A 53-year-old woman with a personal history of diabetes mellitus was referred to dermatology for painless skin lesions that had first appeared 1 month earlier on the upper limbs and right eyelid, together with joint pain, mainly affecting the shoulder girdle.
Physical ExaminationPhysical examination revealed a hard erythematous-violaceous plaque on the internal canthus of the upper right eyelid (Fig. 1A). Multiple flesh-colored nodules with no erythema or increased temperature were observed on both elbows, the dorsal aspect of the fingers on both hands (Fig. 1B), and the dorsum of the left wrist (Fig. 1C). There were no enlarged lymph nodes.
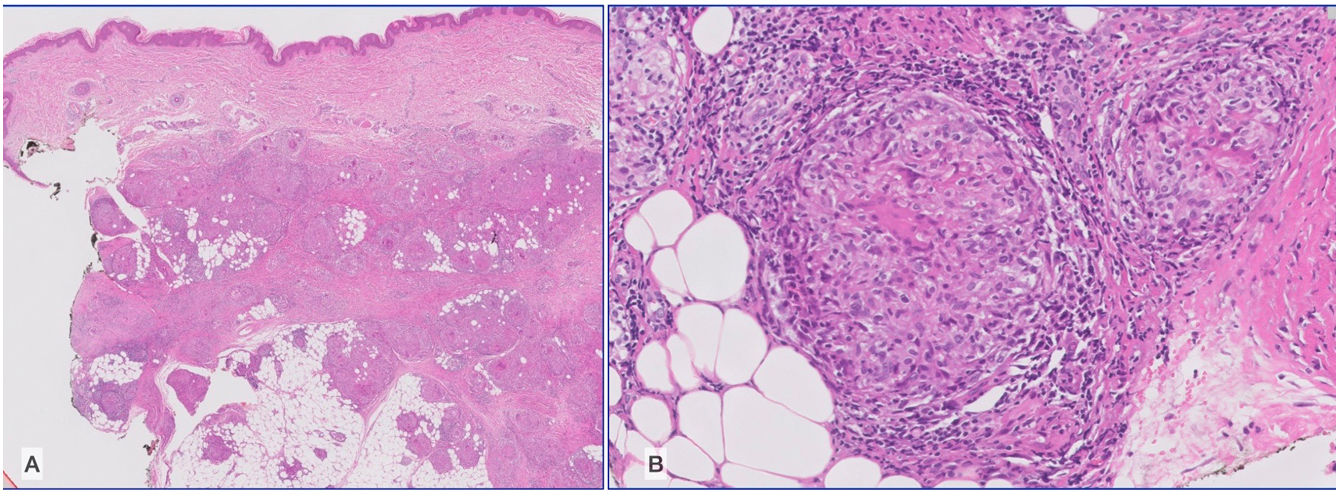
HistopathologyThe histopathology findings for a nodule from the elbow were compatible with tuberculoid granulomatous lobular panniculitis with scant central noncaseous necrosis. The granulomas were located in the deep dermis and subcutaneous cellular tissue (Fig. 2A and B). As this was a poorly specific finding, more frequently observed in mycobacterial infections, we ordered a polymerase chain reaction assay on the specimen provided. Testing ruled out Mycobacterium tuberculosis complex.
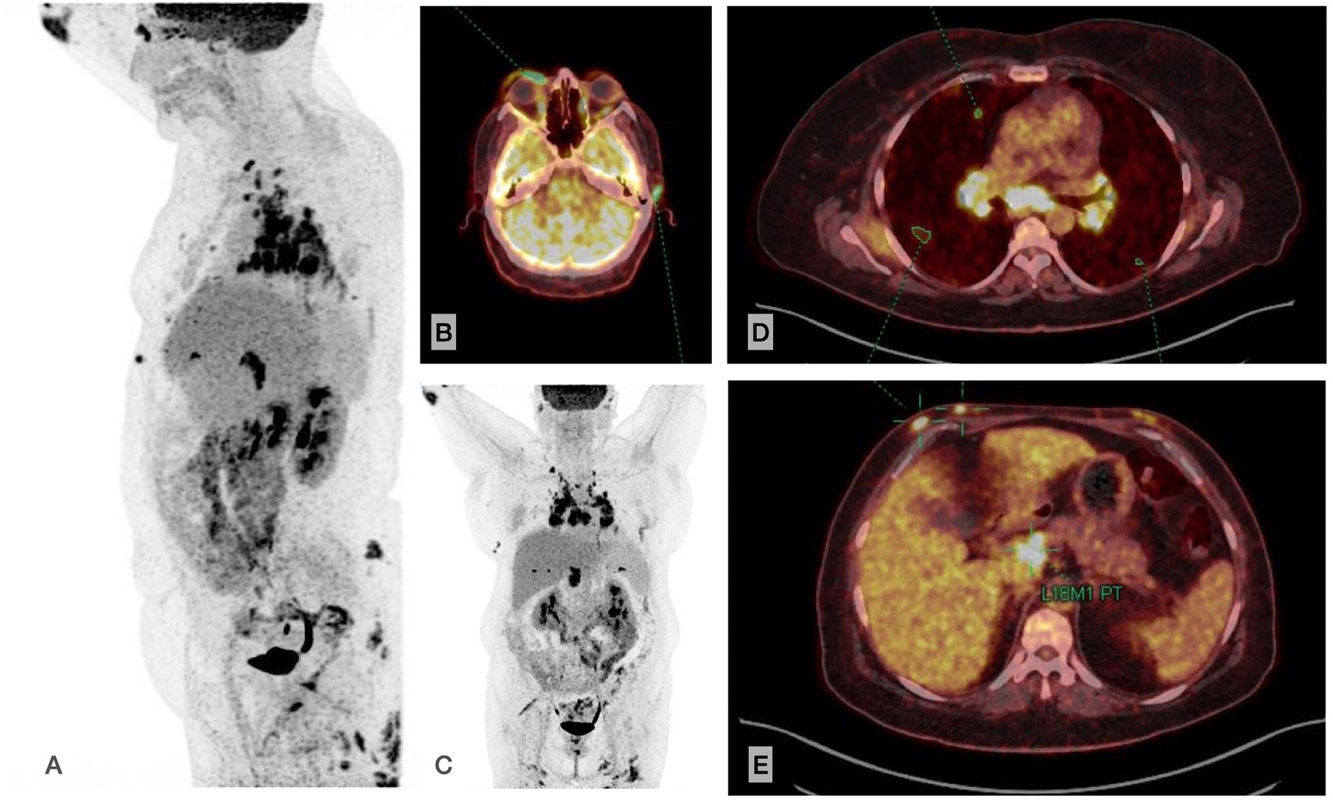
Additional TestsThe laboratory workup was remarkable for a negative result in the interferon γ release assay and increased levels of angiotensin-converting enzyme (116U/L [reference range, 13–63.9]). Positron-emission tomography–computed tomography (PET–CT) confirmed the presence of matted lymph nodes with considerably increased uptake in the mediastinum, supraclavicular fossae, and retroperitoneum (Fig. 3A–C), together with 3 pulmonary nodules (Fig. 3D). We also observed subcutaneous nodules with heavily increased uptake at the abovementioned locations and in the mammary and intergluteal regions (Fig. 3B–D), with a maximum standard uptake value of 6.
What is the diagnosis?
DiagnosisSubcutaneous and plaque sarcoidosis with systemic involvement (pulmonary stage ii).
Clinical Course and TreatmentThe patient had poorly controlled diabetes mellitus, with a baseline blood sugar value of 300mg/dL despite treatment with metformin and canagliflozin. Therefore, she was prescribed subcutaneous methotrexate 10mg weekly. After 1 month with no improvement, the dose was increased to 15mg/d and combined with hydroxychloroquine 200mg. The lesions partially improved thereafter, angiotensin-converting enzyme levels decreased to normal, and the patient remained in quarterly follow-up in our department.
CommentSarcoidosis is a multisystemic granulomatous disease that increasingly affects the lungs and lymph nodes, followed by the skin and eyes. Skin involvement is observed in 20%–35% of cases and may be specific (if sarcoid granulomas are identified in histology) or nonspecific. Co-occurrence of different types of lesion is not uncommon. These include Darier-Roussy subcutaneous sarcoidosis, with a frequency of 11.8%–16% and a female predominance of 2:1. The lesions manifest clinically – as in the present case – in the form of painless elastic nodules with the skin intact located on the limbs.1,2 It is interesting to note that acral involvement in the present case has been reported on only 5 occasions. All the patients were middle-aged adults with associated dactylitis in half of the cases and with mediastinal and bilateral hilar enlarged lymph nodes, except for 1 case, where the finding was unknown, thus indicating a close association between acral and pulmonary involvement.3 The differential diagnosis for the subcutaneous nodules on the fingers should be made with conditions such as subcutaneous granuloma annulare, rheumatoid nodules, xanthoma affecting the joints, and giant cell tumors of the tendon sheath.
Eye involvement is observed in 30%–60% of patients in the form of granulomatous uveitis and/or dacryocystitis. Eyelid involvement is uncommon, usually unilateral, and clinically variable, in the form of erythematous-edematous plaques, nodules, or ulcerations. It generally presents as a solitary finding, with no intraocular eye involvement (3%) and may be asymptomatic or with tearing as the most common symptom, as well as altered visual acuity and ectropion. Diagnosis is based on histology, and the differential diagnosis is with mycobacterial infection, foreign body reaction, acne agminata, and destructive skin tumors. In the diagnosis, it is preferable to biopsy the extraocular lesions owing to the risk of Koebner phenomenon. Therefore, surgery is contraindicated, and the preferred approach is corticosteroid infiltrations or systemic corticosteroids or immunosuppressants.4,5
The risk of systemic involvement is controversial. Subcutaneous sarcoidosis seems to be the only specific manifestation associated with mild systemic involvement, especially the pulmonary form with bilateral enlarged hilar lymph nodes without progressing to pulmonary fibrosis.2 Subcutaneous sarcoidosis has been associated with eyelid involvement in case series, with hilar compromise in 67%,4 thus necessitating screening for systemic disease with a laboratory workup (angiotensin-converting enzyme), chest x-ray, and more sensitive tests such as PET-CT.
Finally, we emphasize that skin involvement is not usually an early finding in the disease and that the ability to recognize it enables us to spare the patient more invasive diagnostic procedures for histologic confirmation.
Conflicts of InterestThe authors declare that they have no conflicts of interest.