Pediatric vascular malformations are categorized into vascular malformations (VM) and vascular tumors (VT).1 The most common type of VT is infantile hemangioma (IH), while congenital hemangiomas (CH) are much rarer.1 Hemorrhage is a very rare complication of the latter.
In a full-term newborn with the right weight, a controlled pregnancy, and normal prenatal ultrasounds, a total of 3 vascular lesions were identified on the right upper limb (outer wrist, back of the forearm, and elbow), rounded, raised, violaceous, with well-demarcated regular borders, and surrounded by a pale halo.
In an initial ultrasound study, they were described as solid, hypoechogenic, and hypervascularized solid tumors with visible blood vessels, regions of venous ectasia, and arteriovenous shunts inside. These characteristics, along with the clinical presentation described, initially suggested a diagnosis of CH,2,3.
On the second day of life, the lesion on the elbow started to ulcerate (figure 1) and spontaneously bled. However, it was stopped with local compression measures. Four days later, a new pulsatile and abundant hemorrhage occurred triggering a hemorrhagic shock that required emergency blood volume replacement and inotropic support.
Afterwards, due to the risk of recurrent bleeding, surgical excision of the lesion and direct closure of the incision were performed. In later follow-ups, the suture showed dehiscence in its distal part, which healed by secondary intention.
Three months later, despite a significant regression of the remaining lesions (figure 2), they were surgically removed due to their ulceration, a history of hemorrhagic shock, and the difficulties reported by the family to access medical care.
CH, as in the presented case, develop completely in the uterus, and distinguish themselves from IH, in that they are not present at birth. This characteristic justifies their differential diagnosis vs other congenital vascular tumors, such as tufted angioma, or kaposiform hemangioendothelioma.1
The definitive diagnosis is based on the clinical characteristics of the lesion, although additional tests such as ultrasonography, magnetic resonance imaging, or histopathological studies may be required as well.1,3
Since lesions were present at birth, and considering the ultrasound characteristics described, CH was suspected as the initial diagnosis. The rounded, raised appearance of the malformations, surrounded by a pale ring, their smooth telangiectatic surface and coloration support this diagnosis, as documented in the scientific medical literature currently available.3
Following excision, the histopathological examination revealed negativity for GLUT-1, and the presence of large cellular lobules with small capillaries inside over a thickened basement membrane, fibrotic areas, and multiple calcifications, all consistent with the diagnosis of a rapidly involuting congenital hemangioma (RICH).3
CH often have a benign course, and do not require specific therapies. Their involution is especially fast in the case of RICH, as illustrated in the case mentioned earlier. In contrast, non-involuting congenital hemangiomas (NICH) involute only exceptionally.1,3
Overall, VT can present complications, some relatively common, such as ulceration, and others exceptional, such as massive hemorrhages,4 being the latter associated with CH mainly. This could be due to the fact that CH have larger and more superficially located blood vessels.4–6
Hemangioma-related hemorrhages are challenging in terms of management and treatment, potentially posing a life-threatening risk to the patient. The risk factors associated with this complication have not been categorized to date,6 probably due to the low incidence of this entity.
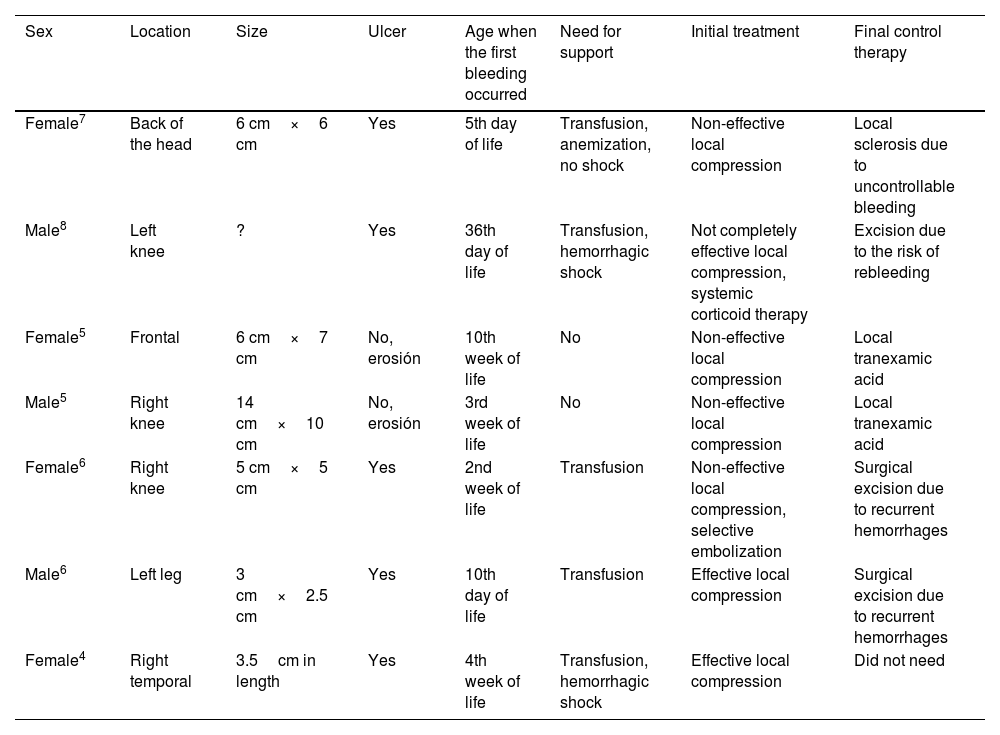
Table 1 illustrates the cases of RICH reviewed and associated with massive hemorrhages published from 1995 through 2018.
Main features of RICHs associated with a massive hemorrhage according to the medical literature from 1995 through 2018.
| Sex | Location | Size | Ulcer | Age when the first bleeding occurred | Need for support | Initial treatment | Final control therapy |
|---|---|---|---|---|---|---|---|
| Female7 | Back of the head | 6 cm×6 cm | Yes | 5th day of life | Transfusion, anemization, no shock | Non-effective local compression | Local sclerosis due to uncontrollable bleeding |
| Male8 | Left knee | ? | Yes | 36th day of life | Transfusion, hemorrhagic shock | Not completely effective local compression, systemic corticoid therapy | Excision due to the risk of rebleeding |
| Female5 | Frontal | 6 cm×7 cm | No, erosión | 10th week of life | No | Non-effective local compression | Local tranexamic acid |
| Male5 | Right knee | 14 cm×10 cm | No, erosión | 3rd week of life | No | Non-effective local compression | Local tranexamic acid |
| Female6 | Right knee | 5 cm×5 cm | Yes | 2nd week of life | Transfusion | Non-effective local compression, selective embolization | Surgical excision due to recurrent hemorrhages |
| Male6 | Left leg | 3 cm×2.5 cm | Yes | 10th day of life | Transfusion | Effective local compression | Surgical excision due to recurrent hemorrhages |
| Female4 | Right temporal | 3.5cm in length | Yes | 4th week of life | Transfusion, hemorrhagic shock | Effective local compression | Did not need |
A total of 57% of them were found on the lower limbs (mainly the kneecap region), and the remaining ones on the cranial pole. The size ranged from 2.5cm to 14cm, and ulceration occurred in 70% of the lesions. Hemorrhages were reported between the 1st and 10th weeks of life, and only once an expectant approach was decided following the hemorrhage.
The case presented here is unusual in terms of its location, since lesions often appear on the upper limbs, a location not previously described. We should also mention the presence of 3 different hemangiomas, which are unique lesions compared to other cases published in the medical literature currently available. Both the size and the timing of the hemorrhage are consistent with the described ranges, and, as in most cases, local compression was not enough to control the bleeding, requiring excision as the final therapy.
In conclusion, although RICHs are rare, and rarely trigger massive hemorrhages, we should be aware of this possibility due to its potential life-threatening consequences. It is also important to consider the limited response of hemorrhages to local measures and the need for advanced support, transfusions, and complex treatments in some cases.
Conflicts of interestNone declared.