An 82-year-old man was admitted to our Dermatology Department for necrotic skin lesions on the limbs with a 4-month evolution. He was diagnosed a coronary disease by coronary angiography made six months earlier. He had also hypertension, hypercholesterolemia, and was anticoagulated with warfarin for atrial fibrillation.
The physical examination revealed purpuric papules and plaques with a necrotic center in the upper and lower limbs, including fingers and toes (Fig. 1). Erosions of the nasal mucosa were also observed.
Laboratory testing was unremarkable, including autoimmunity (tests for antinuclear and anti-neutrophil cytoplasm antibodies were negative), viral serologies (HIV, HBV, HCV), serum protein electrophoresis, and cryoglobulins.
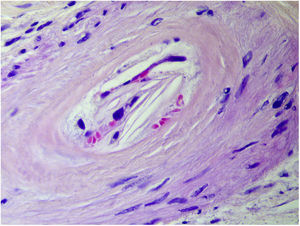
Skin biopsy showed biconvex, needle-shaped clefts inside the arterioles of the dermis, without signs of vasculitis (Fig. 2). Direct immunofluorescence of perilesional skin was negative
What is the Diagnosis?
DiagnosisObstructive Vasculopathy by Cholesterol Crystal Emboli (CCE)The oral anticoagulant was withdrawn. Treatment for this patient included oral prednisolone (0.5mg/kg/day) and statins, with progressive improvement of the cutaneous lesions. Unfortunately, the patient died of nosocomial pneumonia one month later.
CommentsCCE is one of the complications of atherosclerosis. It usually occurs after a precipitating event, such as endovascular procedures, or in association with anticoagulant therapy.1,2
Virtually, all organs can be affected. A variety of clinical manifestations, ranging from asymptomatic to life-threatening, may be observed and are generally nonspecific. Consequently, the diagnosis of CCE is frequently a challenge, because often it simulates other diseases. Despite not being uncommon, it is still an under-recognized disease.1–3
The frequency of cutaneous findings in CCE varies from 35% to 96%. They include livedo reticularis, gangrene, cyanosis, ulceration, nodules, and purpura, which mainly occur on the lower limbs. The differential diagnoses include infectious, inflammatory, and vascular conditions, particularly embolic, coagulopathic, or vasculitic diseases that should warrant a skin biopsy as part of the diagnostic workup. Therefore, the presence of skin involvement, more than any other, should facilitate the diagnosis of CCE. Skin biopsies are fairly sensitive for CCE by showing the hallmark of cholesterol clefts within the arterioles in 92% of cases.3
The prognosis of CCE is poor, with mortality as high as 81%.3
There is no specific treatment for CCE. However, aggressive supportive care has been shown to have a significant benefit. Ceasing anticoagulation is recommended. The benefit of steroids and statins has been suggested, but it is still unclear.3
Although CCE frequently presents as a multisystemic disease, it may also manifest only in the skin, similar to our case, which underlines the importance of the dermato(patho)logist on the correct diagnosis of this condition.
Conflict of InterestThe authors declare not to have any conflict of interest.