Although subungual melanoma is uncommon, it is associated with worse outcomes than melanomas in other locations and accounts for 1% to 23% of all melanomas, depending on the population. The aim of this study was to describe the clinical and histopathologic features of subungual melanoma in a Mexican population. We identified 303 patients with melanoma, and of these, 19% (57 patients with a median age of 71 years) had subungual melanoma. The main sites affected were the lower limbs (52.6%) and the toe (75.4%). The most common histologic subtype was acral lentiginous melanoma (50.9%). Median Breslow thickness was 3 mm, and stage IA tumors were the most common (in 28.1% of patients). Recurrence and metastasis occurred in 19.3% and 8.8% of patients, respectively. The clinical and histopathologic features identified are similar to those described in the literature. Early diagnosis and treatment are crucial for improving prognosis.
El melanoma subungueal es un tumor poco común, con peor pronóstico comparado con los de otras localizaciones. Corresponde al 1-23% de los melanomas, según la población. El objetivo de este estudio fue describir las características clínicas e histopatológicas del melanoma subungueal en la población mexicana. Se incluyeron 57 pacientes con melanoma subungueal (19% de los 303 melanomas totales), con una mediana de edad de 71 años. La localización predominante fueron los miembros inferiores (52,6% de los melanomas subungueales) y el primer dedo (75,4% de los casos). El subtipo histológico más frecuente fue el acral lentiginoso (50,9%). La mediana de Breslow fue de 3mm. El estadio IA fue el más frecuente (28,1%). Se encontró una tasa de recurrencia del 19,3% y de metástasis del 8,8%. Las características clínico-patológicas fueron semejantes a lo descrito en la literatura. Es importante realizar un diagnóstico y tratamiento tempranos de cara a mejorar su pronóstico.
Subungual melanoma (SUM) is a rare tumor of the nail matrix and bed that is associated with a worse prognosis compared to melanomas in other locations, mainly due to its advanced stage at diagnosis.1 It represents 1% to 3% of all the melanomas reported among Caucasians and up to 23% of all neoplasms reported among the Japanese population.1–3 The onset of SUM is more common between the 5th and 7th decades of life, with no gender predilection. Diagnosis can be challenging as it resembles other conditions, thus leading to delayed identification.4 The aim of this study was to describe the clinical and histopathological characteristics of SUM in Mexican patients treated at a tertiary referral center.
Materials and methodsThis was an observational, retrospective, descriptive, and longitudinal study of patients with subungual melanoma treated from January 2016 through January 2021 at the dermatology unit of Centro Médico Nacional La Raza in Mexico City, Mexico, a tertiary referral center that treat nearly 1000 patients each year. The study included patients older than 18 years with a histopathological diagnosis of malignant melanoma of the nail unit.
The following clinical-pathological variables were collected: affected finger, age, gender, education, affected limb (upper or lower), affected anatomical region (hand or foot, right or left), number of affected finger (1st to 5th), associated trigger prior to the appearance of the tumor (trauma, de novo, nevus), family history of melanoma, Breslow thickness, ulceration, positive sentinel lymph node, clinical stage, Hutchinson's sign, involvement of the hyponychium, presence of nail dystrophy, duration of the lesion until histopathological diagnosis, Clark level, mitotic index, perineural invasion, vascular invasion, tumor spread (local: no lymph node involvement; regional: lymph node involvement; distant: lymph node involvement beyond regional nodes or organs), recurrence, metastasis, and site of metastasis.
Descriptive statistics was used. The involvement of the hyponychium, Hutchinson's sign, the affected segment, and mortality were compared to gender, poor prognostic factors (recurrence, positive sentinel node, Breslow thickness, affected segment), and death using the chi-square test, or Fisher's exact test and the Mann-Whitney U test. P values<.05 were considered statistically significant. This study was approved by Centro Médico Nacional La Raza research ethics committee.
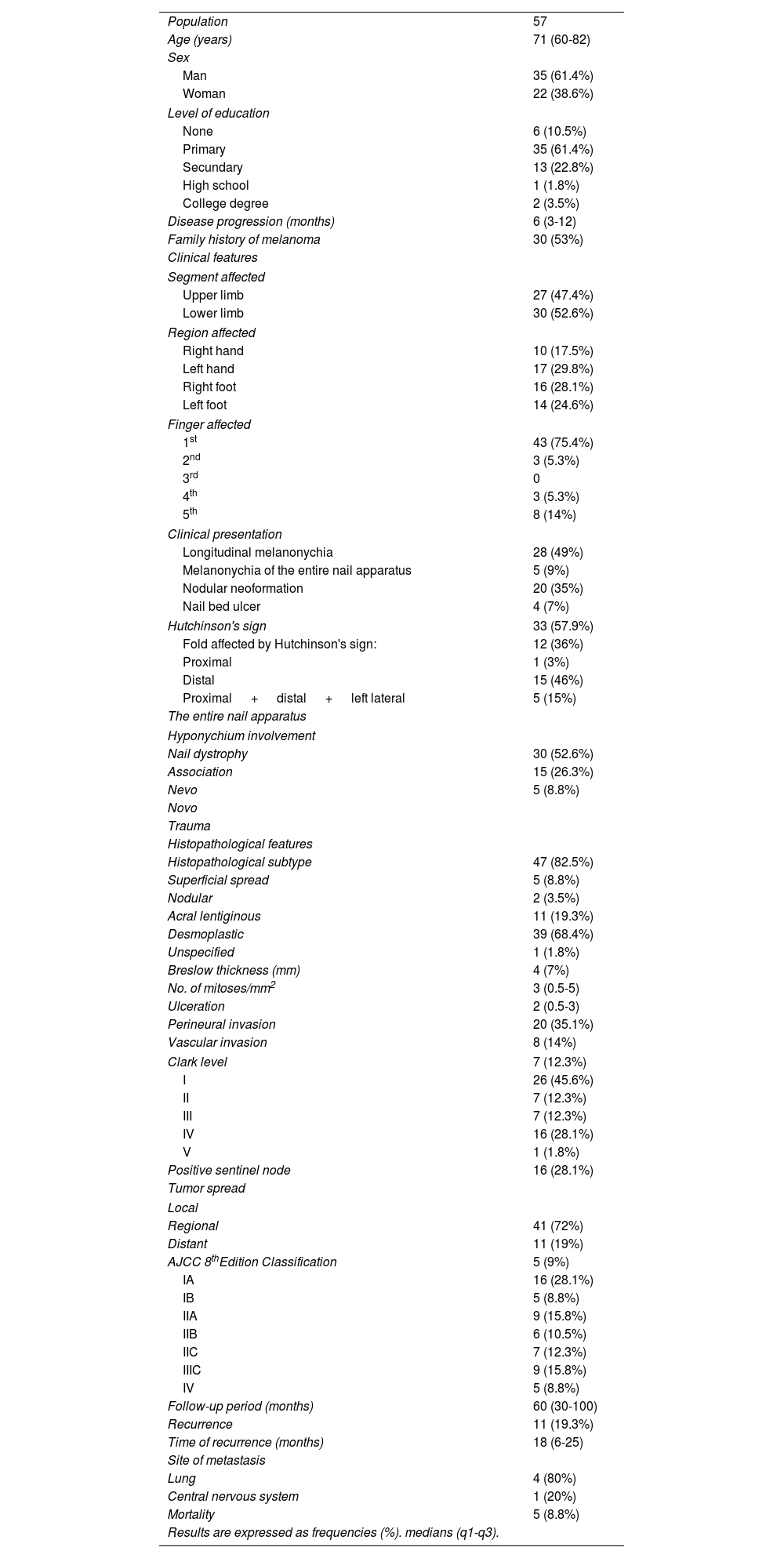
ResultsA total of 57 (19%) out of 303 patients diagnosed with melanoma were identified with subungual melanoma, with a median age of 71 years. Most patients were men (n=35; 61.4%), with a median 6-month evolution prior to diagnosis (Table 1).
Clinical and histopathological characteristics of patients with subungual melanoma.
| Population | 57 |
| Age (years) | 71 (60-82) |
| Sex | |
| Man | 35 (61.4%) |
| Woman | 22 (38.6%) |
| Level of education | |
| None | 6 (10.5%) |
| Primary | 35 (61.4%) |
| Secundary | 13 (22.8%) |
| High school | 1 (1.8%) |
| College degree | 2 (3.5%) |
| Disease progression (months) | 6 (3-12) |
| Family history of melanoma | 30 (53%) |
| Clinical features | |
| Segment affected | |
| Upper limb | 27 (47.4%) |
| Lower limb | 30 (52.6%) |
| Region affected | |
| Right hand | 10 (17.5%) |
| Left hand | 17 (29.8%) |
| Right foot | 16 (28.1%) |
| Left foot | 14 (24.6%) |
| Finger affected | |
| 1st | 43 (75.4%) |
| 2nd | 3 (5.3%) |
| 3rd | 0 |
| 4th | 3 (5.3%) |
| 5th | 8 (14%) |
| Clinical presentation | |
| Longitudinal melanonychia | 28 (49%) |
| Melanonychia of the entire nail apparatus | 5 (9%) |
| Nodular neoformation | 20 (35%) |
| Nail bed ulcer | 4 (7%) |
| Hutchinson's sign | 33 (57.9%) |
| Fold affected by Hutchinson's sign: | 12 (36%) |
| Proximal | 1 (3%) |
| Distal | 15 (46%) |
| Proximal + distal + left lateral | 5 (15%) |
| The entire nail apparatus | |
| Hyponychium involvement | |
| Nail dystrophy | 30 (52.6%) |
| Association | 15 (26.3%) |
| Nevo | 5 (8.8%) |
| Novo | |
| Trauma | |
| Histopathological features | |
| Histopathological subtype | 47 (82.5%) |
| Superficial spread | 5 (8.8%) |
| Nodular | 2 (3.5%) |
| Acral lentiginous | 11 (19.3%) |
| Desmoplastic | 39 (68.4%) |
| Unspecified | 1 (1.8%) |
| Breslow thickness (mm) | 4 (7%) |
| No. of mitoses/mm2 | 3 (0.5-5) |
| Ulceration | 2 (0.5-3) |
| Perineural invasion | 20 (35.1%) |
| Vascular invasion | 8 (14%) |
| Clark level | 7 (12.3%) |
| I | 26 (45.6%) |
| II | 7 (12.3%) |
| III | 7 (12.3%) |
| IV | 16 (28.1%) |
| V | 1 (1.8%) |
| Positive sentinel node | 16 (28.1%) |
| Tumor spread | |
| Local | |
| Regional | 41 (72%) |
| Distant | 11 (19%) |
| AJCC 8thEdition Classification | 5 (9%) |
| IA | 16 (28.1%) |
| IB | 5 (8.8%) |
| IIA | 9 (15.8%) |
| IIB | 6 (10.5%) |
| IIC | 7 (12.3%) |
| IIIC | 9 (15.8%) |
| IV | 5 (8.8%) |
| Follow-up period (months) | 60 (30-100) |
| Recurrence | 11 (19.3%) |
| Time of recurrence (months) | 18 (6-25) |
| Site of metastasis | |
| Lung | 4 (80%) |
| Central nervous system | 1 (20%) |
| Mortality | 5 (8.8%) |
| Results are expressed as frequencies (%). medians (q1-q3). | |
The most affected body segment was the lower limbs (n=30; 52.6%). However, the most affected region was the left hand (n=17; 29.8%), and overall, the most affected finger was the 1st one (n=43; 75.4%) (Fig. 1A-F).
Clinical features of subungual melanomas. A) Nail dystrophy with Hutchinson's sign affecting the proximal, left lateral, and distal fold of the right hallux. B) Amelanotic nodular growth on the right hallux. C) 1st finger of the right hand with Hutchinson's sign affecting the entire nail apparatus. D) Right hallux with Hutchinson's sign affecting the entire nail apparatus. E) Left hallux with nodular growth, Hutchinson's sign, and involvement of the proximal, left lateral, and distal fold. F) Longitudinal melanonychia on the right hand 1st finger.
Hutchinson's sign was present in 57.9% of the cases, and the hyponychium was compromised in 52.6% of the cases. Most were de novo melanomas (n=47; 82.5%) (Table 1).
The most common histological subtype was acral lentiginous (n=39; 68.4%). Eight out of 11 cases of nodular melanoma reported were amelanotic. The median Breslow thickness and mitosis was 3mm and 2 mitoses per field, respectively. Sentinel lymph node metastasis was confirmed in 16 patients (28.1%). Most patients had localized tumors (n=41; 72%) (Table 1).
According to the AJCC 2018 classification, the most common stage was IA (n=16; 28.1%). The median follow-up was 66 months, with a rate of recurrence of 19.3% and metastasis in 5 cases (9%) [4 (80%) in the lungs]. The mortality rate was 8.8% (Table 1).
Patients with Hutchinson's sign were more prone to having positive sentinel lymph nodes (P=.040). Patients with higher mortality rates were those with 1 recurrence (P=.045), high Breslow thickness (P=.045), positive sentinel lymph nodes (P=.001), and higher AJCC stages (P=.001). No significant differences were found between the clinical-histopathological characteristics and the affected segment (Appendix; Tables 2-4).
DiscussionThe incidence of SUM varies depending on the population, from 1% in Caucasians to 23% in Japanese.1–4 In our study, all patients were Mexican mestizos, with an incidence rate of 19%, which is higher than that reported by Mejbel et al. (19% vs 14%, respectively).5 Men are more commonly affected in most series, as the studies conducted by Chakera (61%),2 Mejbel (53%),5 and our own study demonstrated (61.4%), with a median age from 40 to 70 years. A past disease history of over 15 months has been reported. However, in our series, it was shorter (6 months).4,5 Clinically, the lower limbs are often the most affected ones (50% to 60%), mainly the 1st toe (50% to 70%).3–6 However, Chekera et al. reported a higher involvement of the left hand (53%).2 In our study, although the lower limbs were the most affected ones (52.6%), when results were split by region, the left hand revealed more cases of SUM (30%). Although de novo appearance is the most common one (as it was the case in our study), up to 28% of trauma-related cases of SUM have been reported.7–9 Hutchinson's sign has been reported in over 70% of all cases of SUM. However, in our study, it was found in less than 60% of the cases. All our cases had it on one nail only. We should mention that patients with Hutchinson's sign were more prone to having positive sentinel lymph nodes (P <.05).
The most widely reported subtype of SUM is acral lentiginous (57%), with a Breslow thickness median from 1mm to 4mm,3–5 which is similar to that from our study. Ulceration and vascular invasion tend to be more common in this type of melanoma, with incidence rates of 60% to 80% for each of these histopathological characteristics, according to different series.2–8 However, this observation is important since we could confirm lower rates (< 30%) in these variables in our cases. The perineural invasion reported by authors such as Mejbel (22%)5 was similar to the one reported in our study. It can be hypothesized that patients with SUM from the cited studies present with advanced stages of the disease. In our case, earlier stages of the disease were observed (AJCC IA).
The recurrence of SUM varies from 4% to 44%,5–9 which is similar to the results obtained from our study. The presence of distant metastasis was lower in our patients with SUM compared to what Mejbel,5 and Yoo8 reported (8.8% vs 44% and 29.5%, respectively). Also, our population had a lower mortality rate (9%), which differs from the data reported by Chakera et al. (30%).2
The limitations of this study include its retrospective nature, missing data such as melanonychia morphology features, the lack of a control group for comparison purposes, and the need for more statistical power.
In conclusion, this study is the first of its kind to specifically describe the characteristics of the Mexican mestizo population with subungual melanoma, which closely resemble those reported in the current scientific medical literature available. However, we could confirm that our patients presented with earlier stages of the disease, and lower rates of distant metastasis, and mortality. Additionally, Hutchinson's sign could be an early marker for the presence of positive sentinel lymph nodes.
Conflicts of interestNone declared.