Coronavirus disease 19 (COVID-19) has many manifestations, including respiratory, thrombotic, neurologic, digestive, and cutaneous ones. Cutaneous manifestations have been classified into 5 clinical patterns: acro-ischemic (pseudo-chilblain), vesicular, urticarial, maculopapular, and livedoid. Oral manifestations have also been reported, but much less frequently.
Patients and methodsWe performed a cross-sectional study in which we examined the oral mucosa of 666 patients with COVID-19 at the IFEMA field hospital in Madrid in April 2020.
ResultsSeventy-eight patients (11.7%) had changes involving the oral mucosa. The most common were transient anterior U-shaped lingual papillitis (11.5%) accompanied or not by tongue swelling (6.6%), aphthous stomatitis (6.9%), a burning sensation in the mouth (5.3%), mucositis (3.9%), glossitis with patchy depapillation (3.9%), white tongue (1.6%), and enanthema (0.5%). Most of the patients also reported taste disturbances.
ConclusionsCOVID-19 also manifests in the oral cavity. The most common manifestations are transient U-shaped lingual papillitis, glossitis with patchy depapillation, and burning mouth syndrome. Mucositis with or without aphthous ulcers or enanthema may also be observed. Any these findings may be key clues to a diagnosis of COVID-19.
La enfermedad por coronavirus-19 (COVID-19) se ha relacionado con múltiples síntomas: respiratorios, trombóticos, neurológicos, digestivos o cutáneos. Estos últimos se han clasificado en 5 tipos: lesiones acroisquémicas, lesiones vesiculares, erupción urticarial, exantema maculopapular o lesiones livedoides. Sin embargo, se han descrito mucho menos las alteraciones orales asociadas a COVID-19.
Pacientes y métodosPresentamos un estudio transversal realizado durante abril de 2020 en el Hospital de Campaña de IFEMA examinando la mucosa oral de 666 pacientes con COVID-19.
ResultadosEn total, 78 pacientes (11.7%) presentaron alteraciones en la mucosa oral. La más frecuente fue papilitis lingual transitoria anterior en forma de U (11.5%) asociada o no a edema lingual (6,6%); estomatitis aftosa (6.9%), mucositis (3.9%) glositis con depapilación en parches (3.9%), boca urente (5.3%), lengua saburral (1,6%) y enantema (0.5%). La mayoría refería disgeusia asociada.
ConclusiónLa cavidad oral se puede alterar por la enfermedad COVID-19, el edema lingual con papilitis lingual transitoria en forma de U o la glositis con depapilación en parches son los signos encontrados con mayor frecuencia, al igual que la sensación de ardor en la cavidad oral o boca urente. Otras manifestaciones orales que se pueden asociar a COVID-19 son mucositis con o sin aftas o el enantema. Todos pueden ser signos clave para un diagnóstico de esta enfermedad.
Multiple clinical manifestations of coronavirus disease 2019 (COVID-19) have gradually come to light since the early reports of respiratory and thrombotic symptoms, and include loss of smell, taste disturbances, and neurological and digestive disorders. Cutaneous manifestations of COVID-19 have been classified into 5 clinical patterns: acro-ischemic (pseudo-chilblain), vesicular, urticarial, maculopapular, and livedoid or necrotic.1,2
Oral mucosal changes have also been reported, but much less frequently.1,3
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes COVID-19, binds to angiotensin converting enzyme 2 (ACE-2) receptors, which were recently identified on the dorsum of the tongue and in the salivary glands, confirming that the virus can infect the oral mucosa.4–6
In this article, we describe oral mucosal findings observed in patients with COVID-19 pneumonia at the IFEMA field hospital in Madrid, Spain. Some of these cases are already described in the literature.7 The specific aim of this study was to describe all the oral mucosal changes observed in this series of patients and discuss the possible pathophysiological mechanisms of SARS-CoV-2 infection of the oral cavity.
Patients and methodsDuring the first wave of the COVID-19 pandemic in Spain, the country’s hospitals were so overstretched that it was necessary to open field hospitals. The Community of Madrid installed a provisional hospital at the IFEMA trade show and conference center that provided care to over 4500 COVID-19 patients between March 21 and April 30, 2020. A group of voluntary dermatologists conducted a cross-sectional study in which they examined the mucous membranes of all patients admitted to IFEMA from other hospitals in Madrid. They included patients with pneumonia and a positive polymerase chain reaction test for SARS-CoV-2 or radiological images of COVID-19 without evidence of other causes of pneumonia. The examination of patients was facilitated by the fact that the investigators did not need to change personal protective equipment (PPE) between contacts, as all the patients were examined in a dedicated COVID-19 room. The study was approved by the ethics committee of Hospital La Paz.
ResultsThe mucous membranes of 715 patients were examined. Of these, 666 met the inclusion criteria. The results are shown in Table 1.
Oral Mucosal Changes in Hospitalized Patients with Coronavirus Disease 2019 Pneumonia.
| No. (%) | |
|---|---|
| Oral mucosal changes | 78 (11.7) |
| Transient U-shaped lingual papillitis | 35 (11.5) |
| Tongue swelling | 20 (6.6) |
| Glossitis with patchy depapillation | 12 (3.9) |
| Mucositis | 12 (3.9) |
| Aphthous ulcers | 21 (6.9) |
| Burning mouth | 16 (5.3) |
| White tongue | 5 (1.6) |
| Candidiasis | 3 (1) |
| Enanthema | 2 (0.5) |
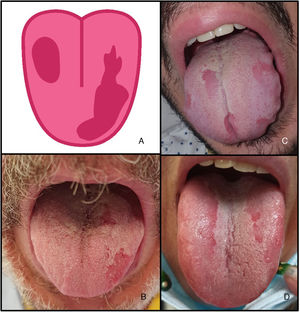
Seventy-eight patients (11.7%) had changes involving the oral mucosa. The most common manifestation was transient U-shaped lingual papillitis, present in 35 patients (11.5%); 20 of these patients (6.6%) also had tongue swelling (Fig. 1).
Characteristic tongue swelling or macroglossia (6.6%) associated with transient U-shaped lingual papillitis (11.5%) in patients with COVID-19. A, Illustration showing tongue changes with indentation on both sides of the tongue and inflammation of anterior papillae, probably caused by friction. B–E, Tongue swelling and transient U-shaped lingual papillitis during COVID-19. COVID-19 indicates coronavirus disease 2019.
Glossitis with patchy depapillation, a characteristic inflammatory pattern of the tongue, was observed in 12 patients (3.9%) (Fig. 2). A fungal culture was performed in all cases and was negative.
Glossitis and patchy depapillation (3.9%) in patients with COVID-19. A, Illustration showing glossitis with patchy depapillation observed in patients with COVID-19. B–D, Patients with glossitis and patchy depapillation. Fungal culture and serology were negative. COVID-19 indicates coronavirus disease 2019.
Other common manifestations were aphthous stomatitis (n = 21, 6.9%) and mucositis (n = 12, 3.9%).
Sixteen patients (5.3%) reported a burning sensation on the tongue or in the mouth; 5 (1.6%) had white tongue and 2 (0.5%) had enanthema.
DiscussionThe reported prevalence of cutaneous manifestations in patients with COVID-19 is variable, and ranges from 7.8% in the study by Giorgi et al.8 to 20% in the study by Recalcati9 and 45.6% in the first study of mucocutaneous manifestations in this series of patients from the IFEMA field hospital.7 There have been few reports, however, of oral manifestations, probably because of fear of infection during examination or the shortage of PPE during the first wave. Enanthema was among the first manifestations to be described. Several cases were mentioned by Galván-Casas et al.,1 who classified the cutaneous manifestations of COVID-19 into 5 patterns. Jimenez-Cahue et al.3 later described enanthema in 29% of COVID-19 patients with a skin rash, which mostly took the form of papulovesicular, purpuric, or erythema multiforme–like eruption.
The most frequently described oral manifestation associated with COVID-19 to date is dysgeusia, with rates ranging from 5.6% in early reports from China10 to 88.8% in a study conducted by ear, nose, and throat specialists.11 Taste disturbances are highly specific to SARS-CoV-2 infection and may or not be accompanied by a loss of smell.11 Dry mouth is also very common and is possibly linked to the destruction of salivary glands caused by the binding of the virus to ACE-2 receptors on the glands.12
We also observed what we consider to be tongue-specific manifestations, such as swelling with characteristic indentation on both sides due to the increased size of the tongue and its pressing against the teeth. This swelling also causes inflammation of the anterior papillae, leading to what we have termed transient U-shaped lingual papillitis. One group of authors reported a case of macroglossia associated with COVID-19 that required treatment with corticosteroids.13 Tongue swelling and irritated papillae can be caused by multiple factors, including direct inflammation of the oral mucosa by SARS-CoV-2, drying of the mucosa due to viral activity or oxygen therapy, or even poor oral hygiene due to the patient’s situation.
Another highly characteristic finding was glossitis with patchy depapillation, observed in 3.9% of patients in our series. Díaz Rodríguez et al.14 also reported a case of depapillation, interestingly associated with a burning sensation in the mouth. Another more recently described oral manifestation is COVID tongue,15 which is similar to geographic tongue but characterized by an increased incidence in patients with SARS-CoV-2 infection. It might be caused by direct binding of the virus to ACE-2 receptors on the tongue or by an increased expression of interleukin 6, which has been described in patients with COVID-19 and patients with geographic tongue. Further studies are needed to better understand this association and its possible etiology and pathogenesis.
Mouth ulcers and aphthous stomatitis have also been described in patients with COVID-19, and in some cases as an early sign of infection16,17; mucositis and aphthous lesions in the mouth have been linked to infections by other viruses, such as herpes simplex and cytomegalovirus.
The sensation of a burning tongue or burning mouth syndrome has also been previously described in association with COVID-19. One Italian study of oral manifestations in 20 COVID-19 patients found that 15% had the sensation of a burning mouth18; this rate is somewhat higher than that of 5.3% detected in our series. The authors of an Iranian study reported a prevalence rate of 68% for oral manifestations of COVID-19 classified into pain, burning, and pruritus.5 These manifestations could have a neurological origin as palmoplantar erythrodysesthesia has also been described in COVID-19.19 A burning sensation in the mouth or on the palms and soles could be a sign of SARS-CoV-2 infection.
Oral manifestations in patients with COVID-19 might be due to SARS-CoV-2-mediated hemolysis (erythrocytes have ACE-2 receptors). The virus might compete with hepcidin, causing increased levels of serum ferritin and, paradoxically, anemia and iron deficiency. Like patients with iron deficiency, they could experience ulcers and a burning sensation in the mouth.20
There have also been reports of new-onset halitosis in patients with COVID-19. Using a halimeter, one group of authors found that patients had increased sulphur compound levels during active SARS-CoV-2 infection and normal levels afterwards.21 As possible reasons, the authors proposed primary, virus-mediated, alterations to the oral mucosa or secondary alterations related to dry mouth and decreased salivary flow.
Possible sources of bias in our study are its cross-sectional design (we do not know the history or outcomes of the lesions identified) and our exclusive focus on patients with pneumonia (we do not know whether patients with few or no symptoms might have developed similar lesions). We also did not find any reports of oral manifestations in hospitalized COVID-19 patients being treated with antibodies, fluid therapy, or mechanical ventilation.
ConclusionsOral cavity lesions are associated with COVID-19 and may be an early sign of disease. Apart from dysgeusia, dry mouth, ulcers, and enanthema, clinicians should also check for tongue alterations, such as transient U-shaped tongue papillitis with or without tongue swelling and glossitis with patchy depapillation. Burning mouth syndrome might also be a sign of COVID-19.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Nuño González A, Magaletskyy K, Martín Carrillo P, Lozano Masdemont B, Mayor Ibarguren A, Feito Rodríguez M, et al., ¿Son las alteraciones en la mucosa oral un signo de COVID-19? Estudio transversal en un Hospital de Campaña, ACTAS Dermo-Sifiliográficas, 2021;112:640–644.