Primary cutaneous mucinous carcinoma (PCMC) is a rare neoplasm of the adnexa of the skin, with around 150 cases published in the literature.1,2 Clinically, it usually presents in adults as a solitary, asymptomatic, erythematous nodule, papule, or cyst of variable size, typically occurring on the face or scalp or in the axilla.2 It had been thought to arise from the eccrine sweat glands,2,3 but apocrine differentiation has recently been shown in some cases.1 In general, PCMCs are slow-growing tumors and have an indolent behavior.2 However, late recurrence and metastases have been reported, probably related to incomplete excision of the tumor.3 Histologically, it is indistinguishable from metastatic mucinous adenocarcinomas from other organs,1 particularly from the breast, which can make diagnosis difficult. We present a case of this rare entity and review the literature, discussing the main recommendations and the immunohistochemical reactions useful to reach a correct diagnosis.
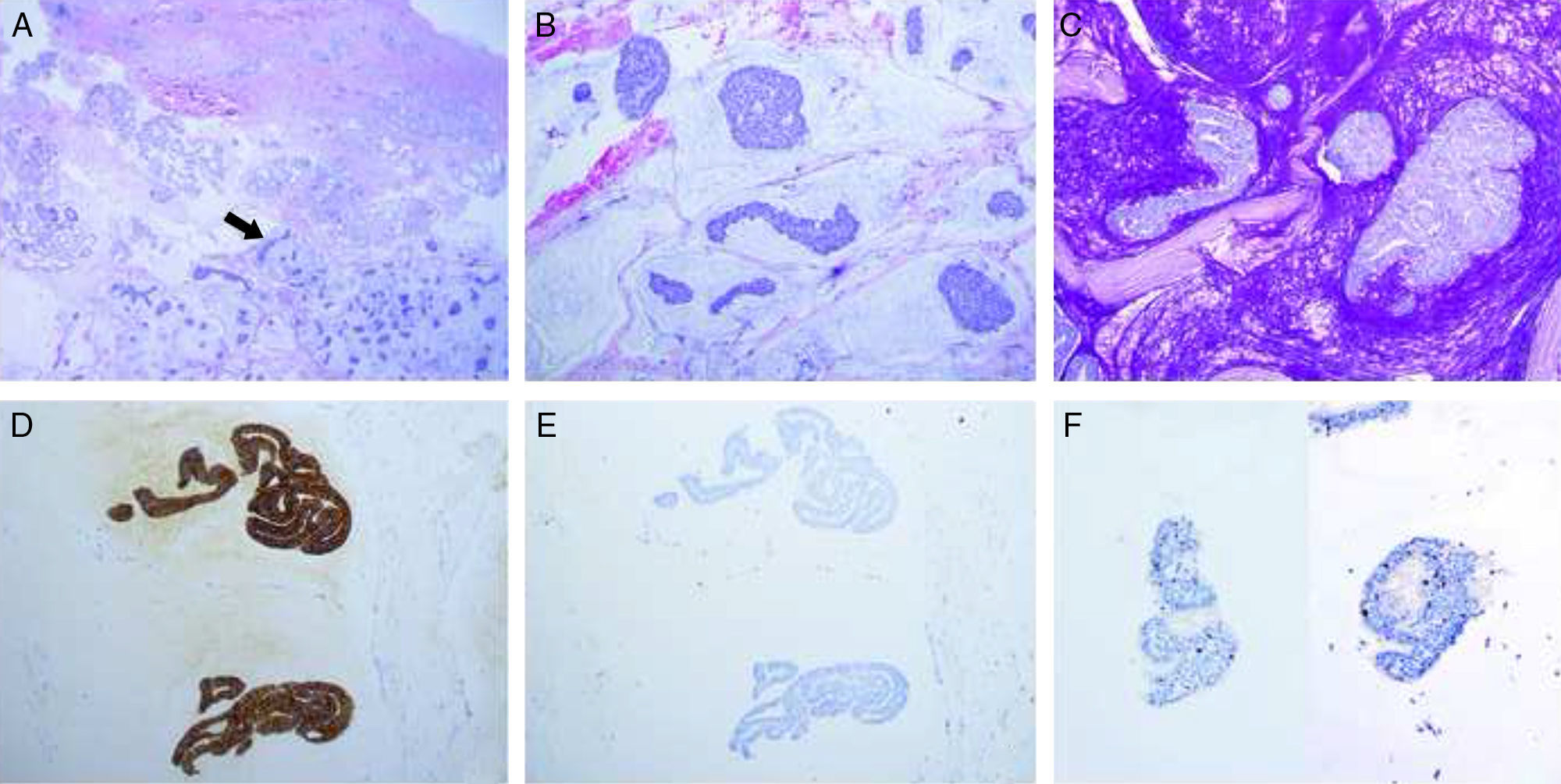
Case DescriptionThe patient was a 68-year-old man with no past history of interest. He was seen for a mobile nodular lesion that had been present for 2 years in the left axilla. The lesion was not adherent to deeper planes and measured 1.5cm in diameter. The clinical diagnosis was epidermal cyst. Macroscopically, the sample consisted of a number of reddish fragments of soft tissue, including areas with a gelatinous appearance, with an overall diameter of 3cm. Histologically, there were fragments of skin with abundant eccrine and apocrine glands that were diffusely infiltrated by lakes of mucin (Fig. 1A). These lakes contained cords and solid nests of cuboidal and round epithelial cells that, in some areas, formed glandular structures, with scattered cribriform lumina (Fig. 1B). The cells presented cytologic atypia and occasional mitotic figures. Periodic acid Schiff stain revealed an abundant quantity of mucin (Fig. 1C). Immunohistochemistry was positive for CK7 (Fig. 1D), CK19, epithelial membrane antigen, GATA3, estrogen receptors (ER), progesterone receptors (PR), and p63 (in isolated small cells) (Fig. 1F); the study was negative for CK20 (Fig. 1E), CK5/6, CD15, and mammaglobin. The pathologic diagnosis based on these findings was mucinous carcinoma. Subsequently the patient underwent complete clinical evaluation, including positron emission tomography (PET) in which no increased uptake was observed in other organs. In cases such as ours, it cannot be ruled out that the tumor may have arisen in a focus of ectopic breast tissue in the axilla; however, as no remnant of healthy breast tissue was observed in the surgical sample, we made a definitive diagnosis of PCMC.
A, Skin sample after removal of the epidermis. Normal skin adnexa may be observed in the mucinous tumor (arrow). Hematoxylin and eosin (H&E), original magnification×2. B, Detail of the tumor with lakes of mucin that contain tumor nests, with a cord-like and cribriform appearance in some areas. H&E, original magnification×10. C, Positive staining with period acid Schiff (PAS) in the lakes of mucin. PAS, original magnification×10. D, Diffuse, intense positivity for CK7 in the neoplastic cells. Original magnification×10. E, Negative stain for CK20. Original magnification×10. F, Two photomicrographs showing details of nuclear positivity for p63 in isolated cells within the tumor nests; these cells correspond to a detectable myoepithelial component in the tumor, supporting the cutaneous origin of the tumor. Original magnification×20.
PCMC is a rare entity that was first described in 1952 by Lenox et al.2 It usually shows an indolent clinical course and is typically present for several years before diagnosis; it is often misdiagnosed clinically as an epidermal cyst, sebaceous carcinoma, cystic basal cell carcinoma, squamous cell carcinoma, neuroma, or pilomatrixoma.2 Late recurrence and metastases due to incomplete excision of the tumor3 and lymphovascular invasion have been reported.4 Apparently, such recurrences have not responded well to treatment with radiotherapy or chemotherapy.3
Morphologically, it is not possible to differentiate PCMC from metastatic mucinous adenocarcinomas of noncutaneous organs.1 Immunohistochemistry can exclude metastatic mucinous adenocarcinomas from the colon, as these tumors are usually positive for CK205 and CDX2, whereas PCMC is negative for these markers. However, immunohistochemistry is not particularly useful in distinguishing PCMC from mucinous adenocarcinoma of the breast, as both tumors can express CK7,1 GATA3,6 mammaglobin, REs, andPRs.1
It has recently been suggested in the literature that detection of a myoepithelial component in the tumor (confirmed by positivity for p63, CK5/6, or calponin, in isolated peripheral cells) supports or suggests PCMC, but unfortunately this is not a common finding.1,2 In our case, we did detect the presence of this remnant of myoepithelial cells with immune stain for p63 (Fig.1F); however, CK5/6 was negative.
In view of this situation, it is strictly necessary to perform a metastatic workup (computed tomography and/or PET), which must be negative in order to confirm that the lesion is not a metastasis from another primary site and to make a definitive diagnosis of PCMC.2
In conclusion, despite the low incidence of PCMC, it must be included in the differential diagnosis of a mucosecretory adenocarcinoma in the skin. Using immunohistochemistry techniques, it is now possible to differentiate PCMC from metastatic mucinous adenocarcinomas from a primary in the colon, as these colonic tumors are positive for CK20 and CDX2. However, no immunohistochemistry panel has yet been identified that will consistently differentiate PCMC from metastatic mucinous adenocarcinomas of the breast, though detection of a residual myoepithelial component (confirmed by positivity for p63, CK5/6, or calponin in isolated peripheral cells) suggests a primary cutaneous origin.1 Finally, it is essential to establish an adequate clinical correlation and make the diagnosis of PCMC as a diagnosis of exclusion, after ruling out the presence of a primary tumor in other organs.1,2
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank the Dermatology Department and the technicians of the Pathology Department of Complejo Hospitalario de Navarra.
Please cite this article as: Areán-Cuns C, Córdoba-Iturriagagoitia A, Aguiar-Losada B, Yanguas-Bayona I. Carcinoma mucinoso primario cutáneo: presentación de un caso. Actas Dermosifiliogr. 2017;108:884–886.