Shellac is a known allergen present mainly in cosmetics used on the eyelids and lips, although new sources of exposure have recently been described. Our objective was to assess the use of shellac as a contact allergen in Spain and the clinical profile of patients allergic to shellac.
MethodsThis retrospective cross-sectional study included patients patch tested for shellac between 2018 and 2021 from the Spanish Registry of Contact Dermatitis and Cutaneous Allergy (REIDAC).
ResultsA total of 980 patients were patch tested for shellac (20% in ethanol), and 37 (3.77%, 95% confidence interval [CI], 2.58–3.97%) showed positive results. Most of these patients were tested for shellac due to a suspicion of cosmetic contact dermatitis. Seven patients with present relevance were found, five with relation to cosmetics, and the other two with an occupational background of food handling. The reaction index for shellac was 0.51 and the positivity ratio was 67.56% (95% CI, 52.48–82.65%).
ConclusionsShellac appears to be a prevalent allergen in patients with suspected contact dermatitis related with cosmetics or foodstuff. However, further studies are needed to validate its use in other patients.
El shellac es un alérgeno conocido por su presencia en cosméticos para labios y párpados, aunque en los últimos años se han descrito nuevas fuentes de exposición. El objetivo de nuestro trabajo fue evaluar cómo se está usando el shellac, como alérgeno de contacto en España, y las características clínicas de los pacientes alérgicos al shellac.
MétodosSe realizó un estudio retrospectivo transversal con los pacientes incluidos en el Registro Español de Dermatitis de Contacto y Alergia Cutánea en los que se realizaron pruebas epicutáneas con shellac desde 2018 a 2021.
ResultadosEl shellac (20% en etanol) fue usado en 980 pacientes, con resultados positivos en 37 de ellos (3,77%; intervalo de confianza [IC] del 95%: 2,58-3,97%). La mayoría de estos pacientes realizaron las pruebas epicutáneas por una sospecha de dermatitis de contacto por cosméticos. Se encontraron 7 pacientes con una relevancia presente, 5 de ellos en relación con el uso de cosméticos, y los otros 2 fueron dermatitis de contacto ocupacionales en el contexto de la manipulación de alimentos. El índice de reacción para el shellac fue del 0,51% y la ratio de positividad del 67,56% (IC 95%: 52,48-82,65%).
ConclusionesEl shellac parece un alérgeno frecuente en los pacientes con sospecha de dermatitis de contacto por cosméticos o alimentos. Sin embargo, se necesitan más estudios para validar su uso en otros pacientes.
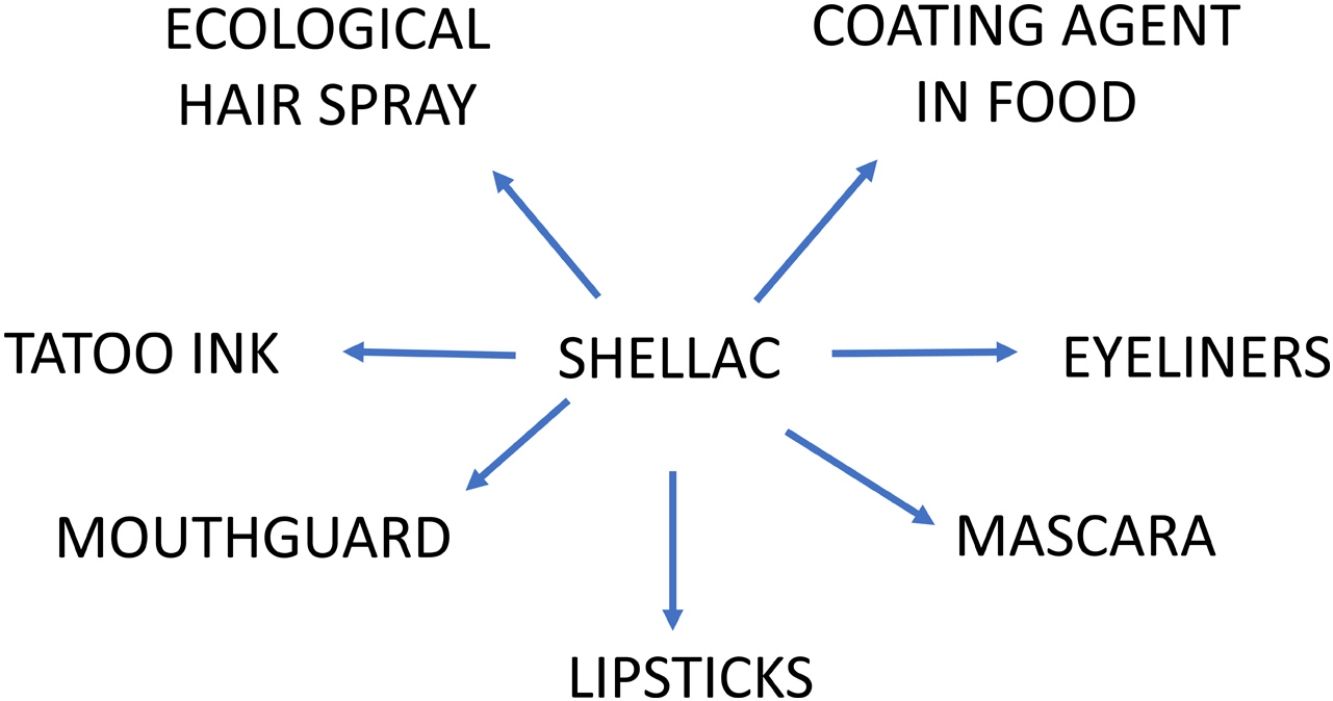
Shellac (CAS no. 9000-59-3, or CAS no. 97 766-50-2 for shellac wax), also known as lac, gomme laque, and lacca, is a purified resin secreted by the female of a Southeast Asian insect known as Laccifer or TachardiaLacca,1 which has multiple uses in the cosmetic, pharmaceutical, and food industries.2 In the 1990s and the first decade of this century, several cases of contact dermatitis associated with shellac use in lipsticks, eyeliners, and mascaras were described.3–7 From 2009 to 2012,8,9 shellac was included in the North American Contact Dermatitis Group (NACDG) baseline series, with a relatively high prevalence of positive tests; 1.6–1.7% of all patients tested, however, it was removed from the NACDG baseline series because more than 50% of positive tests were of unknown relevance and frequent irritant reactions were observed.9 Despite this, in 2020 shellac was included in the American Contact Dermatitis Core Allergen series10 to increase the yield of relevant positive reactions for their patients, however in most countries shellac is tested within specific series, mainly cosmetic series, when clinically suspected. Recently, several clinical reports described new sources of shellac exposure, such as tattoo ink,11 a mouth guard,12 ecological hairspray,13 and cases related to occupational exposure in food handlers14 due to the use of shellac as a coating agent for fruits and sweets. These cases suggest that shellac use could be more widespread than it seems.
Due to scarce comprehensive epidemiological studies outside the United States, we designed a study to investigate how shellac is being used in patch testing in Spain, what the main features of patients allergic to shellac are, relevance of patch testing, and the sources of exposure. Furthermore, shellac has been described as an irritant; therefore, another objective was to assess the validity of patch testing with this allergen.
Material and methodsThe Spanish Registry of Research in Contact Dermatitis and Cutaneous Allergy (Registro Español de Investigación en Dermatitis de Contacto y Alergia Cutánea – REIDAC) is a research project of the Spanish Group for Research in Contact Dermatitis and Skin Allergy (Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea – GEIDAC) which collects results of patch tests performed in 20 contact dermatitis clinics in different Spanish public hospitals; methodology and objectives of the register have been previously described.15
This cross-sectional observational study analyzed data from patients who underwent shellac patch testing from 2018 to 2021. Data were collected using OpenClinica version 3.12 (https://www.openclinica.com/, OpenClinica LLC, Waltham, Massachusetts, USA) and analyzed using Stata version 16 (StataCorp LLC, College Station, Texas, USA). The diagnostic suspicion in most patients was cosmetic allergic contact dermatitis, and they were studied with shellac (diluted 20% in ethanol) included in a cosmetics series supplied by Chemotechnique Diagnostics (Vellinge, Sweden) on Finn Chambers AQUA (SmartPractique, Phoenix, Arizona). In addition to the cosmetic series, all patients were studied with the Spanish baseline series, and patients with a positive patch test for fragrance mix I were also tested with a fragrance series (Chemotechnique Diagnostics, Vellinge, Sweden). The tests were performed and read according to the guidelines of the European Society of Contact Dermatitis (ESCD).16 The intensity and relevance of the positive patch tests of the allergen were assessed, as well as the source of exposure if a present relevance was suspected. We used efficiency as an indicator of both positive test frequency and relevance, calculated as the number of tests needed to get one relevant result, and considered an allergen efficient when less than 200 tests are needed to get one relevant result.17
A descriptive analysis was performed using the χ2 test, and data regarding MOAHLFA index (male, occupational dermatitis, atopic dermatitis, hand dermatitis, leg dermatitis, face dermatitis, age≥40 years) were compared. Additionally, logistic regression with odds ratios (OR) and 95% confidence intervals were performed for the analysis of variables with significant differences between patients allergic and non-allergic to shellac. Irritant or doubtful readings were not included in MOAHLFA calculations.
To assess the validity of shellac skin tests, reaction index18 and positivity ratio19 were used. Reaction index was calculated by dividing the number of positive reactions, excluding doubtful and irritant reactions, by the number of doubtful reactions plus doubtful and irritant reactions. The result gives a number between −1 and 1, values closer to 1 indicate that the preparation gives results that are easier to interpret and reproduce. Positivity ratio is calculated by estimating the percentage of weak positives (+) among the total number of positives (+/++/+++), which is easier to calculate than the reaction index since many weak positives are difficult to interpret and may represent irritant reactions. Ideal values for positivity ratio vary among different studies, with some authors19 stating that values above 80% indicate that the allergen is problematic, whereas others20 consider values above 55% problematic.
The REIDAC study protocol was approved by the ethics committee of Complejo Hospitalario Universitario Insular Materno Infantil de las Palmas de Gran Canaria as a promoter, as well as by each involved center, and was conducted in accordance with the Declaration of Helsinki and attending local and European regulations. All patients involved in the registry signed a written consent form allowing the use of their data.
ResultsDuring the study period, 980 patients from 15 REIDAC centers were tested with the Chemotechnique cosmetic series, with 37 patients showing positive tests to shellac. Of those with positive tests, 25 cases (67.6%) had a weak reaction (+) and 12 (32.4%) had a strong reaction (++), the prevalence of positive test was 3.7% (95% CI, 2.5–3.9%). Additionally, 9 patients had doubtful reactions (+/−) and in the other 3 patients, reactions were qualified as irritant, the proportion of these doubtful and irritant reactions was 1.2% (95% CI, 0.5–1.9%). In 7 patients (18.9%) with positive patch tests relevance was present (Table 1), while relevance was unknown in the rest. In 2 patients, the present relevance was occupational, related to handling of lemons and sweets, while in the other 5 it was related to cosmetics use. The number of tests needed to get one positive relevant result (efficiency) was 140. No significant differences were found in the MOAHLFA index between allergic and non-allergic individuals (Table 2). The reaction index for the preparation used was 0.51 and the positivity ratio was 67.56% (95% CI, 52.48–82.65%).
Clinical features of patients with shellac present relevance upon patch testing.
| Case number | Center | Sex | Age (years) | Main location | Occupation | Source of exposure | Other allergens |
|---|---|---|---|---|---|---|---|
| Case 1 | Hospital Universitario de Araba | Female | 72 | Face | Retired | Cosmetics | Colophonium, 4-tert-butylphenolformaldehyde resin |
| Case 2 | Hospital Universitario La Princesa (Madrid) | Female | 37 | Face | Office worker | Cosmetics | Thimerosal |
| Case 3 | Complejo Hospitalario Universitario Las Palmas de Gran Canaria | Female | 57 | Face | Housewife | Cosmetics | Colophonium, nickel, fragrance mix I, cinnamyl alcohol |
| Case 4 | Complejo Hospitalario Universitario Las Palmas de Gran Canaria | Female | 74 | Face | Retired | Cosmetics | Ylang ylang oil, fragrance mix I |
| Case 5 | Complejo Hospitalario Universitario Las Palmas de Gran Canaria | Female | 38 | Face | Unemployed | Cosmetics | Peru balsam, budesonide, fragrance mix I, isoeugenol, ylang ylang oil |
| Case 6a | Hospital General Universitario Morales Meseguer | Female | 25 | Hands | Worker in a fruit warehouse | Occupational | None |
| Case 7 | Hospital General Universitario Morales Meseguer | Female | 62 | Face and hands | Worker in a sweet factory | Occupational | Tea tree oil oxidized, peppermint oil, lavender absolute, Cananga oil, Ylang Ylang oil, geranium oil, sandalwood oil, 4-tert-butylphenolformaldehyde resin, fragrance mix I |
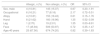
MOAHLFA index of patients allergic to shellac.
| Allergic, n (%) | Non allergic, n (%) | OR | 95% CI | |
|---|---|---|---|---|
| Sex, male | 4 (10.81) | 145 (15.37) | 0.67 | 0.23–1.91 |
| Occupational | 6 (16.21) | 77 (8.16) | 2.17 | 0.72–5.51 |
| Atopy | 4 (10.81) | 155 (16.43) | 0.61 | 0.15–1.76 |
| Hand | 8 (21.62) | 160 (16.96) | 1.35 | 0.52–3.09 |
| Leg | 1 (2.70) | 19 (2.01) | 1.35 | 0.03–8.91 |
| Face | 17 (45.94) | 509 (53.97) | 0.72 | 0.35–1.47 |
| Age>40 years | 25 (67.56) | 674 (74.20) | 0.82 | 0.39–1.83 |
Statistically significant differences in qualitative variants (OR for each item) were calculated using the Chi-square test.
CI, confidence interval; OR, odds ratio; MOAHLFA, male, occupational dermatitis, atopic dermatitis, hand dermatitis, leg dermatitis, face dermatitis, age≥40 years.
The prevalence of shellac allergy in our series (3.7%) was higher than that reported in the NACDG,8,9 but similar to that recently shown by Schubert et al.21 in German patients, with a prevalence of 3.5% in a series of 2167 patients, although these authors included consecutive patients who underwent patch testing, while we mainly used it in patients with suspected cosmetic contact dermatitis. Other studies with patients in which the cosmetic battery was used showed higher frequencies of shellac positives than our sample; for example, the frequency was as high as 10.5%22 in a study performed by the Mayo Clinic and 11.93%23 in a study conducted by the Hospital Universitario de Araba. We believe that the main cause of these varying prevalence rates is the different methods of patient selection for patch testing in the abovementioned studies, which may cause different percentages of positive reactions.
In our study, we found no significant differences in any of the MOALFHA index variables between patients allergic and non-allergic to shellac, similar to the results shown by Schubert et al.21; however, we found seven cases of present relevance in our series, whereas Schubert found no cases. However, in one of the patients with occupational contact dermatitis, the finding was incidental. The tests were performed due to a suspicion of contact dermatitis caused by cosmetics, when the positive test to shellac appeared we could relate it to her work in a sweet factory. The other occupational case was described in a previous article14 and was related to the use of shellac for coating lemons. In that case, there was a clinical suspicion of the source of exposure. The efficiency of patch testing was 140, suggesting that shellac is an efficient allergen at least in the subgroup of patients with suspected allergies to cosmetics or foodstuff.
Another important difference between our results and those of Schubert et al.21 is the high proportion of doubtful and irritant reactions found (8.5%) compared to the much lower proportion shown in our results (1.2%). Veverka et al.22 also found a low prevalence of irritant reactions (0.8%), although these authors excluded 70 patients they described as having macular erythema from their analyses, which may represent irritant reactions. Similarly, Gimenez Castillo et al.23 did not report doubtful reactions in their study although they found that most reactions were weak. Moreover, according to Warshaw et al.,20 they consider shellac as a problematic allergen because the positivity ratio in their series was 76%. However, to classify an allergen as problematic, in addition to the ≥55% positivity ratio, Warshaw et al.20 stated that the reaction index should be ≤0.46. In our study, the ratio of positives was 67.56%; however, the reaction rate was 0.51, so according to the abovementioned study, shellac should be considered an indeterminate allergen. These discrepancies could be due to difficulty in interpreting positive results for this allergen.21,23
Our study had several limitations, one of which is the bias in sample selection. Most of our patients underwent patch testing due to a suspected allergy to cosmetics, which explains the presence of relevant positives, as this is the most frequently known source of exposure described in the literature. Another limitation is that the participation of several centers may lead to differences in interpretation and reading of the tests, particularly for the weak positives.24 It is possible that some of the irritant reactions were not registered or appeared as weak reactions; however, it is also possible that some cases with present relevance were not diagnosed because sources of exposure other than cosmetics were not considered. Finally, the sample size should be larger to allow better measurement of the positivity ratio and reaction index, as studies such as Warshaw et al.20 excluded allergens with fewer than 100 positives from their analyses.
In conclusion, patch testing with shellac in patients with suspected cosmetic allergies, or when occupational use is suspected, appears to be useful. Moreover, the reaction index data and positivity ratio do not clearly demonstrate that shellac is a problematic allergen, at least in these patients. However, larger studies with unbiased selected patients are required to determine the usefulness of adding this allergen to the Spanish baseline series.
FundingREIDAC currently has funding from the Spanish Ministry of Health through an agreement with the Spanish Agency for Medicines and Health Products (AEMPS). The REIDAC accepts donations not conditioned by the pharmaceutical industry. The collaborating companies do not participate, nor have they participated, in the creation or management of the project. The collection, management, analysis, interpretation, publication and review of the data generated in the REIDAC is independent of the public and private funding sources of the project. REIDAC currently receives financial support from Sanofi.
Conflicts of interestPedro Mercader-García reports lectures and advisory boards from Sanofi, Leo Pharma, Lilly and Abvvie, outside the submitted work. Other authors have no conflicts of interest to disclose.
To Ignacio Garcia-Doval and Marina De Vega for their technical support.