A man in his 60s presented to the dermatology office with a 10-year history of dermatosis that started on his trunk and gradually expanded to his proximal upper limbs. His past medical history included factor V Leiden mutation, a pulmonary embolism 7 years ago, a myocardial infarction 30 years prior, and fibromyalgia. His medication included acetylsalicylic acid, losartan, verapamil, atorvastatin, and clonazepam. There was no past pharmacological history of drug, alcohol, or tobacco use. His family history was unremarkable. Despite no pruritus or pain, he expressed dissatisfaction with his skin's appearance. Throughout the years, various treatments, such as emollients with urea, topical corticosteroids (betamethasone dipropionate cream), prednisolone, and oral fluconazole proved ineffective.
Physical examinationPresence of symmetrical erythematous patches of fine wrinkles on his trunk and proximal arms (Fig. 1).
HistopathologyHistopathologic examination of a biopsy performed on the patient's dorsum with Hematoxylin & Eosin (H&E) staining [40×] was unremarkable (Fig. 2A). Orcein staining [40×] showed a focal loss of elastic fibers in the mid-dermis (Fig. 2B).
Supplementary testsLab test results were unremarkable, including complete blood count; biochemistry; renal, hepatic and thyroid function; autoimmunity (tests for antinuclear and antineutrophil cytoplasmic antibodies) and viral serologies (HIV, HBV, HCV).
What is your diagnosis?
DiagnosisMid-dermal elastolysis type III.
Clinical course and treatmentWe tried tretinoin cream 0.5mg/g for 2 months with minor improvement; there was no progression of the dermatosis, yet the wrinkled appearance of the patches remained unchanged.
CommentMid-dermal elastolysis (MDE) is a rare acquired elastic tissue disorder that is more prevalent in middle-aged women. Although MDE is limited to the skin and has no systemic involvement, it is associated with numerous concomitant or preceding diseases, particularly autoimmune disorders.1
The precise pathophysiology of MDE is not completely understood. It appears to involve an enhanced elastolytic activity and a decrease in elastic fiber renewal. Multiple cells such as macrophages and fibroblasts are involved in this entity, creating an imbalance between the overexpression of matrix metalloproteinases and decreased expression of tissue inhibitors of metalloproteinases. The triggers for this enhanced elastolytic activity are not fully understood and may include genetic background, chronic inflammation, and autoimmunity.1–3
On physical examination, symmetrically distributed patches of well-circumscribed fine wrinkles (type I), perifollicular papular protrusions (type II), or persistent reticular erythema and wrinkling (type III) can be found on trunk and proximal limbs. Like in our case, type III is more common in older men (>50 years).1
Histopathologic examination with elastica stains (like Orcein or Verhoeff–Van Gieson) is pathognomonic, revealing a band-like or focal loss of elastic fibers in the mid-dermis, with sparing of papillary and deeper reticular dermis and around the appendages.3 Inflammatory infiltrates and macrophages/elastophagocytosis are sporadically seen. MDE belongs to the group of “invisible” dermatoses to the dermatopathologist, with no significant changes in H&E staining. Clinicopathological correlation is essential to perform additional elastica stains to establish the diagnosis of MDE.4
Differential diagnoses include anetoderma, cutis laxa, pseudoxanthoma elasticum-like papillary dermal elastolysis and annular elastolytic giant cell granuloma. Anetoderma presents with smaller, well-circumscribed areas of pouch-like herniations of flaccid skin, with loss of elastic fibers in the papillary and reticular dermis on histology. Cutis laxa presents with loose redundant skin, frequently with internal organ involvement and fragmentation of elastic fibers on histopathology. Pseudoxanthoma elasticum-like papillary dermal elastolysis resembles pseudoxanthoma elasticum clinically, with a band-like loss of elastic fibers in the papillary dermis on histopathology. Annular elastolytic giant cell granuloma comprises erythematous annular lesions with atrophic wrinkled appearance centrally, and on biopsies, a dermal granulomatous infiltrate with loss of elastic fibers centrally is seen.3
Treatment is challenging since, to this date, no treatment allows full recovery of the lost elastic tissue. UV radiation is thought to play a role in the pathogenesis of MDE; therefore, sun protection is recommended. Various topical and systemic treatments have been attempted, including corticosteroids (topical and systemic), tretinoin, hydroxychloroquine, vitamin E, clofazimine, colchicine, dapsone, and mycophenolate mofetil, with modest improvement being reported.3,5,6
Conflict of interestThe authors declare that they have no conflict of interest.


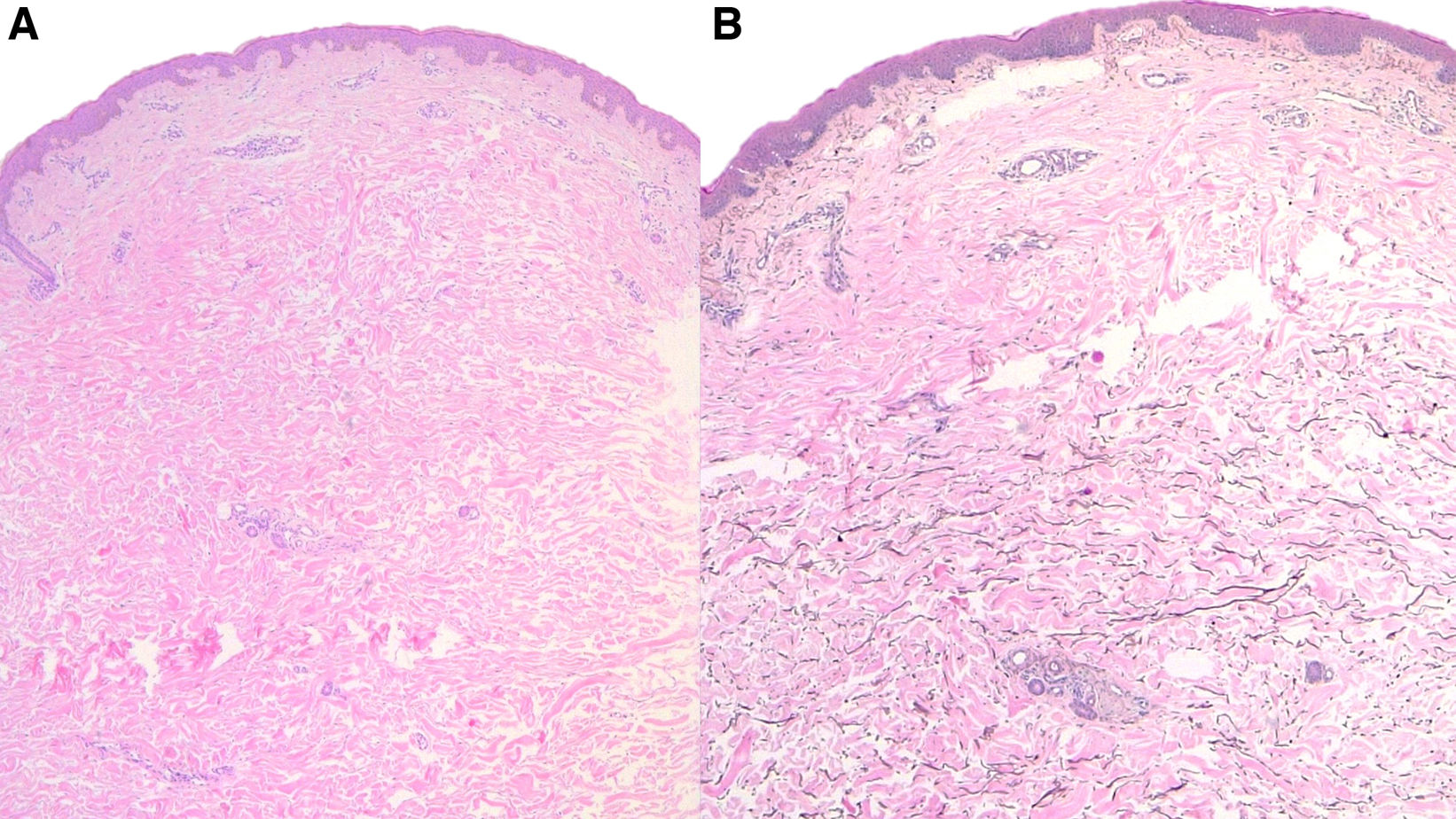

![(A) Histology with Hematoxylin & Eosin stain [40×]. (B) Histology with Orcein staining [40×]. (A) Histology with Hematoxylin & Eosin stain [40×]. (B) Histology with Orcein staining [40×].](https://static.elsevier.es/multimedia/00017310/unassign/S0001731025001139/v1_202503310407/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



