Hidradenitis suppurativa (HS) is a chronic skin disease whose impact on skin homeostasis has not been adequately studied at present. Knowledge about how skin function changes in these patients, and could be of interest not only to improve the topical management of the disease, but also as an objective measure of disease activity. The aim of this study was to compare skin homeostasis and the epidermal barrier function in lesional and healthy skin areas of patients with HS.
MethodsWe conducted a cross-sectional study. Skin homeostasis and the epidermal barrier function of lesions were assessed in HS patients using validated tools. A healthy perilesional skin control was assigned to each lesion to compare skin homeostasis parameters.
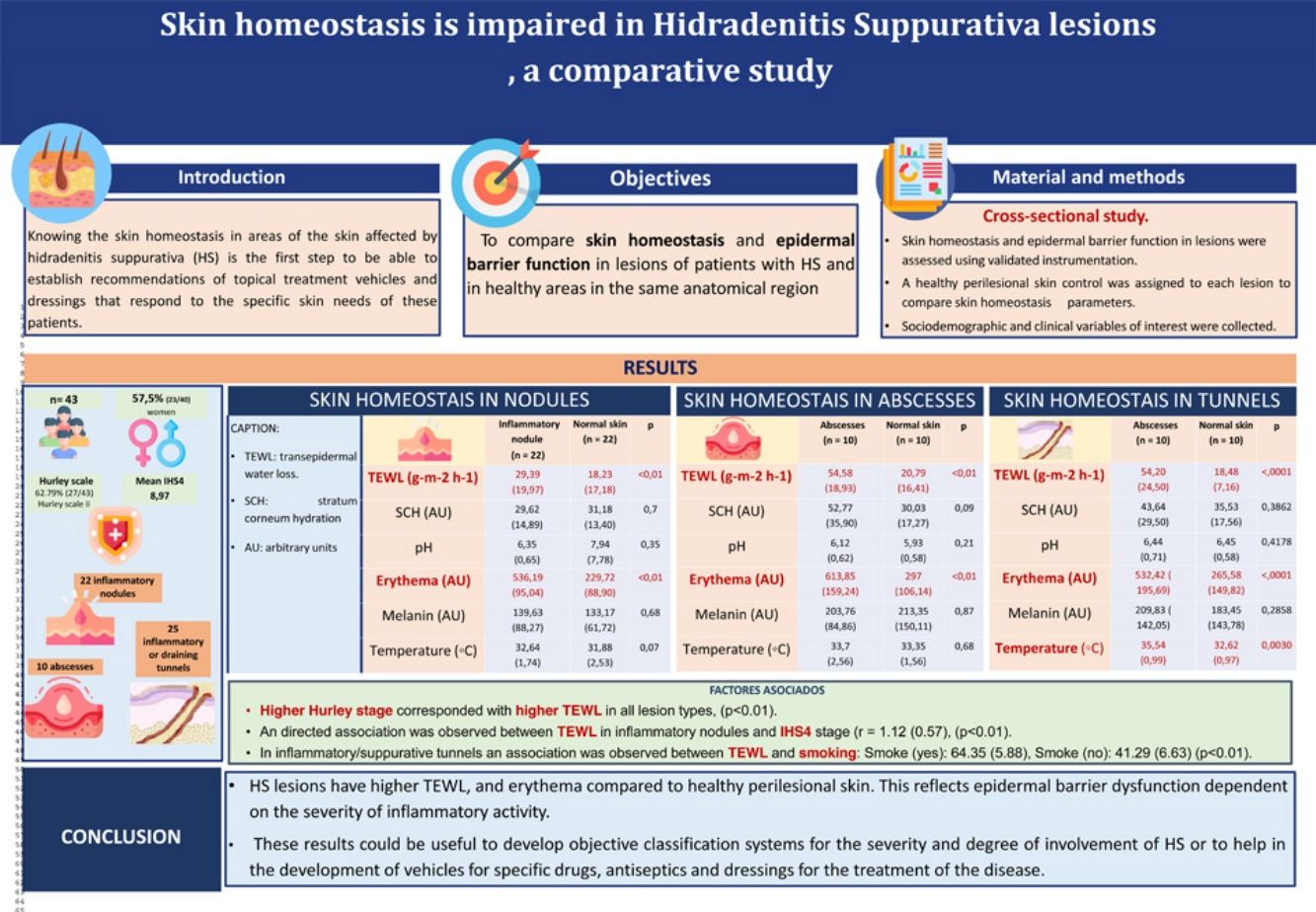
ResultsA total of 43 patients were included: 22 nodules, 10 abscesses and 25 draining tunnels were measured. The male-to-female ratio was 20:23, and the mean age, 35.95 years (SD, 14.82). Increased transepidermal water loss (TEWL) and erythema were found in nodules, abscesses and draining tunnel vs healthy skin. A direct association was observed between inflammatory nodules TEWL and IHS4 stage. In draining tunnels, a direct association was observed between TEWL and smoking. A trend of increasing TEWL values was observed as a function of Hurley stage.
ConclusionHS lesions exhibit epidermal barrier dysfunction that depends on the severity of inflammatory activity. These results could be useful to develop objective classification systems for the severity and degree of involvement of HS or help in the development of vehicles for specific drugs, antiseptics and dressings for the management of this disease.
La hidradenitis supurativa (HS) es una enfermedad crónica de la piel cuyo impacto sobre la homeostasis cutánea no ha sido adecuadamente estudiado en la actualidad. El conocimiento de cómo se modifica la función cutánea en estos pacientes podría ser de interés para mejorar el manejo tópico de la enfermedad y como medidas objetivas de la actividad de la misma. El objetivo de este estudio fue comparar la homeostasis cutánea y la función de barrera epidérmica en zonas de piel lesional y sana de pacientes con HS.
MétodosSe realizó un estudio transversal. Se evaluaron la homeostasis cutánea y la función de barrera epidérmica en las lesiones de pacientes con HS mediante instrumentación validada. Se asignó un control de piel sana perilesional a cada lesión para comparar los parámetros de homeostasis cutánea.
ResultadosSe incluyeron 43 pacientes: se midieron 22 nódulos, 10 abscesos y 25 túneles de drenaje. La proporción hombre:mujer fue de 20:23, la edad media fue de 35,95 (desviación estándar [DE] 14,82) años. Se observó un aumento de la pérdida transepidérmica de agua (TEWL) y eritema en los nódulos, abscesos y túneles de drenaje en comparación con la piel sana. Se observó una asociación directa entre la TEWL de los nódulos inflamatorios y el estadio del International Hidradenitis Suppurativa Severity Scoring System (IHS4). En los túneles de drenaje, se observó una asociación directa entre la TEWL y el tabaquismo. Se halló una tendencia al aumento de los valores de TEWL en función del estadio de Hurley.
ConclusionesLas lesiones de HS presentan disfunción de la barrera epidérmica dependiente de la gravedad de la actividad inflamatoria. Estos resultados podrían ser útiles para desarrollar sistemas de clasificación objetivos de la gravedad y el grado de afectación de la HS o para contribuir al desarrollo de vehículos para fármacos, antisépticos y apósitos específicos para el tratamiento de la enfermedad.
Hidradenitis suppurativa (HS) is a chronic and progressive inflammatory disease characterized by the appearance of nodules, abscesses, and sinusoidal tracts in the inguinal, axillary, sub-mammary and anogenital areas1,2 which can impact the patient's quality of life significantly3 and be associated with several comorbidities.4 The pathogenesis of the disease is related to follicular hyperkeratosis and subsequent inflammation.
Some cytokines play a key role in the pathogenesis of the disease, including IL-1β, IL-17 and TNF-α.5 Obesity, smoking, and hormonal disturbances are other predisposing factors that can impact the development and progression of the disease.6,7
The management of these patients in all stages of severity usually includes topical treatment such as solutions, gels, ointments, creams, etc., or systemic treatment.8,9 Due to the anatomical areas where the lesions are located, it is a common thing to cover them with dressings, patches or gauzes. Knowing the homeostasis of the skin in skin regions touched by HS is the first step to establish recommendations or plan the design of topical treatment vehicles and dressings that respond to these patients’ specific skin needs, since specific bandages for HS10 are not currently available.
The epidermal barrier is important to protect the human body from many external stressors and maintain skin homeostasis.11 Several methods have been described for assessing skin homeostasis and the epidermal barrier function, such as transepidermal water loss (TEWL), stratum corneum hydration (SCH), surface pH, temperature, elasticity, and erythema.12
The aim of this study was to compare skin lesions of HS and same healthy skin in terms of cutaneous homeostasis and epidermal barrier function in patients with HS to gain knowledge and understanding which could be used to assess specific ways to improve topical care of HS skin lesions.
MethodsStudy design: We conducted a cross-sectional study to evaluate differences in homeostasis and the epidermal barrier function between HS skin lesions and perilesional healthy skin in patients with HS. Participants were recruited from the Dermatology Unit of Hospital Universitario Virgen de las Nieves, Granada, Spain.
Inclusion criteria: Patients older than 18 years of age with a clinical diagnosis of HS who had any kind of active lesion such as nodules, abscesses or draining tunnels with inflammation/suppuration were included in the study.
Exclusion criteria: Patients with HS without active lesions, or those who did not gave their prior written informed consent were excluded from the study.
Study variablesMain variables of interestHomeostasis parameters and epidermal barrier function variables were recorded using a multiprobe adapter. All measurements were taken in the same room at a temperature of 23±1°C and an ambient air humidity of 45% (range, 40–50%). Recorded variables were:
- a)
Skin temperature (in °C, using Skin-Thermometer® ST 500)
- b)
TEWL (in gm2h−1 using Tewameter®™ 300
- c)
Erythema and melanin index (in arbitrary units (AU), using Mexameter® MX 18)
- d)
SCH (in arbitrary units (AU), using Corneometer® CM825)
- e)
pH (using Skin-pH-Meter® 905)
These variables were measured in 2 areas of patients with HS (in an inflammatory/suppurative nodule, abscess, or fistula and in completely healthy skin located 5cm away from the edge of the lesion). A maximum of 1 lesion of each type (nodule, abscess or fistula) was evaluated in each patient.
Other variables of interestThe severity of the disease was determined using Hurley Stage,9 the refined Hurley classification (Hurley-R),11 and the International Hidradenitis Suppurativa Severity Score System (IHS4 (referencia)), which were collected at that time in the office.
Other socio-demographic and clinical data were obtained, such as age, sex, age of onset, comorbidities, family history, previous and current treatments and previous surgical procedures, disease phenotype and number of affected regions. In addition, patients were questioned about certain habits of interest, such as tobacco consumption, type of deodorant routine, whether the lesion was previously covered or not, products used for the hygiene of the area and previous topical treatment of the lesion, etc.
Statistical analysisContinuous variables were expressed as mean standard deviations (SD). Qualitative variables were expressed as absolute and relative frequency distributions. To compare continuous variables, the Student t-test for independent samples or the Student t-test for paired samples were used, as appropriate. Pearson's correlation coefficient was calculated to check for possible correlations between continuous variables. Statistical significance was defined using a two-tailed p value<0.05. SPSS version 24.0 (SPSS Inc., Chicago, IL, United States) was used.
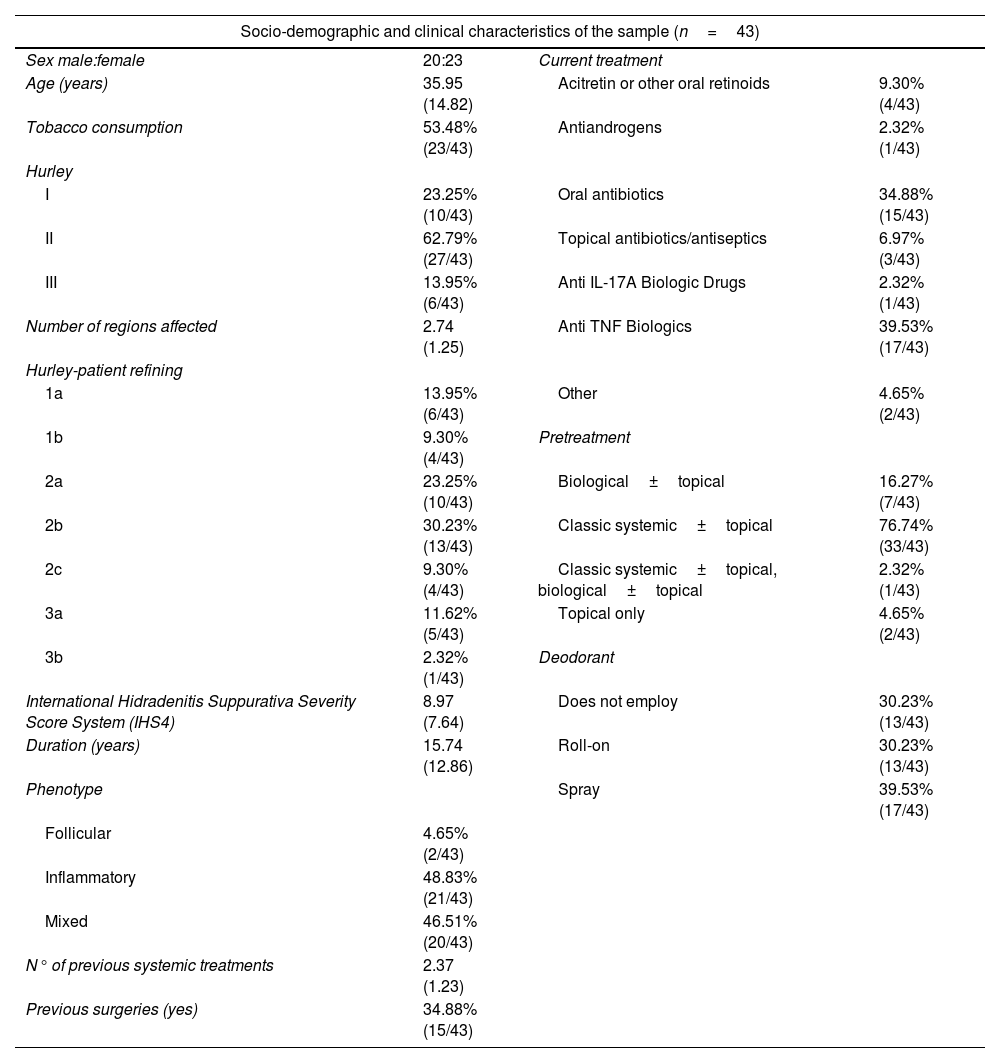
ResultsCharacteristics of the sampleA total of 43 patients with HS (20 men and 23 women) were included. Mean age was 35.9 years (SD, 14.8). The most frequent Hurley stage was Stage II (62.7%, 27/43) and the mean value for IHS4 was 8.9 (SD, 7.6). Most common phenotypes were inflammatory (48.83%, 21/43), and mixed (46.51% – 20/43). Other sociodemographic and clinical characteristics are described in Table 1.
Overview of socio-demographic and clinical characteristics of the sample.
| Socio-demographic and clinical characteristics of the sample (n=43) | |||
|---|---|---|---|
| Sex male:female | 20:23 | Current treatment | |
| Age (years) | 35.95 (14.82) | Acitretin or other oral retinoids | 9.30% (4/43) |
| Tobacco consumption | 53.48% (23/43) | Antiandrogens | 2.32% (1/43) |
| Hurley | |||
| I | 23.25% (10/43) | Oral antibiotics | 34.88% (15/43) |
| II | 62.79% (27/43) | Topical antibiotics/antiseptics | 6.97% (3/43) |
| III | 13.95% (6/43) | Anti IL-17A Biologic Drugs | 2.32% (1/43) |
| Number of regions affected | 2.74 (1.25) | Anti TNF Biologics | 39.53% (17/43) |
| Hurley-patient refining | |||
| 1a | 13.95% (6/43) | Other | 4.65% (2/43) |
| 1b | 9.30% (4/43) | Pretreatment | |
| 2a | 23.25% (10/43) | Biological±topical | 16.27% (7/43) |
| 2b | 30.23% (13/43) | Classic systemic±topical | 76.74% (33/43) |
| 2c | 9.30% (4/43) | Classic systemic±topical, biological±topical | 2.32% (1/43) |
| 3a | 11.62% (5/43) | Topical only | 4.65% (2/43) |
| 3b | 2.32% (1/43) | Deodorant | |
| International Hidradenitis Suppurativa Severity Score System (IHS4) | 8.97 (7.64) | Does not employ | 30.23% (13/43) |
| Duration (years) | 15.74 (12.86) | Roll-on | 30.23% (13/43) |
| Phenotype | Spray | 39.53% (17/43) | |
| Follicular | 4.65% (2/43) | ||
| Inflammatory | 48.83% (21/43) | ||
| Mixed | 46.51% (20/43) | ||
| N° of previous systemic treatments | 2.37 (1.23) | ||
| Previous surgeries (yes) | 34.88% (15/43) | ||
In terms of current treatment, most patients were on oral antibiotics or anti-TNF biologic drugs. Finally, deodorant was used in most patients in spray (39.53%, 17/43) or roll-on formats (30.23%, 13/43).
Cutaneous homeostasis parameters in lesional and healthy skinHomeostasis was explored in different HS skin lesions, including inflammatory nodules, abscesses and draining tunnels:
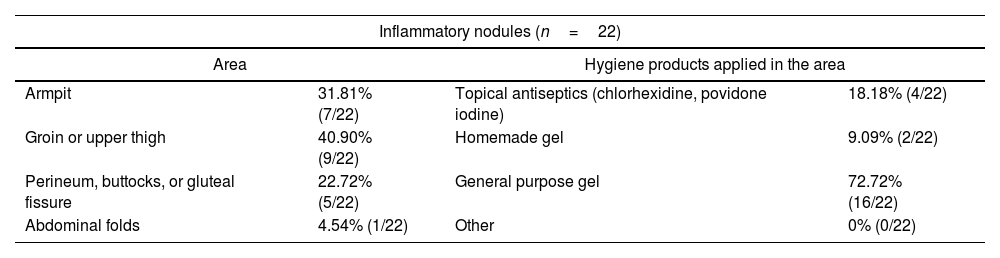
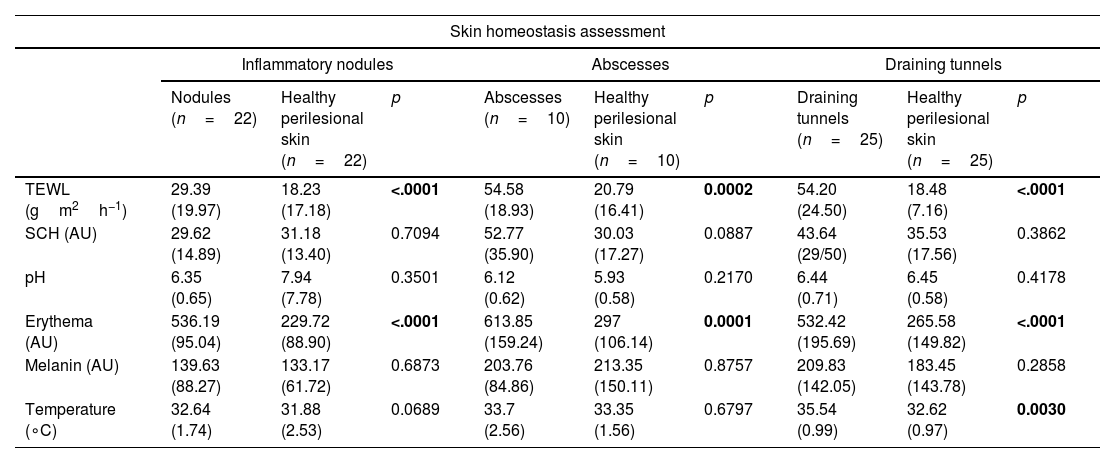
Inflammatory nodules: The most common characteristics of inflammatory nodules included the most frequent location on the groin or upper thigh. For the most part, these lesions were not covered, and patients used general-purpose gel for personal hygiene (Table 2). The comparison of the parameters of the epidermal barrier function between inflammatory nodules and healthy perilesional skin can be seen in Table 3. Of note that TEWL and erythema were significantly higher (p<0.001) in the inflammatory nodule vs perilesional healthy skin. Temperature was higher in inflammatory nodules vs healthy skin, with trends toward significance (p=0.06). Nonsignificant differences were found in SCH, pH, and melanin.
Table 2.Characteristics of each type of HS skin lesions.
Inflammatory nodules (n=22) Area Hygiene products applied in the area Armpit 31.81% (7/22) Topical antiseptics (chlorhexidine, povidone iodine) 18.18% (4/22) Groin or upper thigh 40.90% (9/22) Homemade gel 9.09% (2/22) Perineum, buttocks, or gluteal fissure 22.72% (5/22) General purpose gel 72.72% (16/22) Abdominal folds 4.54% (1/22) Other 0% (0/22) Abscesses (n=10) Area Hygiene products applied in the area Nape of the neck 20.00% (2/10) Topical antiseptics (chlorhexidine, povidone iodine) 30.00% (3/10) Groin or upper thigh 10.00% (1/10) General purpose shampoo 10.00% (1/10) Perineum, buttocks, or gluteal fissure 40.00% (4/10) General purpose gel 60.00% (6/10) Abdominal folds 20.00% (2/10) Degree of suppuration Other location 10.00% (1/10) Suppurative lesions 70.00% (7/10) Draining tunnels (n=25) Area Hygiene products in the area Armpit 52.0% (13/25) Topical antiseptics (chlorhexidine, povidone iodine) 8.0% (2/25) Groin or upper thigh 36.0% (9/25) Homemade gel 4.0% (1/25) Breast or inframammary regions 4.0% (1/25) General purpose gel 84.0% (21/25) Perineum, buttocks, or gluteal fissure 4.0% (1/25) Degree of suppuration Other location 4.0% (1/25) Suppurative 44.0% (11/25) Table 3.Assessment of skin homeostasis in lesioned and healthy areas, including inflammatory nodules, abscessess and draining tunnels.
Skin homeostasis assessment Inflammatory nodules Abscesses Draining tunnels Nodules (n=22) Healthy perilesional skin (n=22) p Abscesses (n=10) Healthy perilesional skin (n=10) p Draining tunnels (n=25) Healthy perilesional skin (n=25) p TEWL (gm2h−1) 29.39 (19.97) 18.23 (17.18) <.0001 54.58 (18.93) 20.79 (16.41) 0.0002 54.20 (24.50) 18.48 (7.16) <.0001 SCH (AU) 29.62 (14.89) 31.18 (13.40) 0.7094 52.77 (35.90) 30.03 (17.27) 0.0887 43.64 (29/50) 35.53 (17.56) 0.3862 pH 6.35 (0.65) 7.94 (7.78) 0.3501 6.12 (0.62) 5.93 (0.58) 0.2170 6.44 (0.71) 6.45 (0.58) 0.4178 Erythema (AU) 536.19 (95.04) 229.72 (88.90) <.0001 613.85 (159.24) 297 (106.14) 0.0001 532.42 (195.69) 265.58 (149.82) <.0001 Melanin (AU) 139.63 (88.27) 133.17 (61.72) 0.6873 203.76 (84.86) 213.35 (150.11) 0.8757 209.83 (142.05) 183.45 (143.78) 0.2858 Temperature (∘C) 32.64 (1.74) 31.88 (2.53) 0.0689 33.7 (2.56) 33.35 (1.56) 0.6797 35.54 (0.99) 32.62 (0.97) 0.0030 AU: arbitrary units; SCH, hydration of the stratum corneum; TEWL, transepidermal water loss.
Bold values mean “significant differences found”.
Abscesses: The most frequent location of abscesses was the perineum, buttocks or gluteal fissure. These lesions were mostly not covered, suppurated under pressure, and patients used general-purpose gel for cleaning these areas (Table 2). The comparison of skin homeostasis between abscesses and healthy perilesional skin can be seen in Table 3. TEWL and erythema were significantly higher (p<0.001) in abscesses vs perilesional healthy skin. No statistically significant differences were found in SCH, pH, melanin, or temperature.
Suppurative draining tunnels: Draining tunnels were most frequently located at the armpit. Most of these lesions were not covered, did not have suppuration, and patients used general-purpose gel for personal hygiene (Table 2). The comparison of skin homeostasis between suppurative draining tunnels and healthy perilesional skin can be seen in Table 3. TEWL and erythema were significantly higher (p<0.001), as well as temperature (p=0.003) in suppurative draining tunnels vs perilesional healthy skin. No statistically significant differences were found in SCH, pH, or melanin.
Clinical factors potentially related to changes in TEWL were explored. First, TEWL was higher in patients with higher Hurley stage for all skin lesions (p<0.01). Moreover, a positive correlation was found between TEWL in inflammatory nodules and IHS4 stage (β=1.12 (SD, 0.57), p=0.006). Finally, in inflamed/suppurative fistulas, an association between TEWL and tobacco use was reported (p=0.016).
DiscussionSkin integrity is crucial to maintain a correct skin barrier function to prevent TEWL and the penetration of pathogens from the external environment. In this study, the state of the epidermal barrier was analyzed by measuring cutaneous homeostasis parameters in patients with HS. The barrier function has been found to be impaired in the skin lesions of HS patients, which is reflected in increased TEWL and erythema in all 3 types of HS lesions: nodules, abscesses, and fistulas.
Skin barrier dysfunction has also been described in other inflammatory skin diseases such as psoriasis13 and atopic dermatitis (AD).14 For example, psoriatic plaques show decreased as well as higher temperatures, TEWL, and erythema.13 In patients with AD, an increased temperature, TEWL and less SCH in eczematous lesions has been reported .15 In addition, dysfunction of the epidermal barrier is also observed in the “healthy” skin of patients with psoriasis and AD, reflected in higher levels of TEWL in the healthy skin of these patients when vs the skin of healthy controls.16
Regarding HS, a recent meta-analysis confirmed that the pathogenic triad of HS consists of upregulated inflammation, changes of epithelial differentiation, and dysregulation of metabolic signaling.17 Among the genes involved in skin regulation, it has been found that the inflammatory process of HS is associated with the upregulation of PI3 and SERPIN, both associated with skin homeostasis and chronic skin inflammation.18
However, a recent study comparing TEWL between HS lesions and healthy skin found no statistically significant differences.19 In this study, researchers did not distinguish between the different types of skin lesions. Also, the location where TEWL measurements were taken was not reported. In contrast, the present study shows the presence of a dysfunctional epidermal barrier in HS lesions that is shown by higher levels of TEWL vs healthy perilesional skin.
The present study has identified a positive association between smoking and increased epidermal barrier dysfunction in HS lesions. This finding has biological plausibility, as smoking acts as an exogenous factor in the pathogenesis of hidradenitis suppurativa, promoting inflammation and exacerbating the clinical signs.1
On the other hand, erythema and temperature are higher in HS lesioned areas vs healthy perilesional skin. Both parameters are related to inflammation, as part of the pathophysiological process of HS. The chemotactic inflammatory response by neutrophils and lymphocytes leads to the development of nodules, abscesses, and the subsequent destruction of the pilosebaceous unit.1
Finally, as in other diseases such as AD and psoriasis, an association has been observed between disease severity and barrier dysfunction for HS patients. In AD and psoriasis, higher TEWL and temperature values are associated with more severe disease, which helps identify patients who would benefit from intensive treatment.16 In HS, higher levels of TEWL seem to correlate with higher Hurley stage in all types of skin lesions. Therefore, TEWL could be a marker of those patients with greatest disease severity. This objective parameter could help us identify the greatest severity of HS and help us develop reproducible and accurate scales and classification systems. On the other hand, studies with larger sample sizes could provide findings with therapeutic implications (for example, greater erythema could lead to the use of topical corticosteroids and higher TEWL lead to the use of topical astringents). Potential therapeutic implications or choice of hygiene products are difficult to predict, given the absence of differences by type of treatment or type of deodorant used in our study. However, these findings are merely exploratory considering the small sample size.
The lack of differencesThis study has been limited by the difficulty of measuring with probes, as they require a smooth surface to perform an optimal measurement. Moreover, the presence of suppuration could have altered some values such as SCH.
In conclusion, HS skin lesions show higher TEWL vs healthy perilesional skin, which reflects a dysfunctional epidermal barrier whose severity seems to be related to general disease severity. These results could be useful to develop an objective classification of disease severity, or help develop vehicles for drugs, antiseptics, and specific dressings for the management of the disease.
EthicsThe present study was approved by the Research Ethics Committee of “Hospital Universitario Virgen de las Nieves” and is in accordance with the Declaration of Helsinki.
Conflicts of interestThe authors have no conflicts of interest to declare.