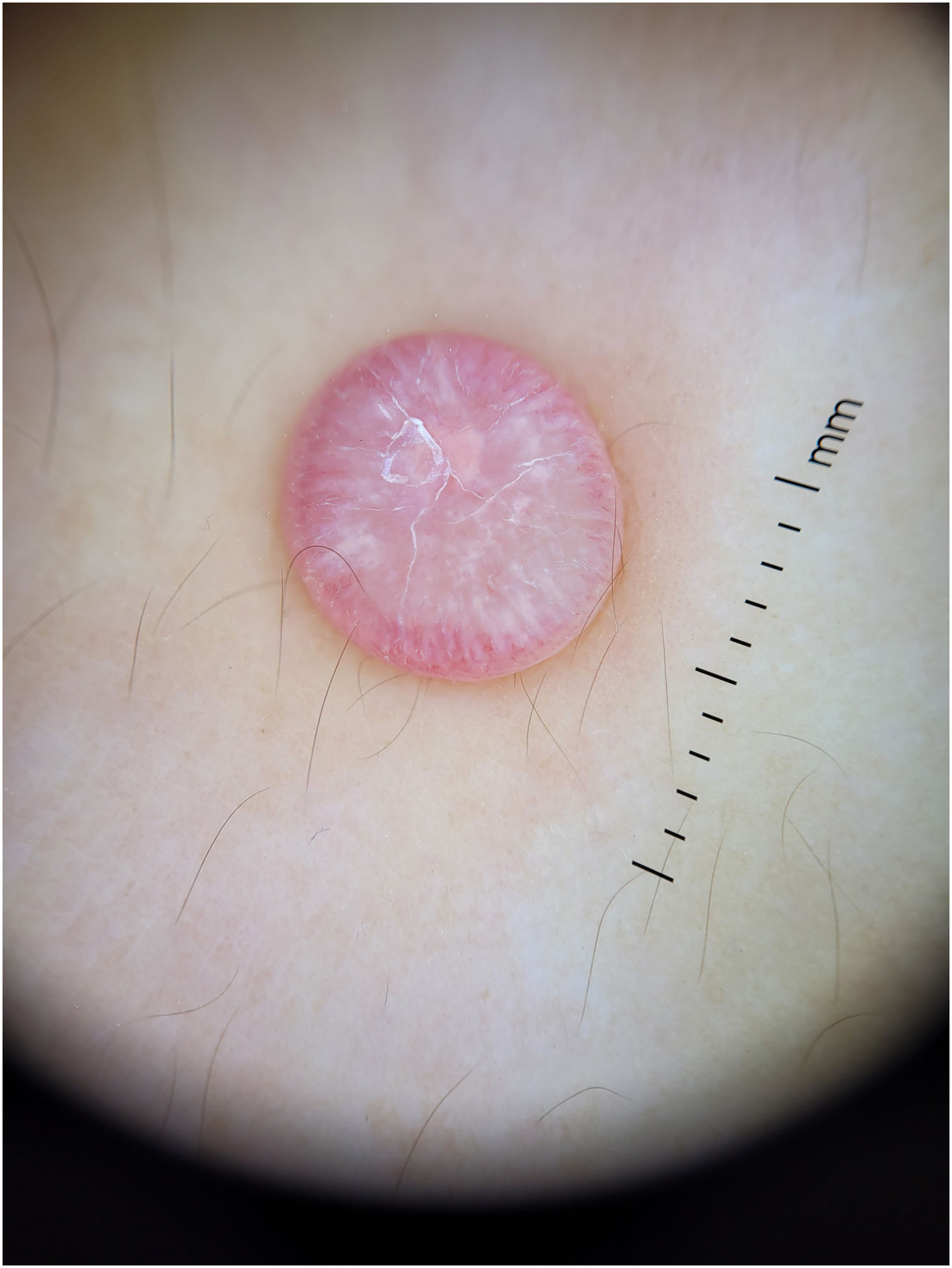
A 12-year-old female, with Fitzpatrick phototype II, presented to the Dermatology outpatient clinic with a 4-month history of anasymptomatic pink nodule on the dorsum of her left hand. A 0.8cm×0.8cm well-demarcated, smooth, exophytic nodule measuring was observed (Fig. 1).
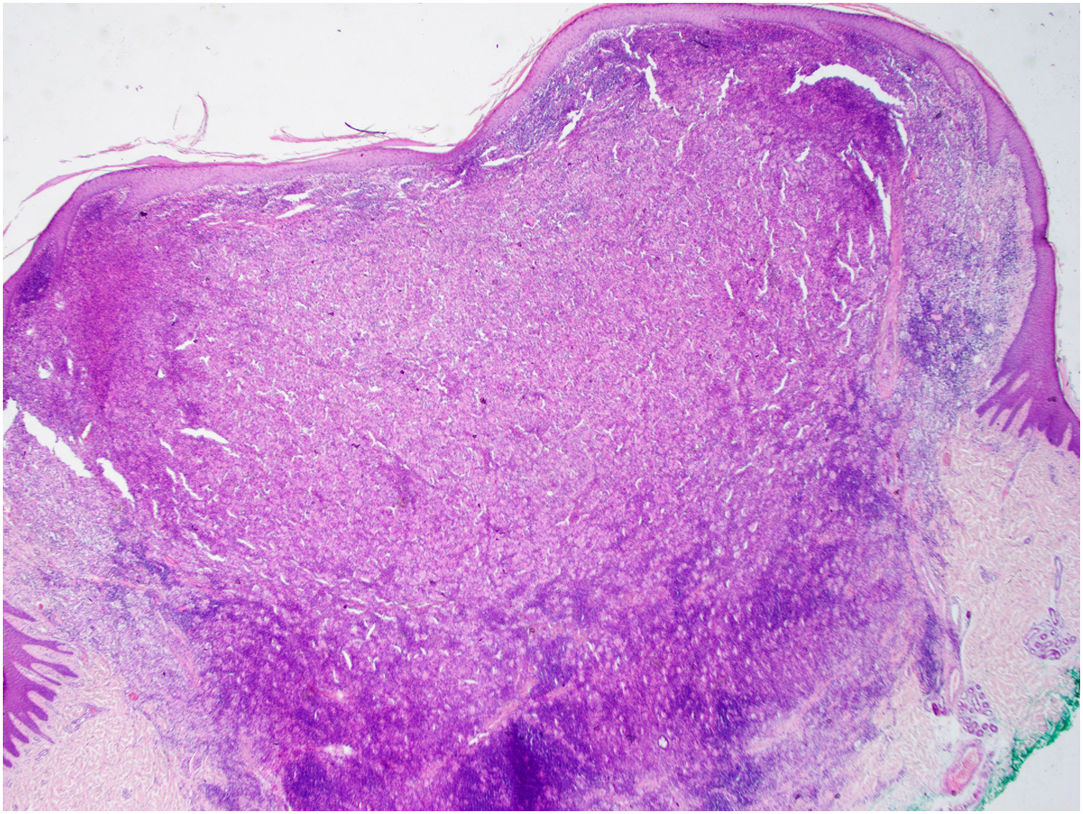
Dermoscopy of the lesion (Fig. 2)
What is your diagnosis?
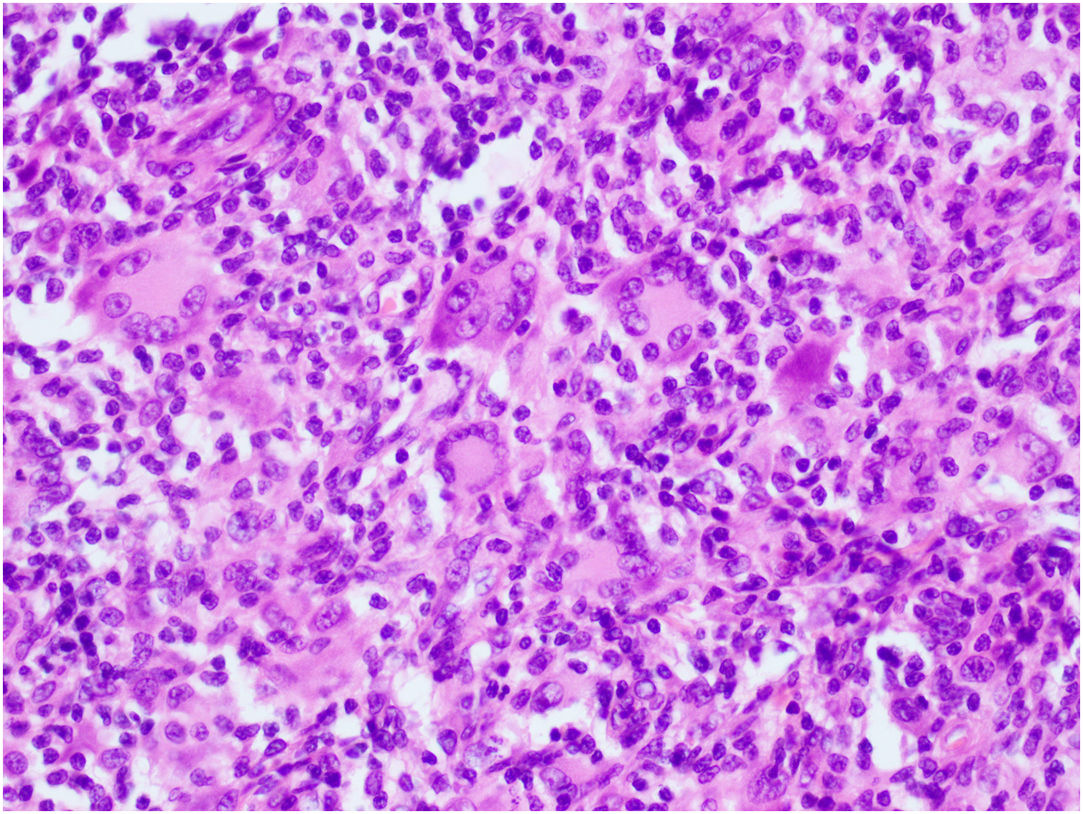
CommentThe dermoscopy of the lesion revealed the presence of a “cloud” of a paler yellow area at the center, shiny white streaks radiating from the it, linear vessels in the periphery, hairpin vessels in the center, and a few scales. The lesion was excised under local anesthesia followed by the simple interrupted suture of the surgical wound. Differential diagnosis included Spitz nevus, solitary reticulohistiocytoma, dermatofibroma and juvenile xanthogranuloma (JXG). Histopathological examination revealed mainly the presence of Touton-type multinucleated giant cells, a few mononucleated histiocytes with large eosinophilic vacuolated cytoplasm, and abundant lymphoplasmacytic inflammatory infiltrate (Figs. 3 and 4). Immunohistochemistry was positive for CD68, S100, and negative for CD1a, Sox 10. These findings, along with clinical examination and dermoscopy, supported the diagnosis of JXG.
The most common form of non-Langerhans cell histiocytosis is JXG. Its clinical presentation are yellow, red, or brown papulonodular lesions, typically seen in individuals within the first two decades of life, often regressing spontaneously.1 Dermoscopy proves to be valuable in distinguishing JXG from other skin lesions, considering its diverse clinical presentations across different stages of evolution.2,3 Histopathologically the early stage of JXG is characterized by sheet-like proliferation of small monomorphous histiocytic cells. As it progresses to its developed stage-xanthomatized cells-Touton giant cells become more prominent. During the transition stage, moderate fibrotic tissue reactions with an increased number of spindle-shaped cells are observed.2,3 The typical dermoscopic “setting sun” pattern characterized by a yellowish background with subtle peripheral erythema is mostly seen during the early, developed stages of the disease. In the transition stage, “clouds” of paler yellow areas are more common, possibly representing the evolution of the yellow background in the “setting sun” appearance.2,3,5 Due to dermal fibrosis at later stages, shiny white streaks or whitish areas with a stellate distribution may be observed.2,3 In all stages of JXG, vascular findings are described, while linear vessels, which may radiate from the periphery to the center, are the most frequently observed. In some cases, dotted, comma-like, coiled, globular, arboriform, hairpin-like and even polymorphic vessels may be present.2–6 Dermoscopic features such as pigment network, follicles, erosions, and scales have also been reported associated with this entity.3,4
Conflict of interestsThe authors state that they have no conflict of interests.