Dermatomyositis (DM) is an idiopathic inflammatory myopathy characterized by muscle inflammation, skin involvement, and systemic manifestations that are often a very broad spectrum in nature.1 Amyopathic DM, also known as DM sine myositis, affects a subset of DM patients and presents with cutaneous symptoms but without myopathy.2
Our patient was a 49-year-old white woman with a history of thalassemia, for which she had been in follow-up for 7 years. She presented with asthenia, itching, and skin lesions located predominantly in photo-exposed areas. Physical examination revealed heliotrope erythema, Gottron papules, Gottron sign, shawl sign, V sign, and Holster sign. A detailed medical history was taken and a systemic review performed, as well as multiple additional tests, including nuclear magnetic resonance imaging of the pelvic girdle, an electromyogram, a muscle biopsy, and determination of muscle enzymes. All results were normal, and the patient was diagnosed with amyopathic DM. Screening for antinuclear, anti-synthetase, anti-TIF-1γ (transcription intermediary factor 1 γ), and anti-MDA-5 (melanoma differentiation-associated protein 5) antibodies and occult tumors was negative throughout the follow-up period.
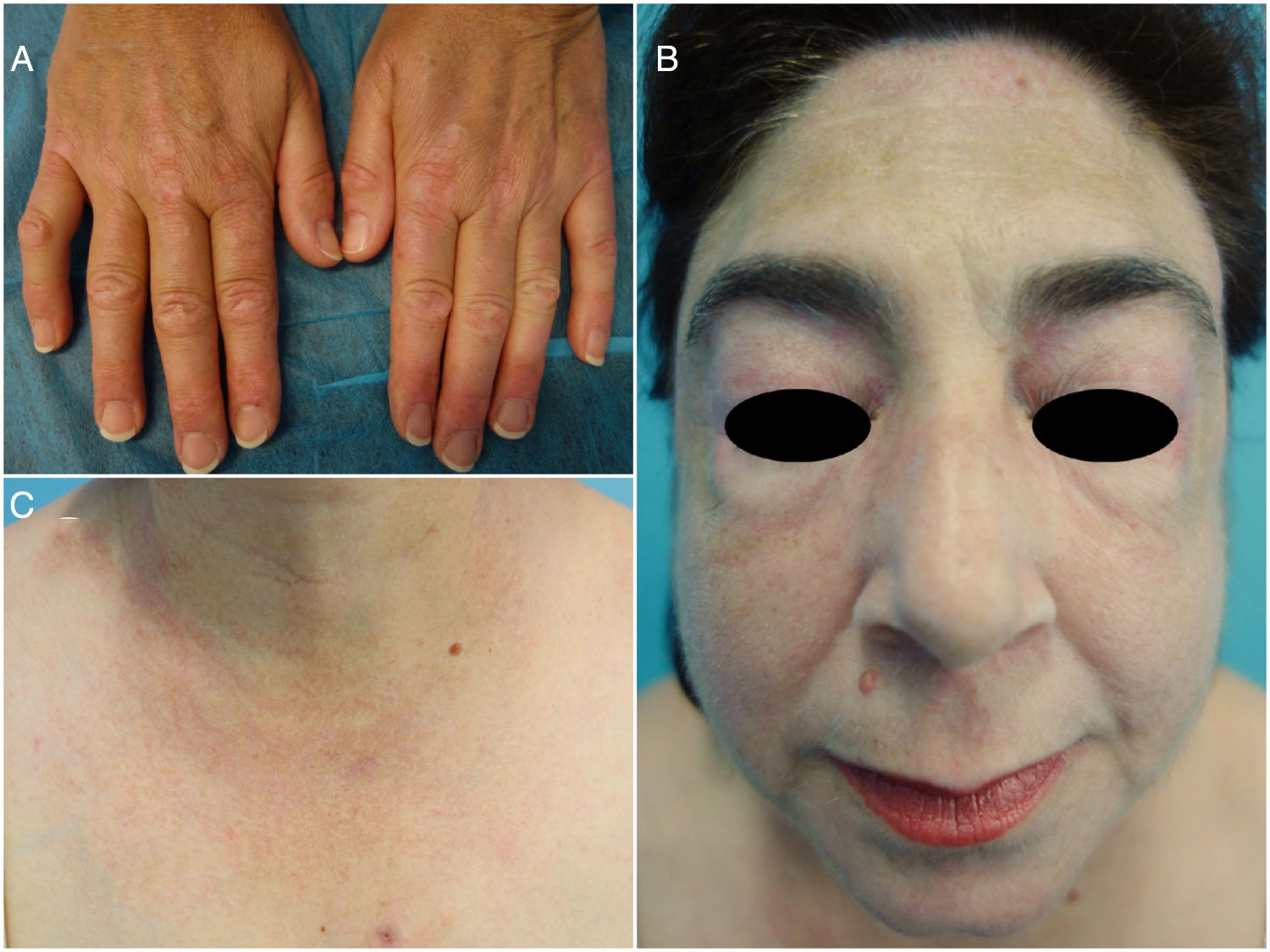
Owing to poor disease control, the patient had undergone multiple treatments to which she responded poorly, including topical and oral corticosteroids (maximum dose, 1 mg/kg/d), azathioprine, methotrexate, hydroxychloroquine, mepacrine, rituximab, oral tacrolimus, intravenous immunoglobulins, and mycophenolate mofetil. She was being simultaneously treated with oral prednisone, hydroxychloroquine, mepacrine, and mycophenolate mofetil up until 7 months before the consultation. Given the progressive worsening of her condition and the severity of the skin lesions (Fig. 1) and pruritus, only treatment with low-dose prednisone (2.5 mg/d) was maintained, and tofacitinib (TOF) treatment (5 mg/12 h) was started.
Clinical improvement was observed 2 weeks later and, at the time of writing, all skin lesions have improved significantly (Fig. 2) and the pruritus has disappeared.
DM is a difficult-to-manage multisystemic disease for which no standardized treatment algorithms have been developed owing to the scarcity of well-designed clinical trials. Furthermore, it is not uncommon for DM to overlap with other autoimmune diseases, posing both diagnostic and therapeutic challenges to physicians.3
TOF is an inhibitor of the Janus kinases JAK3 and JAK1 and attenuates signal transduction activated by interleukin (IL) -2, IL-4, IL-6, IL-7, IL-9, IL-15, IL-21, and type I and II interferons. Because the interferon signaling pathway is overexpressed in DM, TOF may be useful in the treatment of this disease.3,4
Kurtzman et al5 reported promising results in 3 patients with recalcitrant cutaneous DM who were treated with TOF. Subsequently, Paik and Christopher-Stine4 reported a good response to TOF treatment in an adult DM patient who had failed to respond to multiple therapies. In a review by Cinats et al6 of emerging uses of JAK inhibitors in skin diseases, including psoriasis, atopic dermatitis, alopecia areata, vitiligo, DM, and graft versus host disease, adverse effects reported included infections in TOF-treated patients and anemia and thrombocytopenia in those treated with ruxolitinib.6
In the last year, clinical cases have been published demonstrating a therapeutic effect of TOF not only in skin manifestations, but also interstitial lung disease and severe refractory calcinosis, with no notable side effects1,3,7–9 except for transient hypercalcemia and increased body mass index in 2 patients.1
The present case is the sixth published description of amyopathic DM treated with TOF. As in the 5 previously published cases,3,5,7 the patient improved rapidly and treatment was well tolerated.
Clinical trials are required to reliably confirm the efficacy and safety profile of this treatment. A clinical trial is currently underway to evaluate the efficacy of TOF treatment of treatment-refractory DM.10
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Crespo Cruz A, del Boz J, Romero Gómez C. Dermatomiositis amiopática refractaria con buena respuesta a tofacitinib. Actas Dermosifiliogr. 2021;112:374–376.