Skin cancer deaths continue to rise despite the implementation of numerous preventive campaigns and programs. The aim of this systematic review was to evaluate reviews of primary and secondary skin cancer prevention strategies as reported over the past 10 years. We analyzed 63 systematic reviews and meta-analyses: 30 (46.6%) addressing primary interventions and 35 (55.6%) addressing secondary interventions. Two of the reviews covered both. The most widely reported primary prevention approaches were education programs (63.3%), followed by risk modeling to identify individuals at high risk for melanoma (17.6%), and the promotion of sunscreen use (11.8%). The most widely reported secondary prevention measures concerned imaging systems for early skin cancer detection (40%), smartphones and new technologies (22.9%), and visual diagnosis in population-based screening (17.4%). The most effective measures were primary prevention education programs to improve sun protection habits.
La mortalidad por cáncer de piel continúa aumentando a pesar de las numerosas intervenciones dedicadas a su prevención. El objetivo de esta revisión es estudiar la situación de la prevención primaria y secundaria del cáncer de piel en los últimos 10 años. Se incluye un total de 63 revisiones, 30 (46,6%) revisiones incluyeron estrategias de prevención primaria y 35 (55,6%) de prevención secundaria, incorporando 2 de las revisiones información sobre ambos tipos de estrategias. Para la prevención primaria, las medidas más estudiadas fueron los programas educativos (63,3%), seguidos de la creación de modelos para identificar a personas con alto riesgo de desarrollar un melanoma (17,6%) y la promoción del uso de fotoprotectores (11,8%). Los sistemas de toma de imagen para el diagnóstico precoz del cáncer de piel (40%), seguidos por el empleo de smartphones y nuevas tecnologías (22,9%), así como el diagnóstico visual como cribado poblacional (17,4%), fueron las medidas de prevención secundaria más evaluadas. De todas las medidas revisadas, las estrategias de prevención primaria centradas en programas educativos para mejorar los hábitos de fotoprotección fueron las que resultaron más efectivas.
Skin cancer is the most frequent type of cancer in the world. The main risk factor for developing skin cancer is exposure to sunlight, which can be acted upon.1,2
Skin cancer can be classified as melanoma skin cancer and nonmelanoma skin cancer (NMSC).3 Melanoma is an aggressive, highly metastatic cancer,4 in which the clinical and pathological variety is affected by the type of sun exposure. Intermittent exposure and sunburn during infancy and adolescence predispose individuals to superficial spreading melanoma, whereas long-term exposure predisposes to lentigo maligna melanoma. Nodular melanoma has been associated with both intermittent and long-term exposure to sunlight. Acral lentiginous melanoma is not associated with exposure to sunlight.5
NMSC includes basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), together with other, less common types of skin cancer. BCC is the most common malignant tumor in humans, accounting for 60% of all skin tumors, and is associated with intermittent exposure to sunlight during an individual's lifetime.6,7 SCC is associated with cumulative exposure over time.8
The incidence and mortality of skin cancer have risen in recent years. This rise has been associated with an increase in exposure to sunlight, an increase in the number of immunosuppressed persons (immunosuppression is also a risk factor for skin cancer), and increased overall survival of the population.9,10 In Spain, the incidence of BCC was 253.2 per 100000 person-years, that of SCC was 38.2 per 100000 person-years, and that of melanoma 8.8 per 100000 person-years.11 Mortality has also increased in recent years and now stands at 2.2 per 100000 person-years12–14 compared with 1.8 per 100000 person-years in 2001.15 In Australia, the measures implemented to prevent skin cancer some decades ago have clearly proven able to reduce incidence.2 However, data reported for the Spanish population suggest that the primary preventive strategies implemented are insufficient or inappropriate.16
The World Health Organization defines primary prevention as the set of measures that act on factors that cause and predispose to disease in order to reduce their incidence, whereas secondary prevention involves early diagnosis of incipient (asymptomatic) disease in order to enable early treatment, thus avoiding severe consequences and improving survival.17
The objective of this review was to explore primary and secondary measures for prevention of skin cancer during the last 10 years.
Material and MethodsDesign and Search CriteriaWe designed a systematic literature review to answer the following research questions:
- •
What are the most widely studied primary and secondary prevention methods at present?
- •
What interventions for preventing skin cancer have been implemented at the population level during the last 10 years?
- •
Are these measures really effective for preventing skin cancer?
- •
Are the strategies currently being applied in the population sufficient for preventing skin cancer?
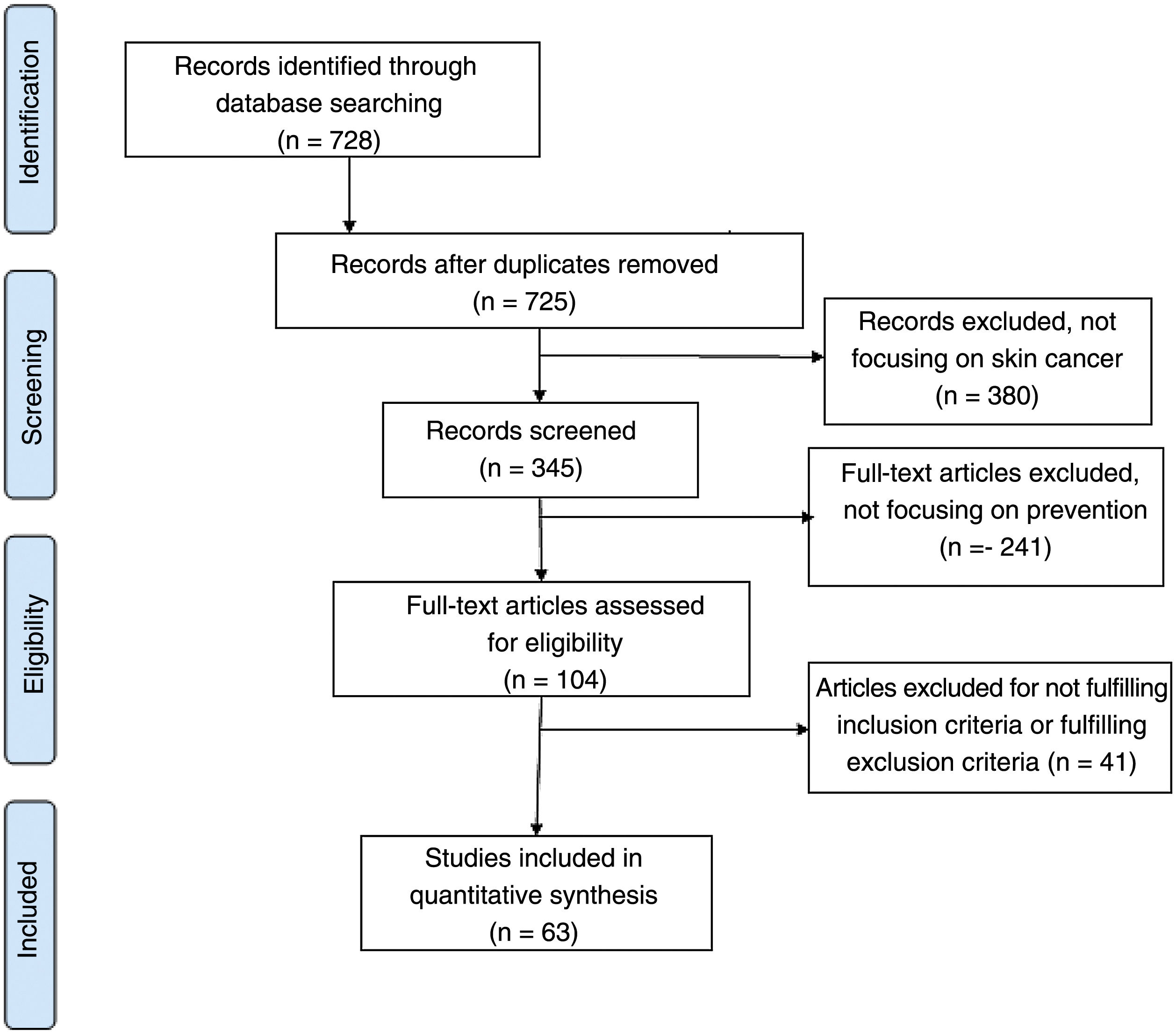
On March 15, 2021, we carried out a bibliographic search of the Medline databases of all articles published from January 1, 2011 to March 14, 2021. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines using the following search algorithm: (“skin cancer” OR “melanoma”) AND (“prevention” OR “screening” OR “primary prevention” OR “secondary prevention”).
Inclusion and Exclusion CriteriaThe search was limited to systematic reviews and meta-analyses from the last 10 years in English, Spanish, Italian, French, and German that included information associated with primary and secondary prevention (screening) of skin cancer. We excluded articles with other types of design, reviews focusing on risk and etiologic factors or treatments, articles on prevention for high-risk populations (patients with a previous diagnosis of melanoma, immunodepressed patients, and other special situations), and articles on advanced diagnostic systems focusing on the individual patient and not applicable at the population level (diagnosis based on confocal microscopy and optical coherence tomography).
Selection of StudiesTwo investigators (CAB and ABE) performed the first screen and independently reviewed the titles and abstracts of the articles found in the first search to identify relevant studies. We reviewed the full text of all those articles fulfilling the inclusion criteria and checked the bibliographic references to search for additional sources. Those articles considered relevant by both investigators were included in the review. Disagreements on the exclusion or inclusion of articles were discussed until agreement was reached. If agreement was not reached, then a third investigator (SAS) made the final decision.
VariablesWe collected information on the type of prevention strategy (primary or secondary), the author, type of tumor, target population, intervention, setting for application (primary care, hospital care, or other), and conclusions.
ResultsThe search yielded a total of 728 articles, of which 63 were eventually included (Fig. 1). Thirty reviews (46.6%) included primary prevention strategies and 35 (55.6%) included secondary prevention strategies. Two of the reviews included information on both types of strategy. The prevention strategies focused mainly on preventing melanoma or skin cancer in general.
Primary PreventionWe included 30 reviews on primary prevention. The usefulness of educational programs was the most widely studied measure (n=19, 63.3%) (Table 1). Six reviews (20%) evaluated models for identifying people with a high risk for melanoma, 4 (13.3%) contained information on the use of sunscreen, and 1 (3.3%) included information on the legislation applying to the use of sunbeds.
Articles Included in the Review on Primary Prevention.
| Primary prevention | |||
|---|---|---|---|
| Method | No. of reviews | Additional information | Conclusions |
| Educational measures | 19 | - Reminders- Educational images- Physical appearance- UV index- Educational programs | Improve behaviors through self-informationImprove behaviors, especially if the images focus on appearance. All images are of White personsImprove behaviors more than interventions focusing on healthNot useful, as not understood by general populationUseful in the various settings where they are applied and improve behaviors, although they are insufficient and policies to support them are lacking |
| Risk assessment models | 6 | Melanoma | Report the usefulness of risk protection models for identification of persons with a high suspicion of melanoma and who are candidates for exhaustive prevention measures. Validated models are necessary before systematic use in clinical practice |
| Use of sunscreen | 4 | Melanoma and nonmelanoma skin cancer | The association between reduced incidence of melanoma and use of sunscreen is weak, probably because use of sunscreen is linked to increased exposure. With respect to nonmelanoma skin cancer, sunscreen has proven effective for prevention of actinic keratosis and squamous cell cancer, whereas this efficacy is less clear for basal cell cancer |
| Tanning booths | 1 | Melanoma in young people | Legislation regulating the use of sunbeds is associated with a reduction in their use |
Educational programs were the most widely studied primary prevention strategy (n=19, 63.3%). Measures to prevent skin cancer are cost-effective.18 Informative images are an effective way to improve attitudes, knowledge, and behavior with respect to sun protection and the effectiveness of self-examination.19–21 Images can also affect the way people perceive the attractiveness of tanned skin.21
Two reviews analyzed the impact of reminders via text messages and email on the prevention of skin cancer.22,23 The authors found that reminders reduce the number of cases of sunburn; however, since the information was self-reported, they were unable to conclude that this measure had a real impact on the prevention of skin cancer.23 A review of 5 trials reported that reminders via text messages had no beneficial effects on sun protection habits.22
Prevention strategies focusing on physical appearance and skin aging have also been evaluated, revealing that in terms of sun protection, strategies focusing on physical appearance were more effective than those focusing on health, since tanned skin is usually associated with concerns over cosmetic appearance.24,25 Educational interventions focusing on physical appearance reduce exposure to the sun's rays and improve people's intentions and habits with respect to sun protection immediately after application and up to 1 year later.24 General knowledge of the Global Solar UV Index is poor,26 and it is not clear whether an understanding of the index affects attitudes to sun protection, since this has been associated with higher-risk behavior and more frequent deliberate exposure to sunlight, as well as with lower-risk behavior, in the form of a fewer cases of sunburn.27
As for implementation of education strategies for prevention in specific settings, 3 reviews focused on the occupational setting.28–30 Knowledge of and attitudes toward sunlight differ between workers, and there are even some people who have never heard of skin cancer.28 Educational interventions in the workplace are effective for improving sun protection habits among people who work outdoors and for reducing the frequency of sunburn.29 Educational and multicomponent interventions increase the use of personal protection material, such as sunscreen; however, there is less evidence on the effectiveness of policies or the specific components of the intervention.30
Interventions targeting school children have shown promising results.31–33 Education programs on prevention are more useful when applied to younger school children than to adolescents.33 Education programs in primary and secondary schools led to improved sun protection knowledge and habits, although few studies led to reduced sun exposure time.31 The results reported were considerably heterogeneous, except for the improvement in attitudes toward the appropriateness of tanned skin. Sunburn and nevus counts were evaluated less frequently, although around half of the studies reported a reduction in the number of burns and nevi after application of prevention strategies.31
In outdoor settings, providing free sunscreen attracted considerable interest among the public, although no clear results were established on its effectiveness.32 Interventions implemented among tourists were ineffective, with strategies based on images of photoaging the only ones that proved to be of notable use.34
Multicomponent community interventions increased the use of sunscreen and reduced sun exposure.35 Interventions implemented through the media alone were not effective, although they did slightly improve sun protection habits.35 Behavioral interventions implemented through primary care served to improve sun protection habits and skin self-examination. However, they did entail an increase in the number of unnecessary diagnostic and therapeutic procedures, with no reduction in the number of cases of sunburn or in the incidence of skin cancer.36
Risk Assessment SystemsSix reviews (20%) analyze the usefulness of identifying people at high risk of melanoma and who would be candidates for preventive measures, follow-up, and early and exhaustive screening.37–42
Many risk prediction models are available, although they differ in terms of the risk factors included. The most commonly included risk factor is the nevus count.37,38 Other factors included in the models are degree of sun exposure, the presence and density of freckles, history of sunburn, hair color, skin color, and age.37–39 Internal and external validation of these models is uncommon, and other performance measures and their application in clinical practice are rarely reported.37,39 Two reviews showed the discriminatory capacity of the models to be low owing to heterogeneity in the selection and evaluation of risk factors. The authors state that it is difficult to draw comparisons between the models owing to differences in methodology during development.37,39 Nevertheless, another review showed that despite the disparity between the factors included and the different sensitivity and specificity cut-offs, almost all the models had a similar discriminatory power, with sensitivity and specificity values that fit along a receiver operating characteristic curve and an area under the curve of 0.755.38
A systematic review of international clinical practice guidelines also reported differences concerning which individuals are at high risk of melanoma. The most consistently included high-risk characteristics were the presence of multiple melanocytic nevi, dysplastic nevi, family history of melanoma, giant congenital nevi, and Fitzpatrick skin types I and II.40
Identification of persons at risk of melanoma and application of preventive behaviors improved sun protection habits and increased the frequency/thoroughness of skin self-examination.41 Moreover, detection of gene mutations that predispose to melanoma in persons with a family history of risk impacted behaviors for prevention of skin cancer, although there is no evidence on measures to be taken, recommendations, or follow-up of affected patients.42
Use of SunscreenThe effect of sunscreen as a preventive measure was evaluated in 4 reviews (13.3%).3,43–45 The association between the use of sunscreen and reduced risk of melanoma is weak and heterogeneous, since the use of sunscreen may be associated with increased sun exposure owing to the false sense of security it provides and, on occasion, inappropriate application.43,44 One review showed that the use of sunscreen did not increase the risk of melanoma, BCC, or SCC.3 Sunscreen was also effective for reducing the frequency of actinic keratosis and SCC,45 as well as that of BCC, although this association is less clear.45
Other Primary Prevention MeasuresOne review found that legislation regulating the use of tanning beds was associated with a decreased frequency of use.46
Secondary PreventionA total of 35 reviews provided information on secondary prevention strategies (55.5%) (Table 2). The most widely studied strategy was digital imaging systems for early diagnosis with dermoscopy or artificial intelligence systems (n=14, 40%). Eight reviews (22.9%) included information about strategies based on the use of a smartphone as a diagnostic system or as a teledermatology tool, 6 (17.4%) on visual diagnosis and its role in population screening, and others on various topics.
Articles Included in the Review on Secondary Prevention.
| Secondary prevention | |||
|---|---|---|---|
| Method | No. of reviews | Additional information | Conclusions |
| Early diagnosis with imaging systems | 14 | - Dermoscopy- AI- TBP | Useful in early diagnosis, and more so if used in high-risk patients. Favors diagnosis during early stages of melanoma and BCC, especially if combined with visual inspection and used by dermatologists. Could prove useful in primary careNot yet shown to be effective. Under developmentUseful for the diagnosis of early-stage melanoma in high-risk patients. Criteria for implementation must be set |
| Smartphones and new technologies | 8 | - Apps for early diagnosis- As an aid in teledermatology | Apps cannot yet be considered reliable. Only developed for melanomaUseful tool for facilitating consultations with the primary care dermatologist by making best use of the patient's time and reducing the number of referrals. Implies greater workload, lack of clinical information for diagnosis, and more consultations. Standardized clinical guidelines are necessary to regulate their use |
| Visual examination | 6 | - As a diagnostic method- As population screening- Self-examination | This approach is insufficient and depends on the professional performing the examination. Should be combined with dermoscopyCost-effective in high-risk patients. No benefit when applied to healthy persons, since it leads to overdiagnosis and unnecessary treatmentNo benefits |
Abbreviations: AI, artificial intelligence; BCC, basal cell cancer; TBP, total body photography.
Fourteen reviews (40%) evaluated the effect of imaging techniques on secondary prevention of skin cancer. Eight evaluated dermoscopy (57.1%), 4 artificial intelligence (28.6%), and 2 total body photography (14.3%).
Combined with an exhaustive clinical history and visual inspection, dermoscopy favored early diagnosis of melanoma and NMSC when used by dermatologists.47–54 Furthermore, follow-up of persons at high risk of melanoma with digital dermoscopy increased the number of melanomas treated in early stages.47 Its usefulness in primary prevention is more controversial.48–51 Dermoscopy proved to be a useful technique for urgent referral of patients at high risk of skin cancer49 and for differentiating between benign and malignant lesions.48,50 Nevertheless, there are no structured algorithms showing the accuracy of dermoscopy for detection of SCC.52
Artificial intelligence consists of the development of neuronal networks that can analyze images of skin lesions in order to provide a diagnosis. Together with a physical examination and dermoscopy, artificial intelligence has proven to be a useful method for early diagnosis of skin cancer, especially melanoma, even in primary care.55–58 Nevertheless, this approach is still under development and requires the participation of dermatologists to improve the technology so that it can be applied in future clinical practice.58
Total body photography has proven useful for the diagnosis of early-stage melanoma in high-risk patients. However, further studies are necessary to determine the factors that make it possible to identify this high-risk population and enable appropriate implementation of programs in clinical practice.59,60
Smartphones and New TechnologiesEight reviews (22.9%) studied the effect of smartphones and new technologies on secondary prevention of skin cancer.61–68 Smartphone applications for the diagnosis of skin cancer are not reliable because they are only designed to distinguish between melanoma and other lesions.61–63 Variations in skin lesions in the general population and in image quality made it difficult to diagnose skin cancer using these applications.64 In the case of teledermatology, smartphones and other technological devices did in fact prove useful for enabling referrals to dermatology from primary care, thus optimizing waiting time and reducing the number of in-person referrals. This approach proved especially useful in rural areas, where attending a hospital is difficult.65–67 The main obstacles to implementation were increased workload and lack of clinical information on which to base a diagnosis.63 Guidelines are necessary for standardization of the techniques used to obtain, store, and review images,65 as are studies for prospective and practical evaluation of the ability of this channel to provide an accurate diagnosis and classify lesions.66
Visual Inspection and Population ScreeningSix reviews (17.4%) that analyzed the impact of skin cancer screening in the general population were unable to find benefits.18,33,69–72 Skin cancer screening did prove beneficial in high-risk patients69 and was cost-effective.18 However, screening of the general public for melanoma and NMSC based on whole body examination is not supported by evidence,33 since it is associated with overdiagnosis and inappropriate treatment, with psychosocial consequences for the public.70,71 Furthermore, used as the only diagnostic tool, visual inspection proved insufficient and depended on the professional who performed the examination.70 The effectiveness of skin self-examination for prevention of skin cancer is controversial.72
Other Secondary Prevention StrategiesEarly detection of skin cancer increased incidence, albeit with a specific increase in the rates of diagnosis of early-stage melanoma, and while this was associated with decreased mortality, the level of evidence remains low.73 The diagnostic delay observed in BCC entails increased costs and more complex surgical procedures.74 Nursing staff could play an important role in skin cancer screening, although their current level of training is insufficient to perform a whole body skin examination.75–77 Many educational interventions for prevention of skin cancer have focused on primary care physicians, although the effectiveness of this approach has not been evaluated.78 Similarly, the growing concern and awareness of skin cancer are leading to an increase in the number of unnecessary surgical procedures as a prophylactic approach for melanocytic lesions.79
DiscussionMultiple measures have been applied for the primary and secondary prevention of skin cancer. The most effective have been primary prevention strategies focusing on education programs aimed at improving sun protection habits. However, evidence is lacking for the direct impact of this approach on the morbidity and mortality of cancer. Screening of the general population is not effective, and it is necessary to develop models for evaluation and prediction of skin cancer in order to select those patients who are at greater risk of skin cancer and candidates for targeted interventions.
What are the Most Widely Studied Primary and Secondary Prevention Measures at Present?In primary prevention, most strategies focus on education programs aimed at increasing knowledge of risk factors in skin cancer and on the measures necessary to prevent it, with the greatest emphasis on sunscreen.19–21 The second most studied strategy was the implementation of risk assessment systems to identify persons at greater risk of skin cancer who are potential candidates for targeted prevention programs.37,38 The use of sunscreen was also evaluated,45 as was the existence of legislation on indoor tanning devices.80
The most widely evaluated secondary prevention strategies were as follows: early diagnosis based on imaging systems (including dermoscopy),47 artificial intelligence,58 and total body photography60; the use of smartphones as tools for diagnosing skin cancer64 and as an aid in teledermatology65; and visual inspection as a population screening technique.69
Smartphones and new technologies are increasingly used in many areas of medicine,81–83 with dermatology being one of the specialties where this approach is has most frequently been implemented.84 However, most of these tools require additional assessments to clearly demonstrate their effectiveness.63,66 The use of new technologies, such as smartphones and instant messaging, could increase workers’ knowledge of sun exposure and reduce the incidence of skin cancer.28 Smartphones could be more widely applied in teledermatology, although validated clinical guidelines are necessary to improve implementation.61,67 Artificial intelligence could play a major role in the link between dermatology and primary care.56,58,84,85
What Interventions for Preventing Skin Cancer Have Been Implemented at the Population Level in the Last 10 Years?Education strategies19–21 and skin cancer screening aimed at high-risk persons69 are the main skin cancer strategies at population level.
Education strategies have the greatest effect on prevention of skin cancer, since they improve sun protection habits among the population,29 although studies should be performed to establish a correlation with reduced morbidity and mortality of skin cancer.28 The yield of education programs is particularly good in children.18 This observation is highly relevant, since 75% of cases of skin cancer could be prevented with appropriate protection during childhood.15 The information in these programs should focus on the benefits of sun protection in terms of physical appearance, rather than on health and disease,24,25 and should be provided via visual images of sun damage.20,21 Given that tanned skin is a cosmetic issue, showing images of the damage caused by exposure to sunlight could have a considerable impact on the population. One example is the national campaign of the Healthy Skin Foundation (Fundación Piel Sana) of the Spanish Academy of Dermatology and Venereology (Academia Española de Dermatología y Venereología), which uses the slogan “A suntan is not synonymous with health and should not be synonymous with beauty” (El bronceado no es sinónimo de salud y no debería serlo de belleza).86
Education strategies improve people's behavior, although we should assess their impact in terms of incidence and mortality.36 These programs should also be supported by consistent policies that favor their application.28 The Australian campaign SunSmart, which was implemented more than 3 decades ago, has shown the importance of campaigns aimed at schoolchildren for improving sun protection habits.87 In Europe, we have the Euromelanoma project, a campaign that offers free skin examinations to the public. The campaign is implemented in Spain through the Healthy Skin Foundation, focusing on both primary and secondary prevention of skin cancer and offering free skin examinations, talks, and interventions at universities and schools and via social networks.86 Furthermore, the year 2020 saw the implementation of the campaign “Cuentos lunares, poemas y microrrelatos que salvan vidas” (Cuentos lunares: poems and flash-fiction that save lives)1 during the COVID-19 pandemic to disseminate the harmful effects of sun for the skin and possible prevention strategies through flash fiction and poems.88 In addition, through microinfluencers and social networks (Instagram, Facebook, and Twitter), members of the public, dermatologists, and other collaborators used a photograph as inspiration to write a poem or flash fiction on a common subject, namely, the observation of moles or beauty spots.88 This year, the campaign entitled “Misión Amarte” (literally “The love your skin mission”) is using social media to disseminate a message in favor of self-protection and care.89
Screening of the asymptomatic general public is not effective, leading to overdiagnosis and unnecessary treatment that increases the cost of health care and may have a negative impact on patients’ psychosocial health.70,71 Also potentially effective is screening of the high-risk population by dermatologists using a combination of visual inspection and dermoscopsy.69 When they are aware of this risk, more vulnerable persons improve their behavior.47 However, exactly which persons are considered high-risk and how to identify them remain unclear. We still require validated models to predict the risk of melanoma when selecting these patients37–39 and clinical practice guidelines to regulate the process of identification and subsequent follow-up.74 Ensuring that people can recognize clinical alarm signals with respect to pigmented and nonpigmented lesions could also favor early diagnosis of skin cancer.
Are These Measures Really Effective for Preventing Skin Cancer?After implementation, education programs show an improvement in sun protection habits, although it is difficult to evaluate the real impact in terms of the incidence of cancer-related mortality.29 Educational strategies seem to have had the greatest impact, especially those associated with physical appearance based on images.24,25 The implementation of legislation regulating the use of tanning beds has been associated with less frequent use, which could decrease the risk of melanoma.46 Risk prediction models for identifying persons who are more susceptible to melanomas are effective, although they have yet to be validated.40 Dermoscopy and total body photography, together with visual inspection and history-taking, favor early diagnosis of persons at high risk of skin cancer.47
Similarly, no association has been established between the isolated use of sunscreen with no additional measures or the UV score and reduced incidence of skin cancer.43,44 Screening for skin cancer among the general population was not effective and could lead to overdiagnosis and overtreatment.70,71 Apps for early diagnosis of skin cancer and artificial intelligence are both fields that are still under study.58
Clinical trials have shown that sunscreens reduce the risk of melanoma.90 However, the present review highlighted their lack of effectiveness as a preventive strategy, probably because of the association with risk behaviors, such as increased exposure to sunlight and inappropriate application.43,44 Educating the public about sun protection is a public health objective. Once implemented, education campaigns show that people who work outdoors improve their sun protection habits, although this strategy is insufficient without concomitant structural and political measures. It is necessary to draw up policies, such as the recommendations made in Germany, whose focus is multifaceted, including both behavioral (individual) and structural (social) approaches and favoring both general protective behaviors and personalized measures, such as modifying one's work timetable.91
Are the Strategies Currently Being Applied in the Population Sufficient for Preventing Skin Cancer?The incidence and mortality of skin cancer are increasing, despite the wide variety of preventive strategies available9,10; therefore, we can conclude that these measures are not completely effective. This may be because incorrect or inappropriate application prevents them from having a real impact on health.
New technologies for recording images could prove useful for the diagnosis of skin cancer and for facilitating preferential access to a dermatologist in cases of a high suspicion of skin cancer.52 Given that primary care is an individual's first contact with the health system, it would be necessary to train health professionals who are not dermatologists to differentiate between benign and malignant lesions. These professionals are an important part of the prevention process, although their current knowledge is suboptimal.52,75
Limitations(1) We only included systematic reviews and meta-analyses. Therefore, some preventive approaches have not been included (no reviews were available). (2) We only analyzed strategies for early diagnosis that are currently applied to reduce mortality. (3) The search was limited to the last 10 years.
Future Lines of ResearchStudies demonstrating the association between preventive strategies and the reduction in morbidity and mortality of skin cancer are warranted. Such measures improve sun protection habits and self-examination of skin lesions, although the direct impact on incidence and mortality remains unclear.
It is necessary to establish clinical practice guidelines and legislation that favor prevention of skin cancer, since an approach of this type can prove beneficial for public health and reduce costs for the health system.
ConclusionPrimary and secondary prevention of skin cancer is a very relevant issue. Population-based screening strategies are not justified. Early detection systems should be optimized in the case of high-risk patients. Educational programs are the most effective strategies. The fact that deaths from skin cancer are not decreasing shows that current prevention strategies are insufficient. Therefore, these should be improved, standardized, and regulated based on proven effective approaches in order reduce the impact of skin cancer on the population.
Conflicts of InterestThe authors declare that they have no conflicts of interest.