Porokeratosis ptychotropica (PP) is a rare variant of porokeratosis, which occurs in the genital and gluteal regions, and is characterized by multiple cornoid lamellae on histology.1 We present a case of concurrent scrotal and perianal porokeratosis ptychotropica.
A 46-year-old man, of Italian origin, had a 20-year history of recurrent, nodular-verrucous lesions in the scrotum. The lesions were associated with intense pruritus that was exacerbated by stress. He did not suffer from any other cutaneous disease, and there was no family history of similar lesions or other dermatological conditions. The lesions were treated over several years with intralesional steroids and cryotherapy, with partial improvement. Shave excisions of some of the most pruritic plaques provided further relief.
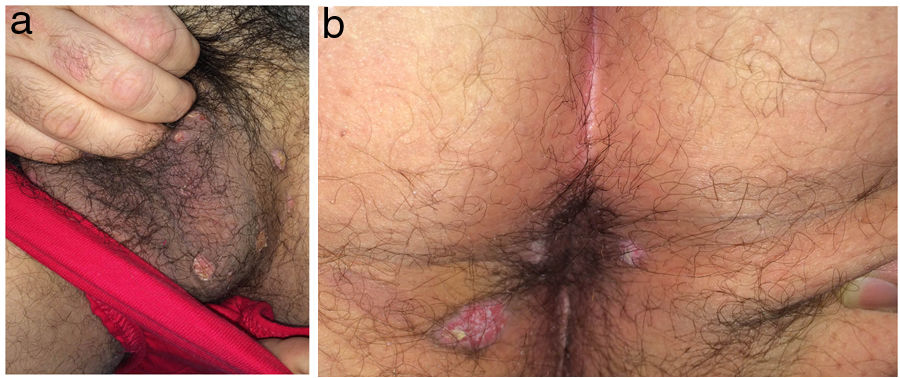
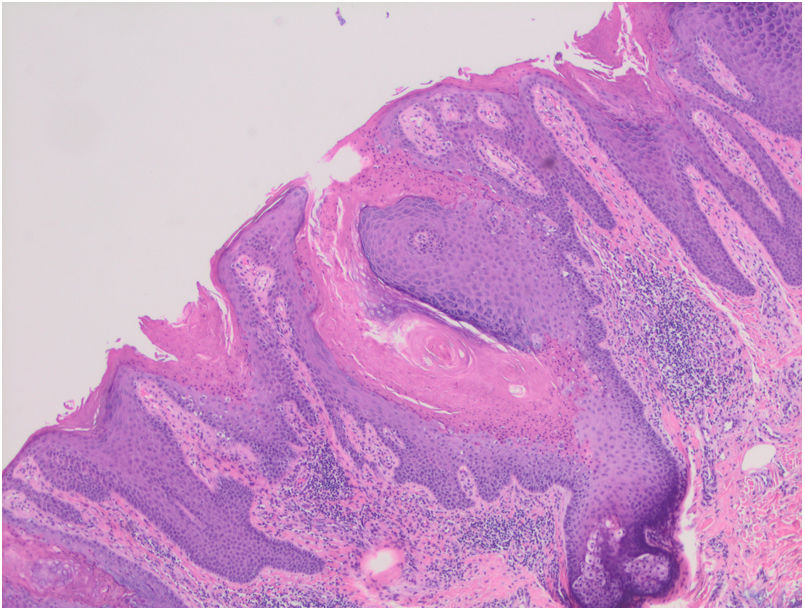
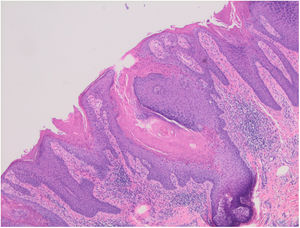
A few months prior to his most recent presentation, he developed some verrucous plaques in the perianal and gluteal region, which were also intensely pruritic. On physical examination there were 3 well-defined erythematous hyperkeratotic plaques on the scrotum (Fig. 1a) and perianal regions (Fig. 1b), measuring around 2cm each. Clinical examination did not find any similar lesions elsewhere on the body. Shave biopsies of the perianal lesions showed psoriasiform epidermal hyperplasia with the presence of several columns of parakeratosis with hypogranulosis (Fig. 2). There were no features to suggest malignancy.
Porokeratosis is a disease of abnormal keratinization. Porokeratosis ptychotropica is a very rare variant with only about 30 reported cases.1 Porokeratosis variants include disseminated superficial actinic porokeratosis, disseminated superficial porokeratosis, porokeratosis of Mibelli, linear porokeratosis, eruptive disseminated porokeratosis, porokeratosis palmo-plantaris et disseminata, porokeratosis punctata, porokeratosis penoscrotal, porokeratosis follicular and porokeratosis gluteo-genital (with three subvariants).2 This particular variant our patient suffers, PP, is named for its ptychotropism, or predilection for body folds, most commonly the gluteal fold.3 Pitney et al. have proposed that porokeratosis ptychotropica may actually represent the clinical end stage of proliferation of lesions of porokeratosis of Mibelli, which have undergone modification by koebnerization, lichenification and other local factors.4
PP initially presents as reddish-brown, hyperkeratotic or verrucous, papules and plaques. Patients often complain of pruritus. Unlike other porokeratotic lesions, they lack the classic elevated peripheral ridges. Satellite lesions grow over several years, eventually fusing into a large, symmetrical, scaly plaque with a “butterfly-shaped” appearance. This classic description mainly only applies to late presentations.1
A common histological finding seen in all variants of porokeratosis is a cornoid lamella; a column of parakeratosis that correlates to the lesions’ hyperkeratotic boundaries. However, PP is unique in that there are multiple cornoid lamellae found throughout the lesion, not just at the borders.1
The pathogenesis of porokeratosis remains unclear, but repeated trauma and immune dysregulation are implicated.5 Amyloid deposition is often seen on the histopathology of PP, which supports a role for repeated friction in its aetiology.6 Immunosuppression may also predispose; a few cases of porokeratosis have been reported in immunosuppressed patients, including a patient with HIV.7 Certain medications have been implicated in the aetiology of other variants of porokeratosis, though not in PP.5 Similar to our patient, another case of porokeratosis was also reportedly aggravated by stress.8
The appearance of PP resembles other common disorders, resulting in frequent misdiagnosis. A slow-growing, scaly, annular plaque on the buttock suggests psoriasis or tinea. Other likely differentials include atopic dermatitis, lichen simplex chronicus and syphilis.1
Treatment of PP is difficult, with variable responses reported to keratolytics, cryotherapy, 5-fluorouracil, imiquimod, vitamin D analogues, diclofenac, corticosteroids, topical antifungals, and lasers. Recurrence is common with all forms of treatment.1 Symptomatic relief from pruritus was observed in two cases treated with photodynamic therapy, however the treatment was not curative and only resulted in partial clearance of the plaques.9 Excision can be curative, but rarely feasible given the size and location of lesions.5 Excision of a 6cm×8cm lesion in a 7-year-old child with PP has been documented, though two small foci of recurrence were seen three years later.10 Recent evidence suggests that many patients with porokeratosis have mutations in enzymes of the mevalonate biosynthetic pathway. Future treatment options may include HMG-CoA reductase inhibitors or inhibitors of preceding steps in the mevalonate biosynthetic pathway.10
There is only one reported case of malignant transformation of PP.3 Though the risk of malignancy may be low, early diagnosis is still important to avoid unnecessary and potentially invasive investigations, and use of ineffective treatments.
This unusual entity should be considered in pruritic, long-standing perianal and scrotal cutaneous lesions, especially in those not responding to therapy. A biopsy will provide the definitive diagnosis. The lesions of PP may significantly impact on patients’ quality of life, both due to pruritus and the large size of plaques in advanced PP. Though individual cases have shown modest improvement with treatment, currently available options are rarely curative. Thus, we highlight the need for increased research into therapeutics.
Conflict of interestsThe authors have no conflicts of interest to declare.