |
| No | 0/25 (0%) | 0/16 (0%) | 0/18 (0%) | |
| No. of devices | 4 (3–6) | 5 (4.5–8) | 5 (4–7) | <.05 |
| Phototherapy | ||||
| Yes | 19/25 (76%) | 16/16 (100%) | 18/18 (100%) | <.05 |
| No | 6/25 (24%) | 0/16 (0%) | 0/18 (0%) | |
| No. of devices | 2 (1–2) | 2 (1.5–3) | 2 (2–3) | .27 |
| Type | ||||
| NBUVB | 18/19 (94.7%) | 16/16 (100%) | 18/18 (100%) | – |
| NBUVB hands and feet | 10/16 (62.5%) | 9/14 (64.3%) | 12/16 (75%) | |
| UV-A-1 | 4/12 (33.3%) | 8/12 (66.7%) | 6/12 (50%) | |
| PUVA | 17/18 (94.4%) | 12/14 (85.7%) | 14/16 (87.5%) | |
| Other | 2/7 (28.6%) | 5/8 (62.5%) | 2/7 (28.6%) | |
| Ultrasound | ||||
| Yes | 15/25 (60%) | 12/16 (75%) | 18/18 (100%) | <.01 |
| No | 10/25 (40%) | 4/16 (25%) | 0/18 (0%) | |
| No. of devices | 1 (1–2) | 1 (1–1) | 1 (1–1) | .88 |
| Digital dermoscopy | ||||
| Yes | 18/25 (72%) | 15/16 (93.8%) | 15/18 (83.3%) | .21 |
| No | 7/25 (28%) | 1/16 (6.3%) | 3/18 (16.7%) | |
| No. of devices | 1 (1–1) | 1 (1–1) | 1 (1–2) | .77 |
| Laser | ||||
| Yes | 5/25 (20%) | 9/16 (56.3%) | 10/18 (55.6%) | <.05 |
| No | 20/25 (80%) | 7/16 (43.2%) | 8/18 (44.4%) | |
| No. of devices | 1 (1–2) | 1 (1–2) | 1.5 (1–2.5) | .84 |
| Type | ||||
| CO2 | 5/5 (100%) | 9/9 (100%) | 7/9 (77.8%) | |
| Pulsed dye | 0/4 (0%) | 3/7 (42.9%) | 6/10 (60%) | |
| Neodymium | 2/5 (40%) | 1/7 (14.3%) | 4/8 (50%) | |
| Other | 2/5 (40%) | 0/5 (0%) | 1/7 (14.3%) | |
| Confocal microscopy | ||||
| Yes | 1/25 (4%) | 1/16 (6.2%) | 3/18 (16.7%) | .32 |
| No | 24/25 (96%) | 15/16 (93.8%) | 15/18 (83.3%) | |
| No. of devices | 1 (1–1) | 1 (1–1) | 1 (1–1) | – |
| Optical microscope | ||||
| Yes | 12/25 (48%) | 12/16 (75%) | 17/18 (94.4%) | <.01 |
| No | 13/25 (52%) | 4/16 (25%) | 1/18 (5.6%) | |
| No. of devices | 1 (1–1) | 1 (1–2.5) | 2 (1–2) | .13 |
| Electrochemotherapy | ||||
| Si | 0/25 (0%) | 0/16 (0%) | 4/17 (23.5%) | <.01 |
| No | 25/25 (100%) | 16/16 (100%) | 13/17 (76.5%) | |
| No. of devices | – | – | 1 (1–1) | – |
| Iontophoresis | ||||
| Yes | 9/25 (36%) | 6/16 (37.5%) | 4/18 (22.2%) | .55 |
| No | 16/25 (64%) | 10/16 (62.5%) | 14/18 (77.8%) | |
| No. of devices | 1 (1–2) | 1 (1–1) | 2 (1–3) | .47 |
Abbreviations: CO2, carbon dioxide; PUVA, psoralen–UV-A; NBUVB, narrowband UV-B.
The median number of hospital and outpatient appointment schedules was, respectively, 41.5 and 20 in hospitals of low and medium complexity, 30 and 32 in high-complexity centers, and 26.5 and 23 in large complexes. The total number of patients treated during 2019 was greater in the departments of the high-complexity centers and large complexes. The visit model was mixed (in-person+virtual consultation) in around 60% of all the departments, with a greater number of remote consultations in the large complexes than in the other types of center. Patients spent a median of 80 days on the waiting list in hospitals of low and medium complexity and 42.5 days in the others. The number of checkups during 2019 and the number of monthly specialist appointment schedules was greater in high-complexity centers and large complexes. The most common functional unit was the psoriasis unit, followed by dermatology–oncology, pediatric dermatology, hidradenitis suppurativa, and digital dermoscopy. Most of the participants, especially in the high-complexity centers and large complexes (100%), would like the specialist units to have a quality accreditation from the AEDV (Table 5).
Activity in clinics.a
| Hospitals of low and medium complexity | High-complexity hospitals | Large hospital complexes | P value | |
|---|---|---|---|---|
| No. of appointment schedules per month (excluding specialist appointments) in hospital/outpatient clinic | 41.5 (27–68) | 30 (13–76) | 26.5 (17.5–75) | .96 |
| No. of appointment schedules per month in outpatient clinic | 20 (15–45) | 32 (7–85) | 23 (7.5–40) | .62 |
| Initial visit format | ||||
| Exclusively in-person | 9/25 (36%) | 6/15 (40%) | 5/14 (35.8%) | .56 |
| Exclusively virtual | 0/25 (0%) | 0/15 (0%) | 1/14 (7.1%) | |
| Mixed | 16/25 (64%) | 9/15 (60%) | 8/14 (57.1%) | |
| Total no. of initial visits in 2019 | 9316.5 (5000–13,000) | 17,308 (11,272–20,000) | 15,876 (15,000–19,000) | <.01 |
| Median time on waiting list | 80 (58–90) | 42.5 (30–70) | 42.5 (24–60) | <.05 |
| No. of monthly virtual consultations in primary care | 80 (12–200) | 140 (30–200) | 478 (100–792.5) | .08 |
| % of initial primary care visits managed virtually | 20 (5–40) | 7.5 (1.6–10) | 11 (10–40) | .3 |
| Median time to response for virtual visits (days) | 2 (1–7) | 2 (1–2.5) | 2 (1–3) | .91 |
| Total no. of virtual visits in 2019 | 150 (10–1122) | 1200 (1000–1750) | 9415 (500–12,000) | <.05 |
| Total no. of checkups in 2019 | 8758.5 (6250–15,000) | 15,653 (11,905–19,000) | 17,000 (13,547–25,000) | <.01 |
| No. of monthly specialist appointment schedules | 4 (0–25) | 20 (4–24) | 13 (7–25) | .06 |
| Are the following specialist units available at your hospital? | ||||
| Dermatology-oncology (melanoma and SCC) | 11/23 (47.8%) | 7/13 (53.8%) | 11/12 (91.7%) | |
| Cutaneous lymphoma | 2/24 (8.3%) | 6/14 (42.9%) | 7/11 (63.6%) | |
| Pediatric dermatology | 10/23 (43.5%) | 10/14 (71.4%) | 10/12 (83.3%) | |
| Autoimmune, connective tissue, and systemic diseases | 3/23 (13%) | 4/14 (28.6%) | 6/11 (54.5%) | |
| Bullous skin diseases | 0/23 (0%) | 1/13 (7.7%) | 5/10 (50%) | |
| Psoriasis | 11/24 (45.8%) | 10/14 (71.4%) | 10/10 (100%) | |
| Hidradenitis suppurativa | 5/24 (20.8%) | 6/14 (42.9%) | 9/10 (90%) | |
| Photobiology | 5/24 (20.8%) | 6/13 (46.2%) | 5/10 (50%) | |
| Cutaneous immunoallergy | 4/24 (16.7%) | 9/13 (69.2%) | 8/11 (72.7%) | |
| Trichology | 0/24 (0%) | 2/13 (15.4%) | 4/11 (36.4%) | |
| Vascular disorders | 0/23 (0%) | 0/12 (0%) | 4/10 (40%) | |
| STI | 4/24 (16.7%) | 8/14 (57.1%) | 4/11 (36.4%) | |
| Laser | 1/23 (4.3%) | 3/13 (23.1%) | 1/10 (10%) | |
| Ultrasound | 5/23 (21.7%) | 3/13 (23.1%) | 2/10 (20%) | |
| Digital dermoscopy/pigmented lesions | 10/24 (41.7%) | 11/14 (78.6%) | 9/11 (81.8%) | |
| Would you like specialist units to receive quality accreditation by the AEDV? | ||||
| Yes | 17/22 (77.3%) | 13/13 (100%) | 11/11 (100%) | .07 |
| No | 5/22 (22.7%) | 0/13 (0%) | 0/11 (0%) | |
Abbreviations: AEDV, Academia Española de Dermatología y Venereología (Spanish Academy of Dermatology and Venereology); SCC, squamous cell carcinoma; STI, sexually transmitted infection.
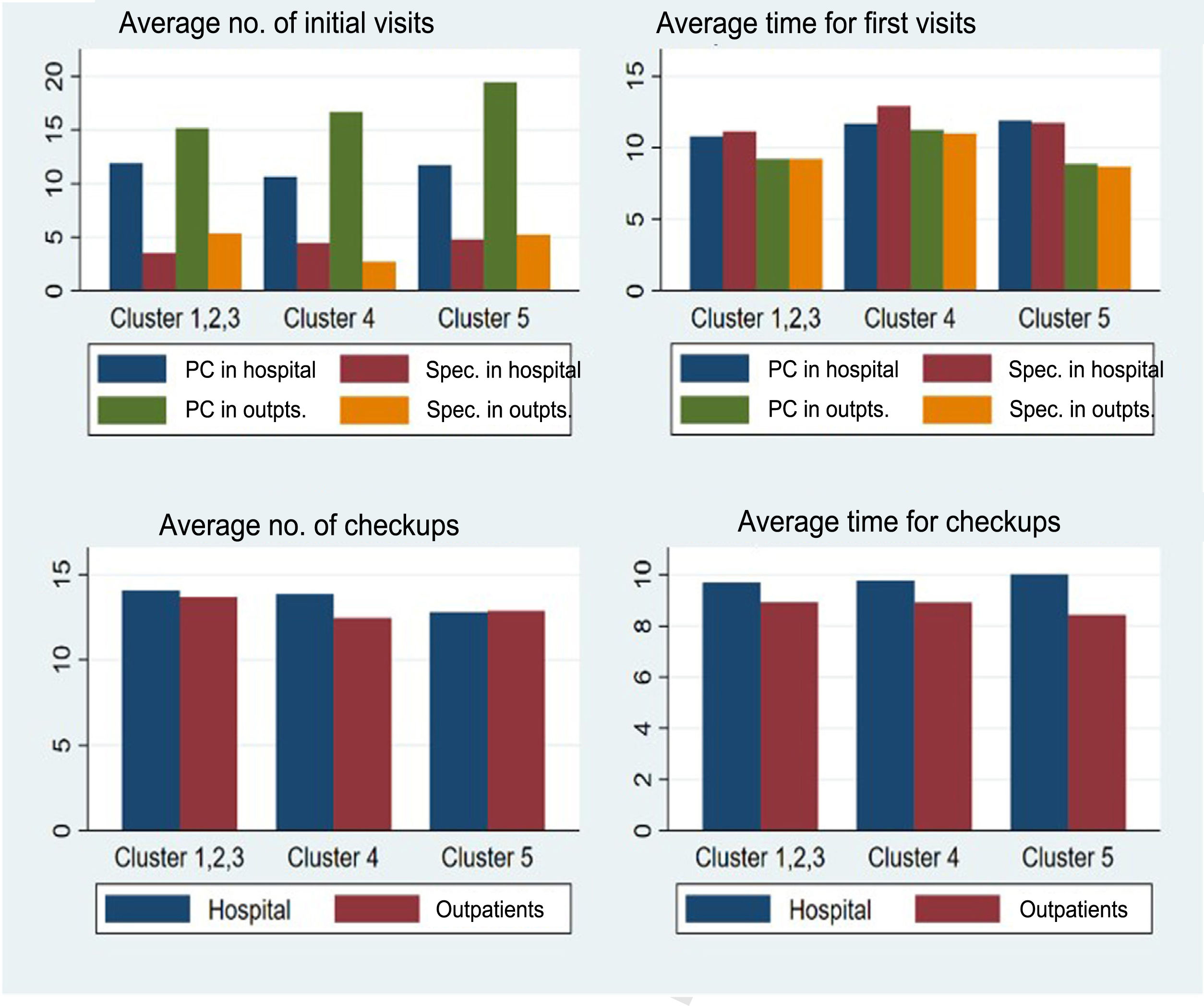
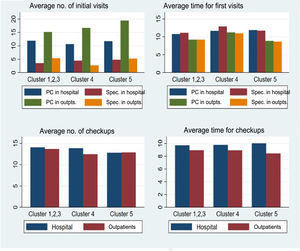
As for scheduling of appointments, the large number of patients referred from primary care to the outpatient clinics of large complexes is noteworthy—almost 20 patients per schedule and day compared with 15 from the schedules of outpatient clinics at hospitals of low and medium complexity. The number of initial visits from specialist care was 3–5 per schedule and day in all departments, both in hospitals and in outpatient clinics. The time dedicated to initial visits was greater in all departments in hospitals (11–13min) than in outpatient clinics (9–10min). The number of checkups was 13–14 in all the services, both in hospitals and in outpatient clinics, whereas the time for each checkup was around 10min for all departments in hospitals and around 9min in outpatient clinics (Fig. 2). These data contrast with the ideal schedule department heads would wish for, where both the mean number of initial visits per schedule (11.6, 11.5, and 10.2 in hospitals of low and medium complexity, high-complexity hospitals, and large complexes, respectively) and checkups (10.6, 10.7, and 9, respectively) would be lower than observed, and both mean time in minutes per patient at the initial visit (15.3, 14.3, and 16.2, respectively) and at checkups (13.7, 12.3, and 14, respectively) would be higher.
Appointment schedules. Number of patients and time assigned to each patient at the initial visits (referred from both primary care and a specialist center) and for checkups from hospital centers and outpatient clinics of the hospitals in the different clusters. PC indicates primary care; Spec., specialist care; outpts., outpatients.
Almost three-quarters (74%) of the departments had operating rooms with an anesthetist, with more interventions in high-complexity hospitals and large complexes. The median number of operating rooms was higher in high-complexity hospitals, whereas the median number of patients included in each operating room with an anesthetist was lower in large complexes. As for operating rooms without an anesthetist, the total number of patients treated in 2019 and the mean number of operating rooms per month was significantly higher in high-complexity hospitals and large complexes. Techniques such as selective sentinel node biopsy and Mohs micrographic surgery were more frequent in large complexes. The median time on the surgical waiting list was 40 days in hospitals of low and medium complexity, 30 days in high-complexity centers, and 75 days in large complexes. The number of patients referred to other services for surgery was higher in high-complexity hospitals (Table 6).
Surgical activity.a
| Hospitals of low and medium complexity | High-complexity hospitals | Large hospital complexes | P value | |
|---|---|---|---|---|
| Availability of operating rooms with anesthetist | ||||
| Yes | 18/24 (75%) | 10/14 (71.4%) | 9/12 (75%) | .97 |
| No | 6/24 (25%) | 4/14 (28.6%) | 3/12 (25%) | |
| No. of procedures with anesthetist in 2019 | 40 (17–185) | 149 (31–300) | 150 (40–240) | .31 |
| Median no. of operating rooms (monthly) with an anesthetist | 1 (1–3) | 8 (2–10) | 4 (2–5.5) | <.05 |
| Median no. of patients included in an operating room with an anesthetist | 4 (4–5) | 4 (3–4) | 3 (3–5) | .82 |
| No. of procedures without an anesthetist in 2019 | 1277.5 (202.7) | 1.884.5 (271.1) | 3.801 (2041.5) | <.001 |
| Mean no. of operating rooms without an anesthetist (monthly) | 14.4 (2.9) | 30.2 (7.9) | 29.7 (9.8) | <.01 |
| Median no. of patients included in an operating room without an anesthetist | 11 (0.5) | 10.3 (0.9) | 11 (1.3) | .27 |
| Is SSNB performed? | ||||
| Yes | 8/23 (34.8%) | 2/14 (14.3%) | 4/11 (36.4%) | .35 |
| No | 15/23 (65.2%) | 12/14 (85.7%) | 7/11 (63.6%) | |
| Median no. of SSNBs per month | 1 (1–1) | 4.5 (1–8) | 3 (3–4.5) | .13 |
| Total no. of SSNBs in 2019 | 10 (5–11) | 12 (12–12) | 41.5 (31–52) | .13 |
| Is Mohs micrographic surgery performed? | ||||
| Yes | 9/23 (39.1%) | 7/14 (50%) | 7/11 (63.6%) | .4 |
| No | 14/23 (60.9%) | 7/14 (50%) | 4/11 (36.4%) | |
| Median no. of Mohs procedures per month | 4 (1.5–11) | 4 (1–6) | 5 (3–8) | .59 |
| Total no. of Mohs procedures in 2019 | 20 (7–101) | 42 (10–55) | 44 (26.5–112.5) | .65 |
| Median time on surgical waiting list, d | 40 (30–60) | 30 (30–60) | 75 (30–90) | .34 |
| Median no. of patients referred monthly to other departments for surgery | 2 (1–5) | 5 (3–10) | 2 (1–5) | .24 |
Abbreviation: SSNB, selective sentinel node biopsy.
The presence and number of residents in training and the number of monthly clinical sessions were greater in large complexes, with statistically significant differences. All high-complexity hospitals and large complexes and most hospitals of low and medium complexity held joint sessions with other departments, especially histopathology. The number of lecturers associated with universities and research projects publicly funded through competitive calls was also significantly higher in large complexes. As for ways of improving departmental research, the main area identified by all the participants was the need for time dedicated specifically to research. Also highlighted were participation in multicenter studies, public funding, and cooperation with the AEDV and its Research Unit (Table 7).
Teaching and research activity.a
| Hospitals of low and medium complexity | High-complexity hospitals | Large hospital complexes | P value | |
|---|---|---|---|---|
| Residents via specialist health care training(RIT) | ||||
| Yes | 10/25 (40%) | 11/16 (68.8%) | 17/18 (94.4%) | <.01 |
| No | 15/25 (60%) | 5/16 (31.3%) | 1/18 (5.6%) | |
| No. of residents | 3.5 (1–4) | 4 (4–7) | 4 (4–8) | <.05 |
| No. of monthly sessions | 5 (1.5–9) | 8 (6–12) | 14 (10–16) | <.01 |
| Joint sessions with other departments | ||||
| Yes | 21/25 (84%) | 16/16 (100%) | 18/18 (100%) | .054 |
| No | 4/25 (16%) | 0/16 (0%) | 0/18 (0%) | |
| Departments | ||||
| Rheumatology | 9/14 (64.3%) | 8/15 (53.3%) | 8/13 (61.5%) | |
| Internal medicine | 7/15 (46.7%) | 4/11 (36.4%) | 6/12 (50%) | |
| Histopathology | 18/20 (90%) | 16/16 (100%) | 17/18 (94.4%) | |
| Hematology | 0/13 (0%) | 2/13 (15.4%) | 5/12 (41.7%) | |
| Pediatrics | 3/14 (21.4%) | 1/10 (10%) | 7/12 (58.3%) | |
| Medical oncology | 8/16 (50%) | 6/11 (54.5%) | 6/12 (50%) | |
| Radiation oncology | 3/14 (21.4%) | 5/11 (45.5%) | 3/12 (25%) | |
| Nuclear medicine | 1/14 (7.1%) | 1/10 (10%) | 4/12 (33.3%) | |
| Radiology | 1/14 (7.1%) | 1/11 (9.1%) | 2/12 (16.7%) | |
| No. of associated lecturers | 0 (0–1) | 1.5 (0.5–3) | 3 (1–5) | <.001 |
| No. of PhDs contracted | 0 (0–0) | 0 (0–0) | 0 (0–0.5) | .78 |
| No. of full professors | 0 (0–0) | 0 (0–1) | 0 (0–1) | .07 |
| No. of professors | 0 (0–0) | 0 (0–0) | 0 (0–0) | .62 |
| No. of publicly funded research projects | 0 (0–0) | 0 (0–1) | 1.5 (1–3) | <.01 |
| Ways of improving research activity | ||||
| Dedicated research time | 25/25 (100%) | 15/15 (100%) | 14/14 (100%) | |
| Training in methodology/analysis | 19/24 (79.2%) | 12/14 (85.7%) | 10/13 (76.9%) | |
| Support in methodology/analysis | 21/23 (91.3%) | 13/15 (86.7%) | 11/12 (91.7%) | |
| Public funding | 21/24 (87.5%) | 14/14 (100%) | 13/13 (100%) | |
| Private/industry funding | 15/23 (65.2%) | 11/13 (84.6%) | 13/13 (100%) | |
| Participation in multicenter studies | 23/24 (95.8%) | 15/15 (100%) | 12/12 (100%) | |
| Collaboration with AEDV and its Research Unit | 22/23 (95.7%) | 15/15 (100%) | 13/13 (100%) | |
| Research is not important | 3/18 (16.7%) | 2/11 (18.2%) | 0/9 (0%) | |
Abbreviations: AEDV, Academia Española de Dermatología y Venereología (Spanish Academy of Dermatology and Venereology); RIT, resident in training.
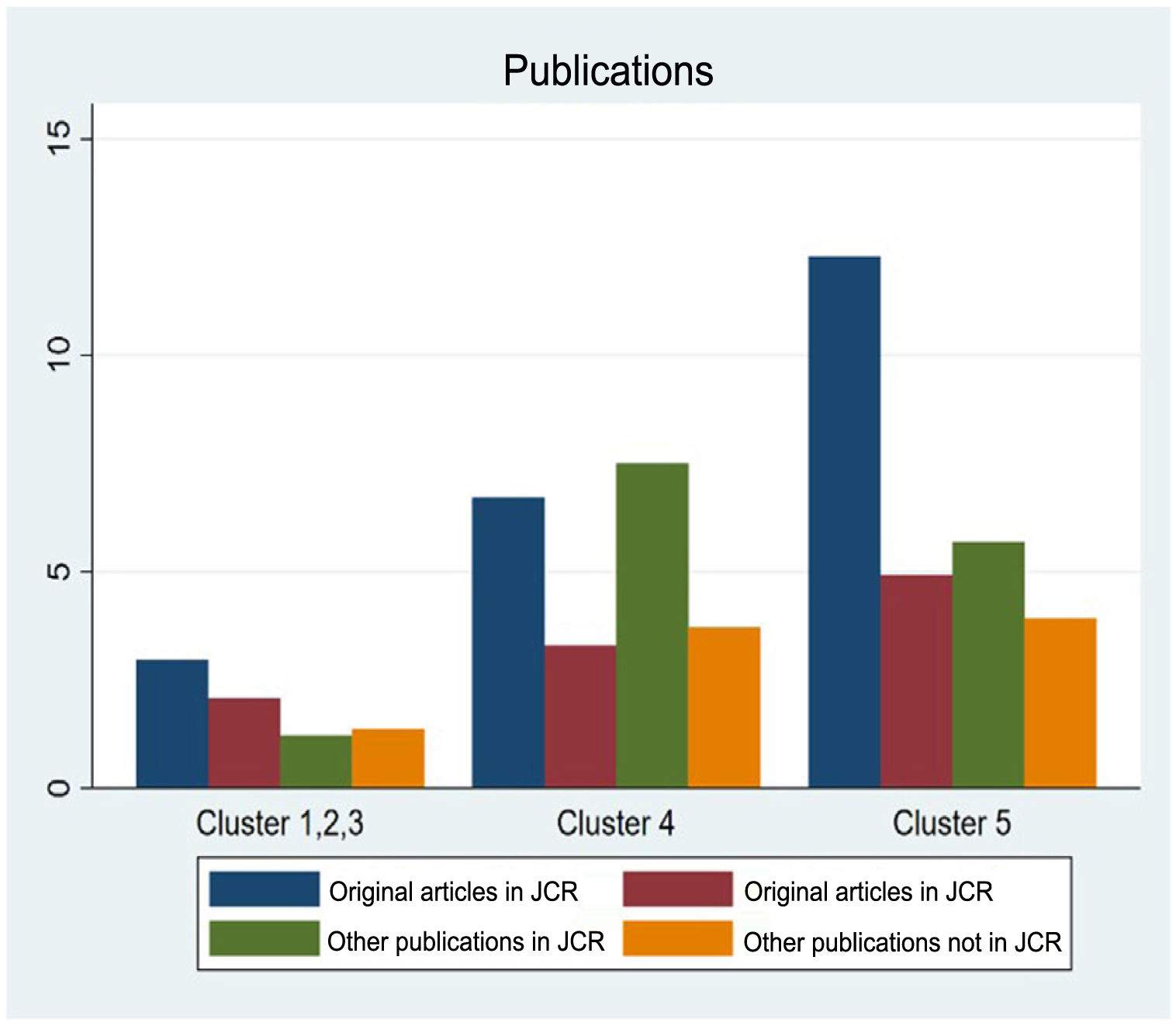
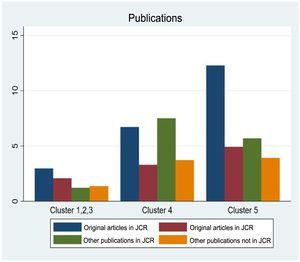
The number of publications by dermatologists from the department was again greater in large complexes, especially for original articles indexed in the Journal Citation Reports (Fig. 3).
Other activitiesThe total number of hospital admissions was greater and the associated length of stay shorter in the departments of large complexes. Participation in multidisciplinary committees was more common in high-complexity hospitals and large complexes, the most frequent being for melanoma and nonmelanoma skin cancer. The median number of interdepartmental consultations concerning patients admitted to other departments was higher in large complexes. In hospitals of low and medium complexity, interdepartmental consultations were addressed mainly by departmental staff physicians, whereas in high-complexity institutions and large complexes, the most frequent approach was for consultations to be managed by residents in training accompanied by staff physicians.
Channels for direct communication with primary care were more common in large complexes, the most frequent being telephone and electronic mail. Between 30% and 40% of departments from all types of hospital were involved in citizen engagement activities, the most common being patient education and workshops/information talks.
As for dermatology on-call shifts, these were only taken by staff physicians in the departments of large complexes in the evening. Depending on the type of hospital, only 20–30% of residents in training took dermatology on-call shifts of 17h on weekdays and 24h on weekends, and between 30% and 60% did not take on-call shifts. Dermatology on-call shifts began during the second year, with 5–6 per month. The main role of dermatologists during on-call shifts was consultations via pager from emergency department staff. Dermatologic emergencies during working hours were managed mainly in the general emergency department, with referral to dermatology when necessary. As for on-call shifts in general emergency departments, these were taken by residents in training in most hospitals, especially in hospitals of low and medium complexity and in high-complexity centers. There were generally between 4 and 5 per month over a period of 1 year (Table 8).
Other activities.a
| Hospitals of low and medium complexity | High-complexity hospitals | Large hospital complexes | P Value | |
|---|---|---|---|---|
| Total no. of admissions to hospital 2019 | 17.5 (15–50) | 22 (9–39) | 30 (14–40) | .94 |
| Median length of stay, d | 6.5 (5–7) | 7 (5–7.6) | 3.1 (2–4) | <.05 |
| Participation in multidisciplinary committees | ||||
| Yes | 19/25 (76%) | 12/13 (92.3%) | 12/12 (100%) | .11 |
| No | 6/25 (24%) | 1/3 (7.7%) | 0 (0%) | |
| Committees | ||||
| Melanoma | 15/19 (78.9%) | 12/12 (100%) | 12/12 (100%) | – |
| Nonmelanoma skin cancer | 16/19 (84.2%) | 8/9 (88.9%) | 12/12 (100%) | |
| Vascular abnormalities | 1/14 (7.1%) | 4/9 (44.4%) | 8/10 (80%) | |
| Pharmacy | 13/18 (72.2%) | 9/10 (90%) | 8/9 (88.9%) | |
| Median no. of interdepartmental consultations (weekly admissions) | 5 (4–10) | 10 (7–12) | 20 (15–24) | <.0001 |
| Who manages interdepartmental consultations? | ||||
| Residents | 1/25 (4%) | 3/14 (21.4%) | 1/12 (8.3%) | <.01 |
| Staff physicians | 20/25 (80%) | 4/14 (28.6%) | 4/12 (33.3%) | |
| Residents accompanied by staff physicians | 4/25 (16%) | 7/14 (50%) | 7/12 (58.3%) | |
| Channels of communication with primary care | ||||
| Yes | 13/25 (52%) | 9/14 (64.3%) | 10/12 (83.3%) | .18 |
| No | 12/13 (48%) | 5/14 (35.7%) | 2/12 (16.3%) | |
| Type of channel | ||||
| Telephone | 13/13 (100%) | 9/9 (100%) | 8/8 (100%) | – |
| 10/12 (83.3%) | 5/5 (100%) | 8/8 (100%) | ||
| Forum | 1/8 (11.1%) | 1/4 (25%) | 1/5 (20%) | |
| Citizen engagement activities | ||||
| Yes | 7/24 (29.2%) | 5/14 (35.7%) | 4/10 (40%) | .81 |
| No | 17/24 (70.8%) | 9/14 (64.3%) | 6/10 (60%) | |
| Type of activity | ||||
| Patient education | 4/6 (66.7%) | 3/5 (60%) | 4/4 (100%) | – |
| Focus groups | 2/5 (40%) | 3/3 (100%) | 0/2 (0%) | |
| Workshops/informative talks | 7/7 (100%) | 4/4 (100%) | 4/4 (100%) | |
| Do residents work on-call shifts? | ||||
| No | 4/10 (40%) | 6/10 (60%) | 3/10 (30%) | .41 |
| Yes, in the evenings | 4/10 (40%) | 1/10 (10%) | 5/10 (50%) | |
| Yes, 17 or 24h | 2/10 (20%) | 3/10 (30%) | 2/10 (20%) | |
| Year of internship when the resident starts dermatology on-call shifts | 2 (2–2) | 2 (2–2) | 2 (2–2) | .9 |
| Median no. of dermatology on-call shifts per month per resident | 5.5 (5–8) | 5 (5–6.5) | 6 (4–6) | .72 |
| Patients who visit the emergency department in the morning (Monday to Friday) | ||||
| Are seen directly in the dermatology department | 1/25 (4%) | 1/13 (7.7%) | 0/12 (0%) | .84 |
| Are seen in the emergency department | 4/25 (16%) | 1/13 (7.7%) | 2/12 (16.7%) | |
| Are seen in the emergency department and sent to dermatology if necessary (directly or referred) | 20/25 (84.6%) | 11/13 (84.6%) | 10/12 (83.3%) | |
| Care is delayed until the on-call dermatologist arrives | 0/25 (0%) | 0/13 (0%) | 0/12 (0%) | |
| During the on-call shifts, the dermatologist | ||||
| Is the first person called | 2/5 (40%) | 1/4 (25%) | 3/8 (37.5%) | 0.55 |
| Is consulted via pager | 2/5 (40%) | 3/4 (75%) | 5/8 (62.5%) | |
| Has a closed schedule | 1/5 (20%) | 0/4 (0%) | 0/8 (0%) | |
| Belongs to the suture pool | 0/5 (0%) | 0/4 (0%) | 0/8 (0%) | |
| Belongs to the internal medicine pool | 0/5 (0%) | 0/4 (0%) | 0/8 (0%) | |
| Do residents take emergency room on-call shifts? | ||||
| Yes | 10/10 (100%) | 9/10 (90%) | 7/11 (63.6%) | .06 |
| No | 0/10 (0%) | 1/10 (10%) | 4/11 (36.4%) | |
| Years during which the resident carries out general on-call shifts | 1 (1–1) | 1 (1–1) | 1.5 (1–2) | .25 |
| Median no. of monthly general on-call shifts per resident | 5 (4–5) | 4 (3–4) | 4.5 (4–5) | .07 |
aThe results are expressed as median (interquartile range) or absolute (relative) frequency. Statistically significant differences are shown in bold.
In this study, we explored the situation and the characteristics of dermatology departments of public hospitals in Spain by analyzing differences between centers of varying levels of complexity. As was to be expected, resources—staff, infrastructure, and equipment—were generally superior in more complex hospitals. As for caseload, the number of patients seen and more specialized procedures performed were also greater in these hospitals. Similarly, teaching and research activity was greater in more complex centers.
We recorded staff shortages compared with the number of professionals considered ideal in all the hospitals. In addition, hospitals of low and medium complexity were characterized by shortages in terms of structural number. The main cause of this shortage was the absence of interested applicants, probably owing to a lack of dermatologists and geographic location, as well as to working conditions considered poor in terms of salary/stability of contracts and that are worse than those found in private clinics, or to a combination of these factors. The last 5 years has seen a relative increase of almost 37% in the number of places offered in specialist health care training for dermatology (82 places in the 2016 call compared with 112 in the most recent [i.e., 2020])9; therefore, it is expected that the problem of a lack of dermatologists in the future will be resolved. The public administration should offer better employment contracts to ensure that dermatologists do not leave the public health sector.
The availability of basic equipment/techniques, such as cryosurgery, electrosurgery, patch tests, photodynamic therapy, and Wood lamps, was good in all types of hospitals. Of note, photodynamic therapy was more readily available than reported in the AEDV White Paper.1 The availability of ultrasound, digital dermoscopes, and phototherapy devices was also good, especially in large complexes. Other, more specific devices and infrastructure were more readily available in more complex centers. This was as expected, since departments at these institutions are larger and more likely to provide subspecialties and have national reference units in some cases. Compared with data from the AEDV White Paper, the number of operating rooms and treatment rooms was similar, whereas access to the day hospital was better.1
While the number of clinics (physical space) in large complexes was higher, the number of monthly appointment schedules was lower. However, the total number of initial visits during 2019 was greater in hospitals of low and medium complexity and similar to that of high-complexity centers. This may be because of the higher number of initial visits in the appointment schedule of outpatient clinics in large complexes or because the number of virtual visits in these centers is notably higher than in the others, thus also explaining the differences observed with respect to the time the patient spends on the waiting list. Teledermatology makes it possible to substantially reduce the time needed for health care.10 Its use is governed by a series of medical–legal requirements in terms of patient autonomy, safety, professional secret, confidentiality, privacy, and data protection, which must be taken into account by any departments offering care via this channel.11,12 The role of teledermatology has increased considerably during the COVID-19 pandemic.13 With respect to previous research, a greater number of patients per appointment schedule has been observed (around 30 in hospitals and 35 in outpatient clinics, compared with approximately 28 in DIADERM and 25 in the AEDV White Paper), as has a much more frequent use of teledermatology (around 60% compared with 1% in DIADERM).1,2 Time per patient at the initial visits was similar to that reported in the AEDV White Paper (around 10min, depending on the type of initial visit), whereas for checkups it was greater (9–10 vs 7min).1
Specialist units were also more common in high-complexity centers and large complexes. Compared with data from the AEDV White Paper, there was a notable increase in the number of psoriasis units and the emergence of hidradenitis suppurativa units (not recorded in the White Paper).1 A high percentage of participants would like a quality accreditation system in these units. Implementation of quality systems could be facilitated by initially selecting the most appropriate units, that is, those that currently have a greater degree of implementation (psoriasis, dermatology–oncology, hidradenitis suppurativa, pediatric dermatology, and digital dermoscopy).
As for surgical activity, a high percentage of departments had an operating room with an anesthetist. More interventions were carried out in hospitals of higher complexity, both with and without an anesthetist. These centers were also characterized by more specific procedures such as selective sentinel lymph node biopsy and Mohs micrographic surgery. Time on the waiting list is longer in large complexes, probably because of insufficient availability of operating rooms due to the local caseload.
Research activity was superior in large complexes, with more projects publicly funded through competitive calls and publication of more articles. Other authors have also reported a larger number of published articles and cumulative citations in large hospitals,3 due in part to the greater presence of residents,4 as we observed for departments at large complexes. The percentage of departments with residents in our study (64.4%) was superior to that reported in the AEDV White Paper (46%).1 According to the participants, original articles were the most published type, in contrast with data reported in the MaIND study1 and in the White Paper, where case studies were the most frequent type.1,5 The number of monthly clinical sessions and university lecturers was greater in larger complexes. Participants were interested in improving research in their departments, with the key points being availability of dedicated research time, funding, participation in multicenter projects, and collaboration with the AEDV and its Research Unit. Therefore, these areas should constitute priority lines if we are to facilitate research in our dermatology departments.
The number of hospital admissions was greater in large complexes, which also had more beds, although the number of admissions was generally low, probably owing to more frequent outpatient care provided to patients today or to the possibility that dermatology patients are being admitted to other departments.6 Participation in multidisciplinary committees was greater in high-complexity centers and large complexes, reflecting the higher degree of specialization in these areas. The number of interdepartmental consultations regarding patients admitted to other services was greater in large complexes; given the higher number of residents in training, these hospitals were more active in responding to consultations of this type. The presence of dermatologists in hospital on-call shifts was generally scarce and inferior to that observed in the AEDV White Paper,1 thus explaining in part the low number of admissions to dermatology services, since most came from the emergency department.6
The main limitation of our study was the low rate of participation by those invited to complete the survey, especially in low-complexity hospitals.
In conclusion, we present the results of a study mapping dermatologic care in Spanish public hospitals. Our findings provide an idea of the current situation of Spanish dermatology departments in terms of activity and structural and care resources immediately before the COVID-19 pandemic and may help to define lines of work and areas for improvement. It will now be necessary to analyze how the pandemic has affected the running and structure of the departments.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We are grateful to all the participants for taking the time to complete the questionnaire and to Miguel Ángel Descalzo Gallego and Ignacio García Doval for their invaluable help. This research was carried out in cooperation with the Research Unit of AEDV and was developed in part during the period of the Juan de Azúa grant awarded to Carlos Cuenca Barrales in 2019.