The Pacman flap is a modified V-Y advancement flap that showed to be versatile in repairing surgical and non-surgical wounds. Indeed, this flap has been used in any anatomical localization, except for the scalp, where its use has not been reported. Moreover, the versatility of the Pacman flap can be enhanced by applying simple modifications to its original design.
Materials and methodsA case-series of 23 patients whose surgical breaches were repaired using standard or modified Pacman flap were included in this retrospective study.
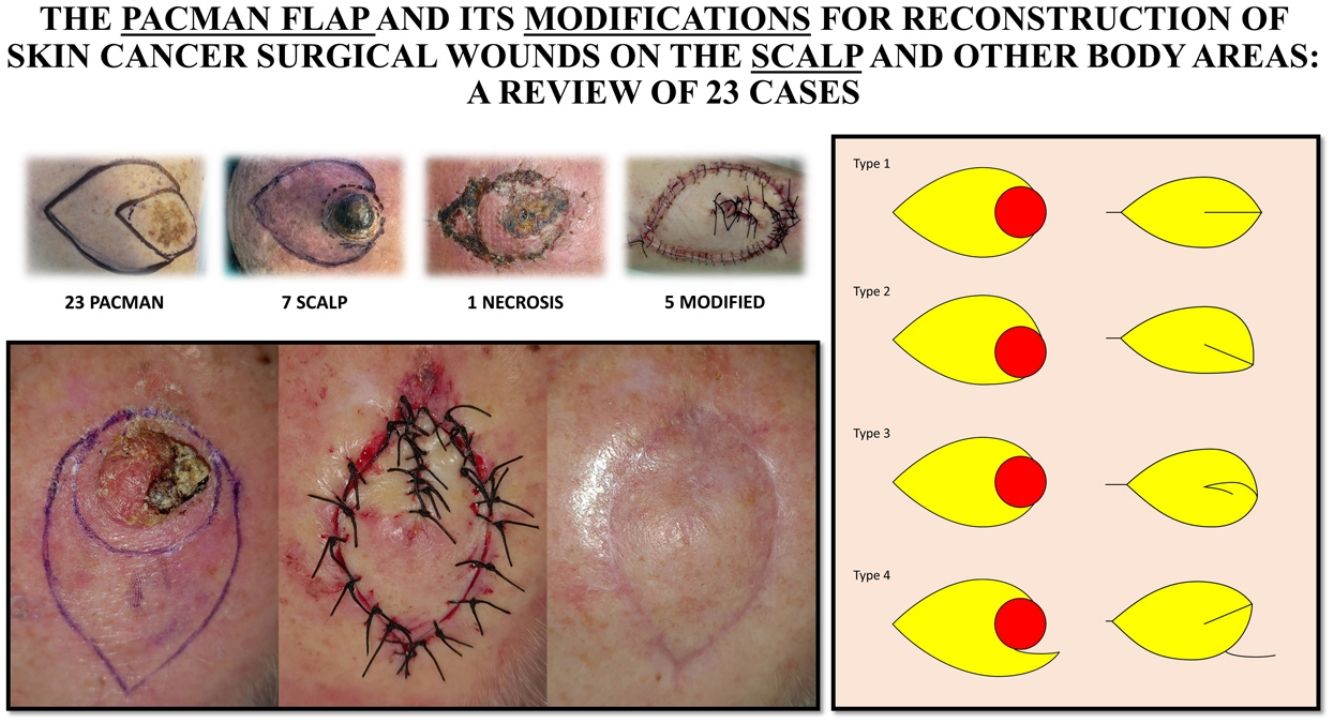
ResultsMost patients were male (65.2%) with a median age of 75.7 years. Squamous cell carcinoma was the tumor most commonly removed (60.9%), while scalp and face were the most frequent localizations (30.4%). Although 18 flaps were sculpted in the traditional Pacman shape, 5 were modified to fit the defect and localization. Complications occurred in 30% of flaps, but all of them were minor except for 1 extended necrosis.
ConclusionsThe Pacman flap can be used to repair surgical wounds localized in any body area, including the scalp. Three modifications can enhance the versatility of the flap and offer new repair options to dermatologic surgeons.
El colgajo Pacman es un colgajo de avance V-Y modificado, que resulta versátil para la reparación de las heridas quirúrgicas y no-quirúrgicas. De hecho, este colgajo ha sido utilizado en cualquier localización anatómica excepto en el cuero cabelludo, donde no se ha descrito su aplicación. Además, aplicando simples modificaciones al diseño original del colgajo Pacman se aumenta su versatilidad.
Material y métodosSe realizó un estudio retrospectivo con una serie de casos de 23 pacientes en los que se empleó el colgajo Pacman estándar o modificado en la reconstrucción de sus heridas quirúrgicas.
ResultadosLa mayoría de los pacientes fueron varones (65,2%) con una media de edad de 75,7 años. La mayoría de las extirpaciones fueron de carcinoma escamoso cutáneo (60,9%). Las localizaciones más frecuentes fueron el cuero cabelludo y la cara (30,4%). Aunque 18 colgajos se diseñaron siguiendo las directrices originales del colgajo Pacman, 5 fueron modificados para adaptarlo al defecto y la localización. El 30% de los colgajos desarrollaron complicaciones, todas ellas menores a excepción de un caso de necrosis extensa.
ConclusiónEl colgajo Pacman puede utilizarse para reparar defectos quirúrgicos en cualquier localización corporal, incluyendo el cuero cabelludo. Mediante 3 sencillas modificaciones puede mejorarse la versatilidad de este colgajo y ofrecer una nueva opción reconstructiva a los cirujanos dermatológicos.
The V-Y advancement flap is one of the flaps proposed to cover circular defects.1 This flap takes full advantage of the laxity of the surrounding tissue. However, the V-Y advancement flap requires the excision of exceeding healthy tissue to shape the flap and cover the roundish defect. Mithat et al. introduced a technique to close bedsores using bilateral flaps in order to better fit circular defects. The resulting shape of this modified V_Y advancement flap led the authors to name the flap as “Pacman” flap after the beloved character of the 90s arcade videogame.2,3 At the same time, Niranjan et al. published an identical flap (named “fishmouth” flap), as a unilateral and bilateral method to repair surgical breach on the lower limbs.4,5 After these descriptions, other authors have published their case series on the usefulness of the Pacman flap to repair various surgical and non-surgical soft-tissue wounds.6–13 To the best of our knowledge, none of these studies presented cases of scalp defects reconstruction.
The Pacman flap consists of two portions: (1) an advancing island flap, in which the universal muscle perforators provide the Pacman with robust vascularization; and (2) the Pacman “mouth”, composed by two flaps that rotate to close the jaws. This double movement leads to a redistribution of the tension forces in different vectors. Moreover, if compared to the traditional V-Y advancement flap the Pacman provides similar coverage but requires less advancement, resulting in reduced tension, and sacrificing less healthy tissue (Supplementary material – Fig. 1). The biogeometry of the Pacman flap has been described previously13 and is also depicted (Supplementary material Fig. 2.)
In this study, we review the Pacman flap using a series of cases where this flap was applied for soft tissue reconstruction after skin cancer resection in different areas of the body, including the scalp. Furthermore, we analyze the technical features that must be considered to obtain optimal results, and we present 3 modifications of the flap that may offer new repair options to dermatologic surgeons.
Materials and methodsWe performed an observational retrospective study including patients with skin cancer surgical breaches reconstructed using the Pacman flap between 2019 and 2021 at the centers involved. Each tumor was removed by using standard surgical margins depending on the risk category. Specimens were sent for standard histological analysis using formalin-fixed paraffin-embedded sections. Margins clearance was confirmed histologically for all tumors, and none required re-intervention.
For each patient, we collected the following variables: gender, age at the time of surgery, histological type of the excised skin tumor, size of the defect, type of Pacman flap used (Fig. 1) and post-operative complications. Size of the defect was calculated approximating the area to that of an ellipse: A=π×a×b (being a and b the major and minor semiaxis, respectively).
Continuous variables were presented as mean and standard deviation if they followed a normal distribution at Kolmogorov–Smirnov test. Median and interquartile range were used otherwise. Qualitative variables were presented as absolute value and percentage.
Results23 Pacman flaps from the same number of patients were included in the study. Fifteen out of 23 patients (65.2%) were male and the median age at time of surgery was of 75.7 years (interquartile range: 72–83.5). The excised tumors included fourteen squamous cell carcinoma (SCC) (60.9%), 7 basal cell carcinoma (BCC) (30.5%), 1 lentigo maligna (4.3%) and 1 from dermatofibrosarcoma protuberans (4.3%). The scalp and the face were the most frequent localizations (7/23, 30.4%; 7/23, 30.4%); followed by the leg (5/23, 21.7%); the shoulder (2/23, 8.7%), the axilla (1/23, 4.3%) and the hand (1/23, 4.3%). Surgical breach size ranged from 5.6cm2 to 15.9cm2 with a median of 12.6cm2.
Eighteen flaps (78.3%) were performed with the traditional technique (type 1) and the remaining 5 (21.7%) were modified: 2 by drawing an asymmetric mouth (type 2), 2 by transposing one of the two jaws (type 4) and 1 by bending it in a logarithmic fashion (type 3). Out of 7 flaps that developed post-operative complications (30.4%), 4 were performed on the leg. Results are summarized in Table 1.
Characteristics of the Pacman flap cases reviewed.
| Case | Gender | Age | Histotype | Site | Defect size (cm2) | Pacman type | Complications |
|---|---|---|---|---|---|---|---|
| 1 | F | 88 | BCC | Leg | 13.7 | 2 | Tip venous congestion |
| 2 | M | 85 | SCC | Scalp | 6.6 | 1 | None |
| 3 | M | 91 | KA | Scalp | 14.1 | 1 | None |
| 4 | M | 73 | KA | Scalp | 6.5 | 1 | Flap necrosis |
| 5 | M | 69 | BCC | Leg | 12.2 | 3 | Tip epidermal necrosis |
| 6 | M | 84 | SCC | Cheek | 11.0 | 2 | None |
| 7 | M | 70 | LM | Shoulder | 28.3 | 1 | None |
| 8 | M | 68 | BCC | Scalp | 12.6 | 1 | None |
| 9 | F | 82 | SCC | Leg | 5.9 | 1 | Tip venous congestion |
| 10 | F | 68 | BCC | Eyebrow | 5.9 | 1 | None |
| 11 | F | 71 | KA | Upper eyelid | 4.9 | 4 | None |
| 12 | M | 77 | SCC | Leg | 5.3 | 1 | Tip epidermal necrosis |
| 13 | F | 81 | SCC | Leg | 3.1 | 1 | None |
| 14 | F | 76 | BCC | Upper eyelid | 2.8 | 4 | None |
| 15 | M | 78 | SCC | Scalp | 23.8 | 1 | None |
| 16 | F | 89 | SCC | Hand | 14.1 | 1 | None |
| 17 | M | 79 | SCC | Cheek | 11.0 | 1 | None |
| 18 | M | 83 | SCC | Axilla | 21.6 | 1 | Tip epidermal necrosis |
| 19 | F | 5 | DFSP | Shoulder | 38.5 | 1 | None |
| 20 | M | 77 | SCC | Scalp | 17.7 | 1 | None |
| 21 | M | 91 | BCC | Lower eyelid | 2.4 | 1+vein graft | Flap retraction |
| 22 | M | 74 | BCC | Eyebrow | 3.1 | 1 | None |
| 23 | M | 81 | SCC | Scalp | 23.6 | 1 | None |
F=female; M=male; BCC=basal cell carcinoma; SCC=squamous cell carcinoma; KA=keratoacanthoma; LM=lentigo maligna; DFSP=dermatofibrosarcoma protuberans.
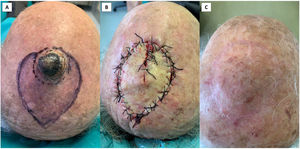
The Pacman flap was originally proposed for repairing surgical wounds located on the lower limb and bedsores. Plasticity of the Pacman flap makes it also useful in repairing large defects on the trunk ad upper extremities, both on concave and convex areas. Moreover, it can be used to cover facial defects, especially if localized on the cheek and lateral forehead/temple region.12 Finally, this flap can be applied to repair scalp defects, where the skin is usually kept firm by the inelastic nature of the galea capitis below and flaps motion is limited. To the best of our knowledge, use of the Pacman flap on the scalp has not been previously reported. In this series we presented 7 cases of Pacman flap used to repair scalp defects. Indeed, scalp resulted the most frequent localization where this flap was applied along with the face. As mentioned above, the Pacman moves tissue from and distributes tension to the skin all around its perimeter. This permits good flap survivability and mobility, even when the surgeon is repairing scalp defects (Figs. 3 and 4). However, there are not perforating vessels that connect the periosteum to the galea above (the subgaleal plane contains loose areolar tissue and is relatively avascular). Thus, flap vascularization depends on the vessels that run through the subcutis and in close proximity to the galea/fascia. Previous papers have shown the utility of V-Y advancement island pedicle flap based on named arteries (e.g., superficial temporal artery) or, more randomly, on the fascia that contains them for repairing scalp surgical wounds.14,15 The Pacman flap on the scalp follows the same technical principles. Therefore, it is important to incise some areas of the Pacman perimeter up to the subcutis just below the dermis and not up to the subgaleal plane, as it is usually recommended in repairing scalp defects (Supplementary material – Fig. 3). This is to guarantee more vascular supply at the expense of mobility. In fact, incising all the perimeter up to the subgaleal plane may lead to flap necrosis (Supplementary material – Fig. 4). The areas where the subcutis and the galea are not incised become the flap's pedicles(s). Once the Pacman flap is incised, its mobility can be enhanced by undermining the flap and surrounding tissue in the subgaleal plane. At the pedicles(s) undermining should be performed in a dual plane: below the pedicle in the subgaleal (or in the even safer subperiosteal plane), and above the pedicle in the upper subcutis (Supplementary material – Fig. 3). If further mobility is required, galeotomy can be performed in the surrounding tissue, but it must be done very carefully below the pedicle to avoid damaging the vessels running in close proximity to the galea. A doppler probe can be used preoperatively to trace the course of named arteries and preserve them.
Thirty percent of the flaps developed complications, all minor except 1 extended necrosis. If we only consider the complications of the flap distal portion, we observed 5 venous congestions/epidermal necrosis (21.7%); the same percentage recently reported by Zhang et al.12 In our series, 5 Pacman flaps were used to repair defects localized on the leg and 4 of them developed minor complications of the flap tip that resolved spontaneously with no esthetic or functional sequelae. All these flaps were based on random vascularization. Thus, we would highlight the importance of sculpting accurately the flap, especially in the case of leg or scalp localization. In fact, given that most of the cases showing complications were located on the leg, it could be suggested that when facing Pacman flaps on the lower limbs, the surgeon should opt to perform a perforator-based approach, as described by Niranjan et al.5
When the Pacman mouth is closed, a standing cone is generally formed independently of the localization. This dog's ear deformity can be removed or not, depending on its bulk and on flap perfusion. Indeed, when correcting the deformity, it is mandatory to not remove subcutaneous tissue unless risking to compromise flap vascularization. However, the exceeding tissue gradually settles down with time and thus it often does not require correction. This dog's ear represents the only healthy exceeding tissue that may be sacrificed.
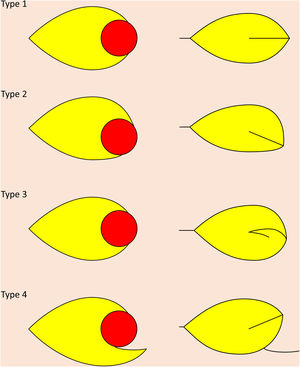
Modifications of the Pacman flapThe standard Pacman flap (type 1) can be easily modified to enhance its capability to repair a wide range of surgical wounds in different localizations (Fig. 1), including the scalp (Figs. 3 and 4).
Type 2 Pacman flap for repairing a leg surgical wound after basal cell carcinoma removal. (A) Being the surgical breach localized on the pretibial region, this Pacman was drawn with an asymmetric mouth: the upper jaw of the flap, next to the tibia, was drawn smaller than the lower jaw. This to recruit more tissue where it was more easily mobilized. (B) The flap was undermined above the superficial fascia, moved, and sutured; a dog's ear deformity was removed at the conjunction of the two rotating jaws. (C) Venous congestion of the tip was present when stiches were removed after 2 weeks. (D) At 1 year the functional and esthetic result was very good with only faint hyperpigmentation of the most distal portion of the flap where venous congestion developed.
Type 1 Pacman flap for repairing a scalp squamous cell carcinoma removal. (A) Tumor excision with 6mm margins and flap design with a symmetric mouth. (B) Flap undermined in the subcutaneous tissue, except for the jaws and the tail of the flap (undermined up the periosteum), and sutured in place. (C) Good esthetic result at 3 months.
Type 1 Pacman flap for repairing a scalp keratoacanthoma removal. (A) Tumor excision with 5mm margins and flap design with a symmetric mouth. (B) Flap sutured after undermining up to the subcutis or into the subcutis. This reduced flap mobility, as demonstrated by the gap of the closing mouth, but it guaranteed sufficient flap perfusion. (C) Post-operative result at 1 year showed an optimal reconstruction.
The first modification (Pacman type 2) is realizing the flap with an asymmetric mouth if surrounding skin mobility is not uniform around the defect (Fig. 2).
The second modification (Pacman type 3) is used when the flap mouth does not close due to scarce tissue mobility or ill-design of the flap. This modification can be called logarithmic Pacman (Fig. 5).
Type 3 Pacman flap for repairing a leg basal cell carcinoma removal. (A) Pacman flap drawn with asymmetrical mouth and tumor extirpation with 4mm margins. (B) The flap and surrounding skin motion were not sufficient to cover entirely the defect width, while they were more than enough to cover its length. Thus, the lower jaw of the flap mouth was rotated on itself in a logarithmic fashion. This permitted to repair completely the surgical wound. (C) The flap suffered epidermal necrosis of the tip, but it did not require further procedures or specific dressings. (D) At 4 months the result achieved was good with great patient satisfaction.
The third modification (Pacman type 4) is applied when the local anatomy requires that one (or both) mouth portions moves as a transposition flap instead of an advancement/rotation flap. This third modification has been already published under the name of crab claw island pedicle flap (CCIPF).16 Indeed, we proposed the CCIPF as a modification of the well-known shark island pedicle flap,17 but when applied outside of the alar-perialar-upper lip area CCIPF shape and movement correspond to those of a Pacman flap where one jaw transposes instead of advancing/rotating (Case 11 of this series).16 For this similarity (in the end both these flaps are modifications of the traditional V-Y advancement flap), we suggest that CCIPF should be also classified in flaps taxonomy as a modification of the Pacman flap.
ConclusionIn this study we reviewed the features of the Pacman flap proposing its application for scalp surgical wounds and illustrating 3 modifications of it. Our study showed that the Pacman flap is a versatile flap that allows to repair a wide array of skin cancer surgical wounds, included those localized on the scalp. Traditionally proposed to cover lower limbs surgical breaches and bedsores, this flap is useful in closing soft-tissue defects localized in any body area, especially if adapted and modified to fit each localization. The Pacman flap is thus a very interesting repair option that should be included in the daily armamentarium of the dermatologic surgeon.
Conflict of interestsThe author(s) declare(s) that there is no conflict of interest.