The at-home isolation measures mandated during the SARS-CoV-2 pandemic changed daily routines drastically.1 In this context, patients with chronic diseases were deprived of regular medical check-ups. Psoriasis is a chronic inflammatory disease that requires frequent immunomodulatory treatments and periodic examinations by a dermatologist.2
We aimed to investigate how patients with psoriasis accessed follow-up care during periods of precautionary isolation or mandated lockdown measures in Argentina from March to November 2020.3 Clinical course and emotional health during this period were also studied.
This cross-sectional study surveyed patients with psoriasis over the age of 18 years who were on systemic treatment and/or phototherapy prescribed by the dermatology department of Hospital Eva Perón de San Martín in Buenos Aires. The authors developed a questionnaire with 10 multiple-choice items (Table 1). The questionnaires were answered in person, by telephone, or by email during the first 15 days of November 2020, once the lockdown period had ended.
Survey Questionnaire for Patients with Psoriasis on Systemic Treatment and/or Phototherapy During Lockdown.a
| Item or question | Multiple-choice answers |
|---|---|
| 1) Indicate your age group. | 18–39 y/40–59 y/60 y or older |
| 2) Indicate your sex. | Female/Male |
| 3) How were your psoriasis symptoms during the pandemic lockdown? | Better/Worse/Same |
| 4) If you have psoriatic arthritis, how were your arthritis symptoms during the pandemic lockdown? | Better/Worse/Same |
| 5) How was your emotional state during the pandemic lockdown?b | Anxious and/or depressed/Needed a psychologist or psychoactive medications/Thought about suicide/None of the above |
| 6) Did you keep taking your treatment during the pandemic lockdown? | Yes/No/Sometimes |
| 7) If you stopped your treatment, what was the reason? | Fear of getting COVID-19/Obstacles to getting medications/Economic problems/Doctor's orders/Improvement in symptomsc/Had COVID-19 |
| 8) What type of follow-up care did you receive during the pandemic lockdown? | In-person or remote visitsd/Both/None |
| 9) What was your experience with COVID-19 during the pandemic lockdown? | Did not have COVID-19/Had COVID-19 and stayed home/Had COVID-19 and stayed in a hotel or quarantine center/Had COVID-19 and was hospitalized (conventional ward)/Had COVID-19 and was in an intermediate care unit/Had COVID-19 but no symptoms |
| 10) Once lockdown restrictions are over, how would you like to continue your follow-up visits with the dermatologist? | In-person/Remote/Both |
We identified 65 patients who met the inclusion criteria; 47 responded. The gender distribution was similar: 24 respondents (51.8%) were men and 23 (48.9%) were women. The median age was 59.5 years (range, 27–81 years).
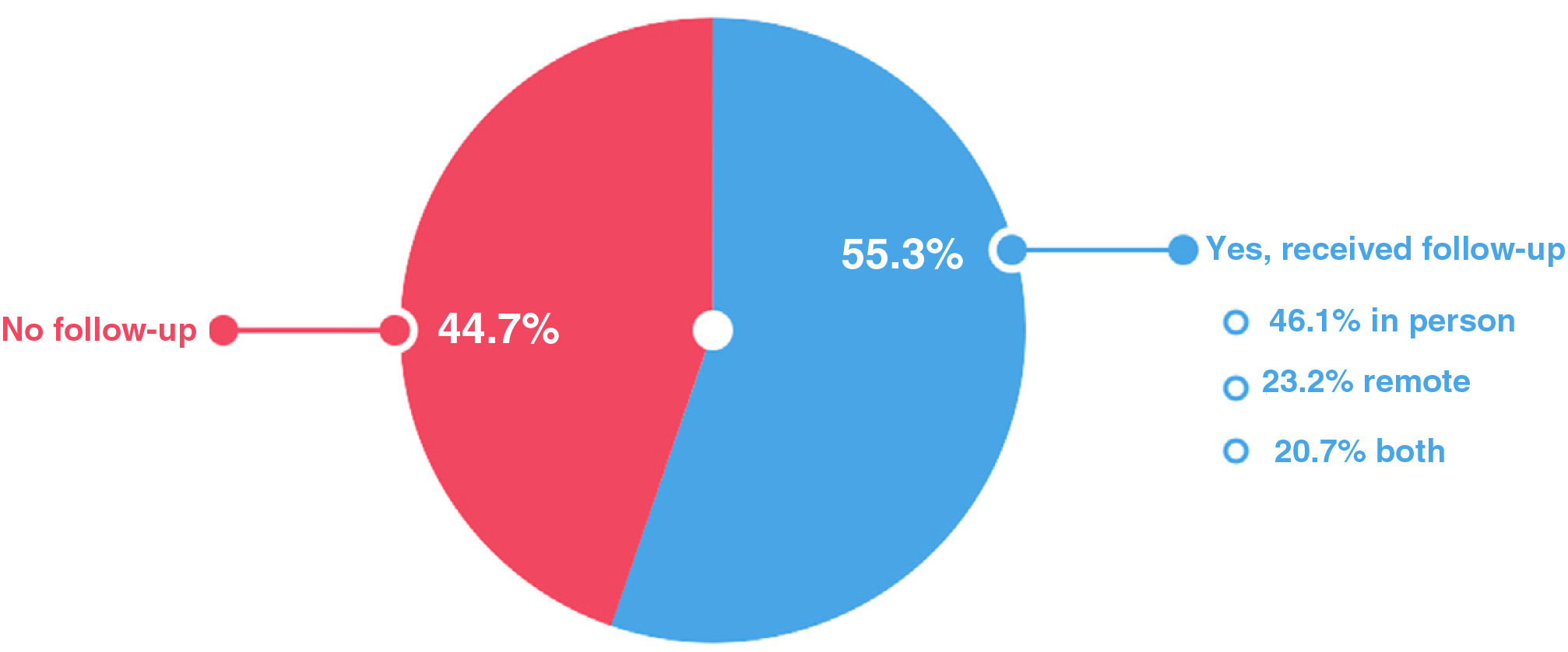
Twenty-one patients (44.7%) had no follow-up visits with a dermatologist during lockdown. Nearly half of the 26 patients who did receive follow-up care (55.3%) had in-person visits (Fig. 1).
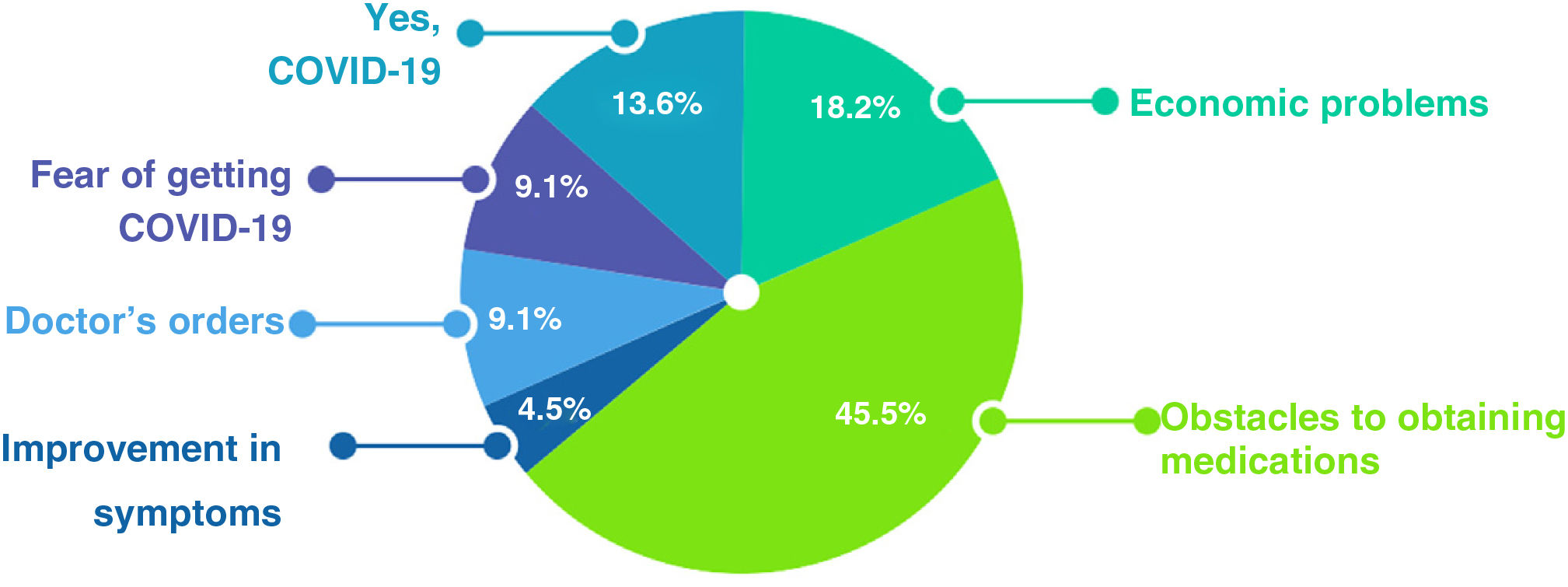
Twenty-two of the 47 respondents (46.8%) reported that they had interrupted treatment during lockdown (Fig. 2). The main reason was difficulty in obtaining medications, reported by 10 patients (45.5%). A second reason was economic difficulty, reported by 4 (18.2%).
Eighteen respondents (38.3%) reported that symptoms worsened, 15 (31.9%) experienced no change, and 14 (29.8%) saw improvement in skin lesions. Of the 17 patients with psoriatic arthritis, 8 (44.4%) said that joint symptoms progressed, 6 (38.9%) reported improvement, and the remaining 2 (16.7%) saw no change.
Responses to the question on emotional wellbeing revealed that 28 respondents (59.6%) experienced anxiety or depression during lockdown. Seven (14.9%) began seeing a therapist or were prescribed psychotropic drugs. Two (4.3%) reported suicidal ideation.
Twenty-six patients (55.3%) expressed a desire to reinitiate in-person dermatology visits once all restrictions were lifted; 20 (42.6%) wanted in-person and remote clinical visits, and 1 (2.1%) preferred only remote communication.
Bearing in mind that psoriasis is a chronic disease and that these patients were on systemic treatment and/or phototherapy, they would require periodic evaluations of response to therapy and tolerance.4 Of the 18 patients who did not receive follow-up care, 6 (33.3%) reported worsening of symptoms. Of the 5 patients with psoriatic arthritis who did not receive follow-up care, 2 (40%) experienced progression of joint symptoms.
Nearly half the respondents interrupted treatment, and disease progressed in 10 of them (45.4%). Difficulty obtaining medications was the main reason for stopping treatment. Similar problems have been reported in other countries. A survey in Italy, for example, revealed that under the period of strictest lockdown measures, 37.2% of patients with psoriasis interrupted treatment due to obstacles to obtaining medications.5
The effect of lockdown on emotional wellbeing was considerable. A meta-analysis published before the pandemic found that 54% of patients with psoriasis experienced stressful events before disease onset or exacerbation.6 Our survey results indicated this association was even more common: 17 of the 18 patients whose disease progressed (94.4%) felt anxious or depressed because of lockdown measures. However, it was noteworthy that patients with suicidal ideation were referred to psychologists for immediate care.
More than half the respondents planned to seek in-person medical visits once restrictions were lifted, a finding that reflects the need to maintain as direct a physician–patient relationship as possible. Apart from meeting the need for a physical examination, we believe in-person visits provide emotional support that is essential for patients with psoriasis and cannot be offered at a distance.
A limitation of our survey was that the sample of 47 respondents who were all treated by the same health facility could not represent the population of patients with psoriasis in Argentina.
In conclusion, our patients with moderate to severe psoriasis had fewer follow-up visits while isolation and lockdown measures were in effect. The decrease had a negative impact on clinical course and emotional wellbeing.
FundingThis paper received no type of funding.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank the patients for their willingness to respond to the questionnaire.