Auricular pseudocyst is a rare benign condition clinically manifested as a painless, fluctuant cystic nodule secondary to intracartilagenous fluid accumulation on the lateral or anterior surface of the ear, usually in the scaphoid or triangularis fossa. The etiology is unknown, although chronic low-grade trauma and congenital embryonic dysplasia of the auricular cartilage have been postulated as predisposing factors. We report the case of a patient with bilateral and synchronous auricular pseudocysts that appeared after prolonged wearing of protective masks during the COVID-19 pandemic.
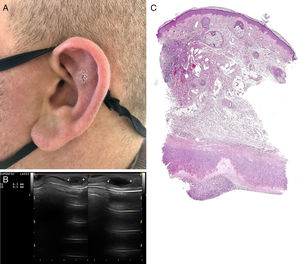
A 35-year-old man presented with slightly tender lesions in both ears that had appeared two months after prolonged wearing (more than 8h per day) non-approved protective masks against SARS-CoV2. The patient denied any local major trauma. Physical examination revealed 5–10mm, elastic, erythematous nodules, located in both left and right upper helix, antihelix and scaphoid fossas of both ears (Fig. 1A). Ultrasounds revealed a hypoechoic cystic lesion with anechoic content and posterior reinforcement with increased cartilage thickness (Fig. 1B). No increased intralesional or perilesional blood flow in the Doppler images were noted. Fine needle aspiration showed a viscous straw-yellow fluid that was sterile after culture. A 3mm punch showed an intracartilaginous cleft devoid of epithelial lining and focal eosinophilic hyaline degeneration of the cartilage along the internal border of the cystic space. The overlying dermis showed a perivascular lymphocytic infiltrate (Fig. 1C). Considering the diagnosis of bilateral auricular pseudocysts, the patient was recommended to wear approved protective masks with a non-tight device in order to avoid local pressure from the ears to the occipital area. Two months later, the lesions had resolved and no relapses were noted after six months of follow-up.
(A) Well-defined non-inflammatory nodules located in the upper helix (small) and scaphoid fossa (biopsy). (B) Ultrasound examination: hypoechoic cystic lesions with anechoic content and posterior reinforcement with increased cartilage thickness in the ultrasounds. (C) Hematoxilin–eosin 10×: intracartilaginous space lacking an epithelial lining with thinning cartilage and hyalinising degeneration along the internal border of the cystic space.
Auricular pseudocyst, also known as benign idiopathic cystic chondromalacia, is a rare and probably underreported condition. Clinically is manifested as a localized oval-shaped swelling arising on the lateral surface of pinna. It usually affects an auricle, but rare cases of bilateral involvement have also been reported.1 Development of auricular pseudocysts has occasionally been related to chronic, repeated and often mild traumatic events (rubbing, ear pulling, sleeping on hard pillows, wearing helmets, earphones or headphones). In our patient, the lesions were bilateral and resolved two months after releasing both ears of the pressure that was being applied by the protective mask. No recurrences were observed during the follow-up. A potential role of mask-induced pressure microtraumatisms could be postulated as a predisposing factor for the bilateral and symmetrical development of these lesions.
During the pandemic, personal protective equipments have been responsible for some skin-related adverse events, specially if prolonged worn.2 Mask usage may have increased the probability of acne flare-ups, commonly called “maskne”, pruritus, worsening of pre-existing dermatoses, irritant contact dermatitis or abrasions.3 Bilateral auricular pseudocysts could probably be added to the list of potential mask-induced skin related side effects.
Pseudocysts of the auricle are usually diagnosed by anamnesis (non-acute painless swelling, usually present metachronously, but can also occur synchronously) and examination (absence of inflammatory signs), although a punch biopsy may help to confirm diagnosis. Ultrasounds is also a technique that may aid in the differential diagnoses that include subperichondrial hematoma caused by accumulation of blood secondary to trauma, relapsing polychondritis, chondrodermatitis nodularis helicis, cellulitis and otoseroma.4,5
In conclusion, we describe auricular pseudocysts as a new complication caused by long time wearing protective masks that should be taken into account due to a worldwide widespread wearing of these as part of personal protective equipment against SARS-CoV2.
Conflict of interestsThe authors declare that they have no conflict of interest.