A 48-year-old female presented with a 5-year history of a mildly pruritic cutaneous eruption starting on the neck and upper chest, gradually spreading to the axilla, arms, and trunk. The lesions had failed to respond to moderate potency topical steroids and improved with short courses of oral steroids, with frequent relapses.
The patient had celiac disease and her family history was irrelevant. She denied any systemic symptoms and she didn’t take any regular medication.
On clinical examination she had numerous widespread, monomorphic skin-colored papules, with a “cobblestone” appearance, symmetrically distributed over the neck, upper trunk, proximal arms, and axilla (Fig. 1a, b). The clinical presentation suggested the diagnosis of pseudoxanthoma elasticum, PXE-like papillary dermal elastolysis (PXE-PDE) or middermal elastolysis.
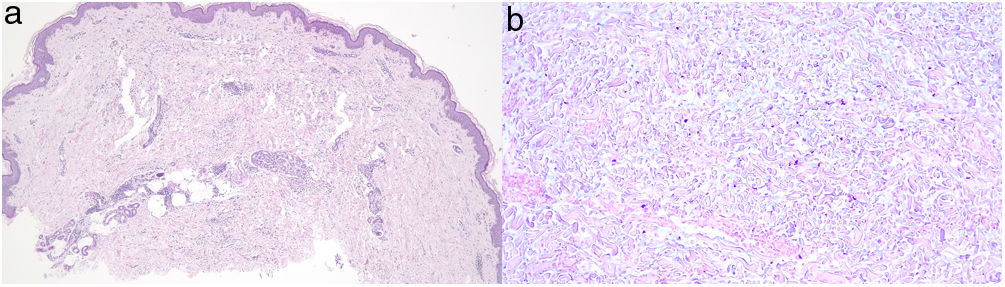
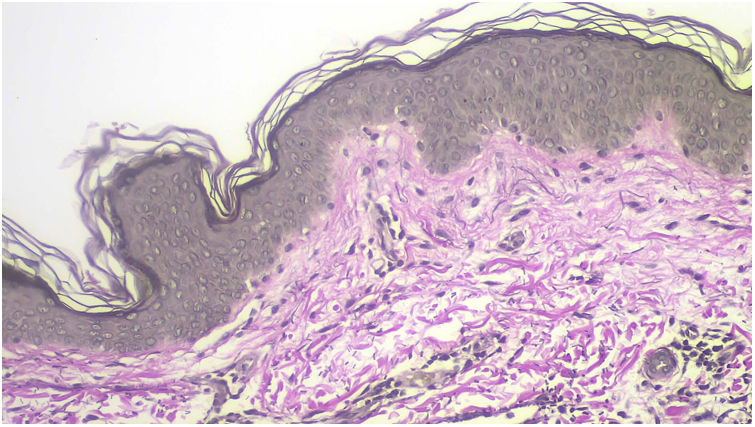
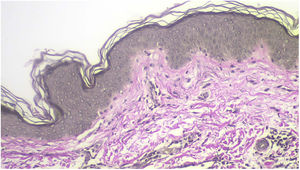
The skin biopsy revealed interstitial dermal infiltration with histiocytes and perivascular lymphocytic infiltrate (Fig. 2a). Alcian blue stain detected deposition of mucin, and Verhoeff stain confirmed regular distribution of dermal elastic fibers, which favored the diagnosis of interstitial granuloma annulare (Figs. 2b and 3).
Laboratory tests, including complete blood cell count, blood chemistry, fasting lipid profile, thyroid profile, antinuclear antibodies, infectious serologies (anti-HCV, HBVs antigen, HIV) and serum protein electrophoresis were unremarkable.
As phototherapy was unavailable because of the COVID-19 pandemic, the patient was started on dapsone 50mg/day, which was discontinued because of gastrointestinal intolerance. When available, the patient started on PUVA, using standard dose oral 8-methoxypsoralen, three times a week, at an initial irradiance of 2.5J/cm2, increasing 0.5J/cm2 per session, as tolerated, with a final dose of 12J/cm2.
There was a significant response after 55 treatments.
Granuloma annulare (GA) is a non-infectious granulomatous dermatosis, classically presenting as annular arranged skin-colored to erythematous papules, involving the dorsal hands and/or feet. Several morphological forms have been described including generalized, subcutaneous and perforating cases. Generalized variant (GGA) presents heterogeneously, with annular plaques seen in only 8–15% of cases. The papular morphology described in our report is though uncommon and presented a diagnostic challenge.1–3
The resemblance with pseudoxanthoma-elasticum and middermal elastolysis has not been described before, though similarities in the pathogenesis of granuloma annulare and middermal elastolysis suggest both entities may be related.4 PXE-PDE, an underrecognized entity, can present with a similar clinical picture, but it typically has a bandlike loss of elastic fibers in the papillary dermis, which was not found in our case (Fig. 3).5
Several other differential diagnosis such as interstitial granulomatous dermatitis, white fibrous papulosis of the neck, papular mucinosis and reticulated erythematous mucinosis could also be considered, though these can be easily ruled out based on clinic and histologic features.5
The diagnosis of GGA requires clinicopathological correlation. The skin biopsy shows palisading granulomas, lymphohistiocytic infiltrate and mucin deposition – a key histological feature to distinguish GA from other granulomatous diseases.1 Of note, in interstitial GA, histopathologic findings are subtle and there is no necrobiosis.6
Several systemic associations have been proposed but they lack scientific evidence and the etiology remains unknown. Insect bites, trauma, herpes zoster, other viral infections, the administration of the bacille Calmette-Guérin (BCG) vaccination and drugs such as biologic therapies have been reported as potential triggering factors.1,7
Further workup for underlying diseases such as diabetes, dyslipidemia, malignancy, thyroid disease and systemic infection is advised in patients with generalized or atypical forms of the disease, as in the reported case.1
Most of the reported treatments in the literature are based on case reports and small retrospective studies, and the outcomes are usually unsatisfactory.1,8
The most popular treatment modalities are topical and systemic steroids, isotretinoin, dapsone, biological agents, surgery, laser treatment, and phototherapy.8 Despite prednisone being effective in many cases, GGA follows a chronic course, requiring a safer long-term therapy.2 Methotrexate is the immunosuppressant most used by dermatologists, other than prednisone.1
Phototherapy, especially PUVA, is the best studied modality of treatment in GGA, with recent analyses advising it as first line treatment, when available.
A retrospective study of 33 patients with GGA treated with PUVA showed significant improvement in 66% of the patients. However most of these patients experienced recurrences within 2 years.9
Another recent retrospective study found a beneficial effect in the majority of patients receiving UVA1 and PUVA.10
The mechanism of action of PUVA in GA is possibly related to the inhibition of T lymphocytes and accessory effects on macrophages and metalloproteinase induction.7 Narrow-band ultraviolet B (NB-UVB) therapy is another viable phototherapy alternative when PUVA is not possible.8
We report a new distinct clinical picture of GGA, which can be misdiagnosed as pseudoxanthoma elasticum and requires accurate clinicopathological correlation to achieve the diagnosis. Additionally, we demonstrate PUVA as an efficient therapy for this challenging-to-treat condition.
Conflicts of interestThe authors declare that they have no conflicts of interest.