Hereditary haemorrhagic telangiectasia (HHT) is characterized by the presence of telangiectases and larger arteriovenous malformations in different organs. Mucocutaneous telangiectases can bleed and become an aesthetic concern, impairing quality of life (QoL). However, the best treatment approach has not been defined yet.
ObjectiveTo evaluate the efficacy and safety of dual wavelength sequential 595/1064nm laser (DWSL) compared to 1064nm laser (Nd:YAG) alone. Secondarily, to evaluate QoL impairment in HHT patients, and its improvement with laser therapy.
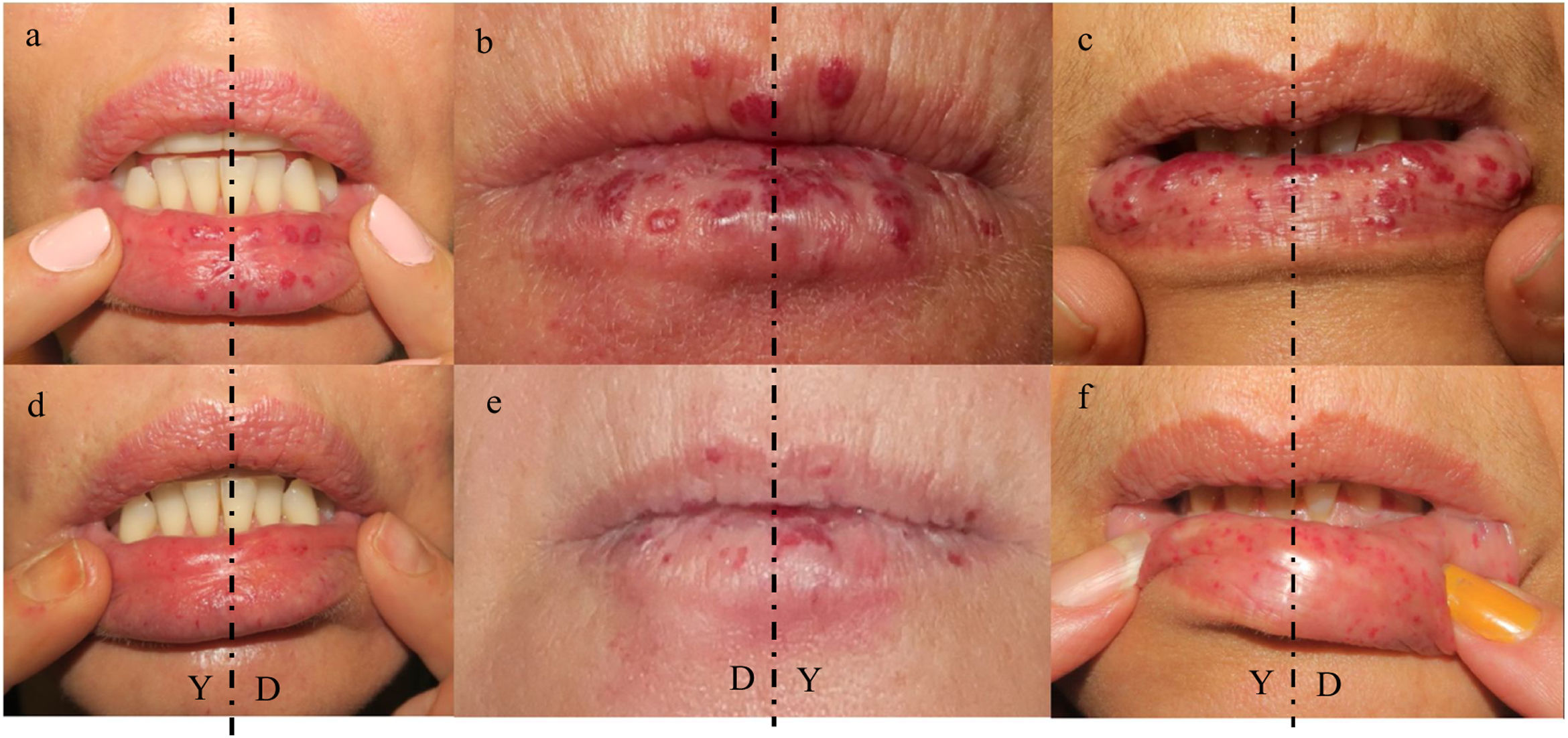
MethodsA comparative randomized split-body double-blinded prospective study (DWSL vs Nd:YAG). Demographic, clinical and treatment characteristics were recorded. The severity and degree of improvement were evaluated by three blinded examiners who scored pre-treatment and post-treatment pictures on a 5-point scale. Patients fulfilled Skindex-29 and FACE-Q® tests and assessed procedure-associated pain and patient satisfaction.
Results111 treatment areas (55 treated with DWSL and 56 with Nd:YAG) from 26 patients were analyzed. The median number of laser sessions was 2 (interquartile range [IQR] 2–4; mean 2.90 vs 2.88, respectively). The median improvement score, irrespective of location, was significantly higher for Nd:YAG compared to DWSL: 3 (IQR 2–3; mean 2.61) vs 2 (IQR 2–3; mean 2.32), p=0.031. Both FACE-Q index and Skindex-29 test results improved significantly (p<0.001), and 92.4% patients reported a high degree of satisfaction (≥8). No severe adverse events were reported.
ConclusionsDWSL and Nd:YAG laser are convenient, safe and effective treatment options for mucocutaneous telangiectases in HHT patients. However, Nd:YAG delivered better results with better tolerability. QoL was significantly improved by both treatments.
La telangiectasia hemorrágica hereditaria (THH) se caracteriza por la presencia de telangiectasias y malformaciones arteriovenosas de mayor tamaño en diferentes órganos. Las telangiectasias a nivel mucocutáneo pueden sangrar y convertirse en un problema estético, afectando la calidad de vida (CdV). Sin embargo, aún no se ha definido su mejor enfoque terapéutico.
ObjetivoEvaluar la eficacia y la seguridad del láser dual secuencial de longitud de onda de 595/1064nm (DWSL) en comparación con el láser de 1064nm (Nd:YAG) solo. Por otro lado, evaluar el deterioro de la calidad de vida en los pacientes con THH y su mejora tras la terapia con láser.
MétodosEstudio prospectivo, doble ciego, aleatorizado, comparativo, de cuerpo dividido (DWSL vs. Nd:YAG). Se registraron las características demográficas, clínicas y del tratamiento. La gravedad y el grado de mejora fueron evaluados por tres examinadores ciegos que calificaron las imágenes previas al tratamiento y posteriores al tratamiento en una escala de 5 puntos. Los pacientes cumplimentaron las pruebas Skindex-29 y FACE-Q® y se evaluó el dolor asociado al procedimiento y la satisfacción del paciente.
ResultadosSe analizaron 111 áreas de tratamiento (55 tratadas con DWSL y 56 con Nd:YAG) de 26 pacientes. La mediana del número de sesiones de láser fue de 2 (rango intercuartílico [RIC] 2-4; media 2,90 vs. 2,88, respectivamente). La mediana de la puntuación de mejora, independientemente de la ubicación, fue significativamente mayor para Nd:YAG en comparación con DWSL: 3 (IQR 2-3; media 2,61) frente a 2 (IQR 2-3; media 2,32), p=0,031. Tanto el índice FACE-Q como los resultados de la prueba Skindex-29 mejoraron significativamente (p<0,001), y el 92,4% de los pacientes informaron un alto grado de satisfacción (≥8). No se informaron eventos adversos graves.
ConclusionesEl láser Nd:YAG y el DWSL son opciones de tratamiento adecuadas, seguras y efectivas para las telangiectasias mucocutáneas en pacientes con THH. Sin embargo, el láser Nd:YAG obtuvo mejores resultados con una mejor tolerabilidad. La calidad de vida mejoró significativamente con ambos tratamientos.
Hereditary haemorrhagic telangiectasia (HHT), also known as Rendu–Osler–Weber syndrome (ORPHA774), is an autosomal dominant condition characterized by the presence of arteriovenous malformations (AVMs) in different locations including the gastrointestinal tract, the central nervous system, the lungs, and the skin.1 HHT can be diagnosed either clinically or through molecular gene testing. For clinical diagnosis, Curaçao criteria (recurrent epistaxis, mucocutaneous telangiectasia, vascular visceral involvement, and a first-degree family member) are used: meeting three or more of these criteria implies a definitive diagnosis of HHT.2,3 Mucocutaneous AVMs of HHT, commonly known as telangiectases, are prone to severe bleeding, mainly epistaxis. Facial and digital lesions are stigmatizing, with a profound impact on quality of life (QoL). Despite these major functional and aesthetic concerns, evidence on treatment of mucocutaneous telangiectases is scarce. Neodymium: yttrium-aluminium-garnet (Nd:YAG) laser has proved its efficacy for the treatment of HHT, but safety is a major concern.
The use of dual wavelength sequential laser (DWSL) with pulsed dye laser (PDL) – Nd:YAG laser could be a safer and more effective alternative than Nd:YAG alone.4,5 DWSL has the advantage of sequentially emitting 595nm PDL and 1064nm Nd:YAG wavelengths from the same handpiece. Thus, PDL first transforms oxyhemoglobin into methemoglobin, increasing three-to-five-fold the absorption of Nd:YAG by the targeted structure. Consequently, it allows the use of lower fluencies of Nd:YAG laser, therefore considerably reducing the risk of side effects.5 DWSL has been used with good results in multiple vascular conditions.5 Also, it has been used to treat HHT with very good responses, similar or even superior to those of other lasers6 (Table 3). However, to our knowledge, no comparative studies between Nd:YAG laser and DWSL for treatment of HHT telangiectases have been published to date.
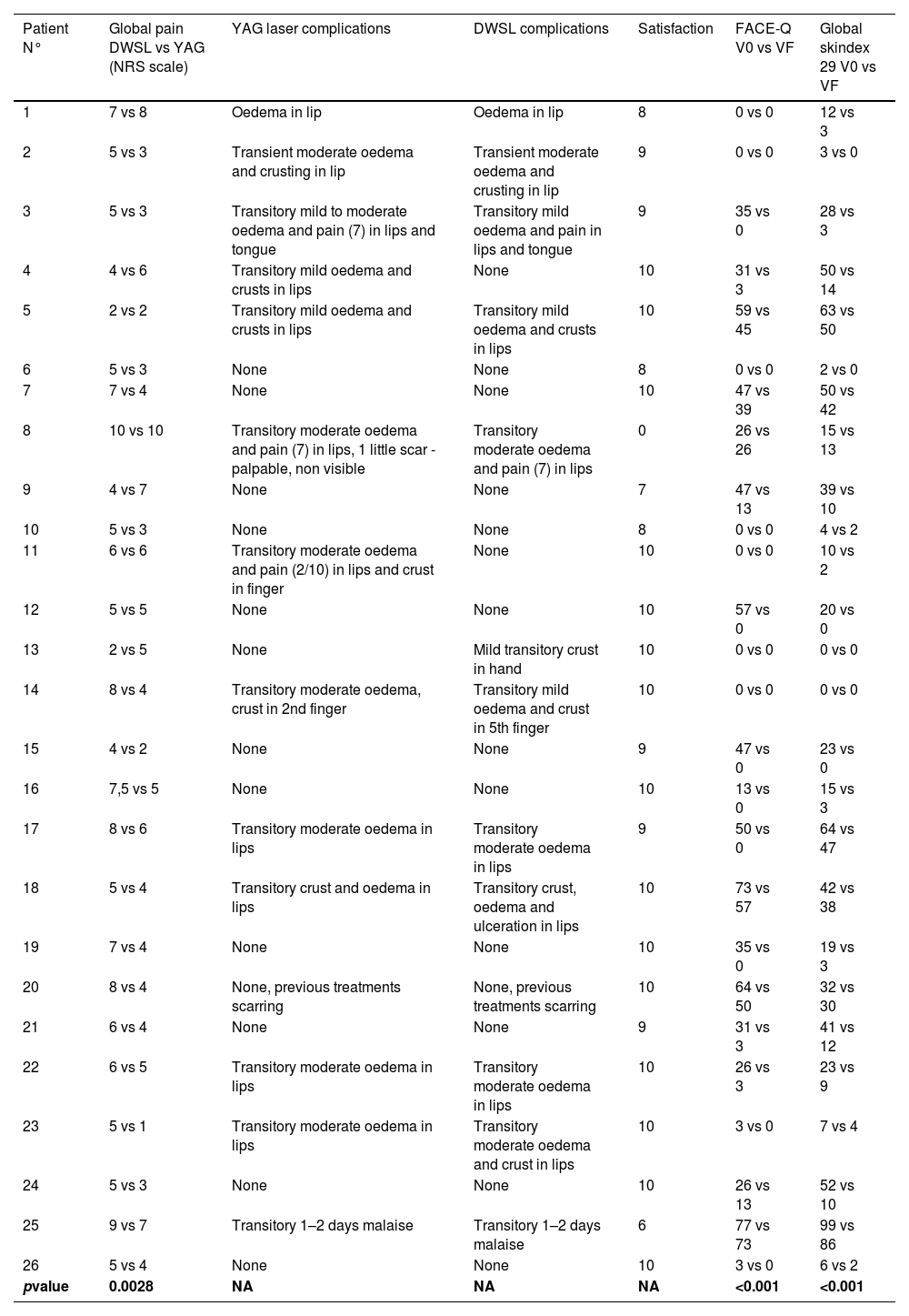
Treatment results.
Shaded areas indicate absence of treatment. Improvement was categorized using a 5-point ordinal relative scale: 0–20%, no response (0); 21–40% poor response (1); 41–60%, partial response (2); 61–80%, good response (3); and 81–100%, excellent response (4).
Abbreviations: DWSL: dual wavelength sequential PDL-Nd:YAG laser; YAG: neodymium-doped: yttrium-aluminium-garnet; PDL: pulsed dye laser; V0: baseline visit; VF: endpoint visit; NA: not applicable/available.
The aim of this study was to compare the efficacy and safety of DWSL versus Nd:YAG for the treatment of mucocutaneous telangiectasia in HHT patients. Secondary aims were to evaluate global laser therapy satisfaction, QoL improvement with laser treatment, and differences in response and tolerance among different therapeutic areas (hands, mouth and face).
MethodsStudy design and patientsWe performed a comparative randomized split-body double-blinded prospective study in HHT patients between October 2018 and June 2022 at the Department of Dermatology of Hospital de la Santa Creu i Sant Pau (Barcelona, Spain). Inclusion criteria were age older than 18 years, a confirmed diagnosis of HHT with active telangiectases requiring treatment and provision of signed informed consent. Exclusion criteria were the presence of photosensitivity (either from disease or drug-induced) and Fitzpatrick phototypes IV–VI (due to the risk of permanent hypopigmentation).
The unit of randomization was the individual body side, with 1:1 allocation ratio, using a random block size of 2. A random number generator was used to generate 0s and 1s, which were designated as left or right. Each random assignment was included as such in the research form. Assignments were made consecutively, with subjects receiving DWSL to the left or right side of the body, and Nd:YAG laser to the contralateral side.
Subjects were blinded by eye shielding as to which body side received which laser treatment. The investigators evaluating therapeutical response were not present during treatments and were blinded regarding identification, type of laser applied and allocation. The Ethical Committee at Hospital de la Santa Creu i Sant Pau approved this study.
Treatment specificationsOur laser treatment protocol for HHT telangiectases was predefined before the onset of the study and was not modified. Lesions on each patient's body side were treated on a single pass per session, through all the study, with dual wavelength sequential PDL-Nd:YAG laser (595 and 1064nm, respectively) (Cynergy with Multiplex™, Cynosure Ltd., Massachusetts, USA) and lesions on the other body side with Nd:YAG laser alone (1064nm, Cynergy, Cynosure Ltd., Massachusetts, USA), respectively. For assessment, all vascular lesions were clustered into three different areas: face, mouth (including lips and tongue) and hands. An air-cooling system (Cryo 6©, Zimmer MedizinSysteme GmbH, Neu-Ulm, Germany), rated at 4–9, was used to protect the epidermis or mucosa. Clinical pictures were taken prior to each treatment session. Skindex-29 test and Face-Q® Appearance-related Distress tests were completed (irrespective of laser type) to assess health-related quality of life (QoL) at every follow-up consultation. No sedation or local anaesthesia were used during the procedure. The choice of laser parameters was individualized for each patient according to clinical details and dermatological criteria. Laser parameters were recorded at the maximum energy used for each individual (independently for DWSL and YAG laser). Patient's pain on each body side and therapeutic area was recorded using a numerical rating scale (NRS), rated from 0 (no pain) to 10 (worst pain).
Follow-up treatment visits were normally scheduled at 4–8 weeks’ intervals. On every follow-up visit, prior to new treatment, complications of previous laser session were assessed as regards post-treatment oedema, blistering, crusts, ulceration, bleeding, scarring and hyper or hypopigmentation. Patients’ satisfaction was assessed using a numerical rating scale (NRS), rated from 0 (extremely dissatisfied) to 10 (extremely satisfied). On achievement of final response further pictures were taken, and more visits were scheduled in case of relapse. All these data were recorded in research forms and – with a template – in the electronic clinical records.
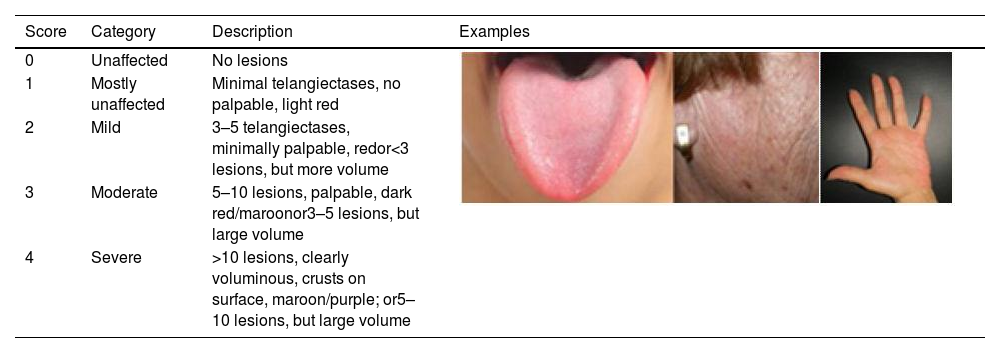
Demographic data, laser parameters, and clinical assessmentBasic demographic data of all patients, location of vascular lesions, prior treatments, laser parameters, number of sessions, complications and degree of satisfaction were retrieved from the study data forms and the clinical records. The initial and final clinical severity and degree of improvement were assessed by reviewing baseline and final pictures for each treated area. Clinical severity and degree of improvement were evaluated and analyzed separately for each topographic area: face, mouth and hand, recording the body side and laser type. Clinical severity was assessed with an ordinal physician's global assessment scale (0–4) (Table 1).6 Improvement was categorized using a 5-point ordinal relative scale. Clinical severity and improvement rates were assessed by two laser surgeons and one general dermatologist who were blinded to the treatment details. Decisions were based on majority agreement; in the event of complete discordance another general dermatologist broke the tie. Skindex-29 test responses were rated on a five-point Likert-type scale and the overall score was transformed into a 100-point scale score. FACE-Q® test responses were rated on a four-point Likert-type scale and transformed to a 100-point scale score, according to the FACE-Q® conversion table.7
Physician's global assessment scale.
| Score | Category | Description | Examples |
|---|---|---|---|
| 0 | Unaffected | No lesions | |
| 1 | Mostly unaffected | Minimal telangiectases, no palpable, light red | |
| 2 | Mild | 3–5 telangiectases, minimally palpable, redor<3 lesions, but more volume | |
| 3 | Moderate | 5–10 lesions, palpable, dark red/maroonor3–5 lesions, but large volume | |
| 4 | Severe | >10 lesions, clearly voluminous, crusts on surface, maroon/purple; or5–10 lesions, but large volume |
Values from 0 to 4 were used, taking into consideration size, volume, colour and number of lesions. See the examples on face and mouth regions.
A sample size of 28 patients was calculated based on a confidence interval of 95% and a precision of 85% with 5% of expected patients’ attrition rate. In this study, each patient side was analyzed using paired samples tests. Demographic data, laser parameters and treatment response were subject to descriptive and inferential statistical analysis. Chi-squared test with Yates’ correction was used for the analysis of categorical variables. Wilcoxon test, Kruskal–Wallis tests, and Spearman's Rho were used for the analysis of quantitative or ordinal variables. All tests were two-tailed and a value of p≤0.05 was considered statistically significant. Statistical analysis was performed using SPSS v. 22 software (IBM SPSS Statistics, New York, USA).
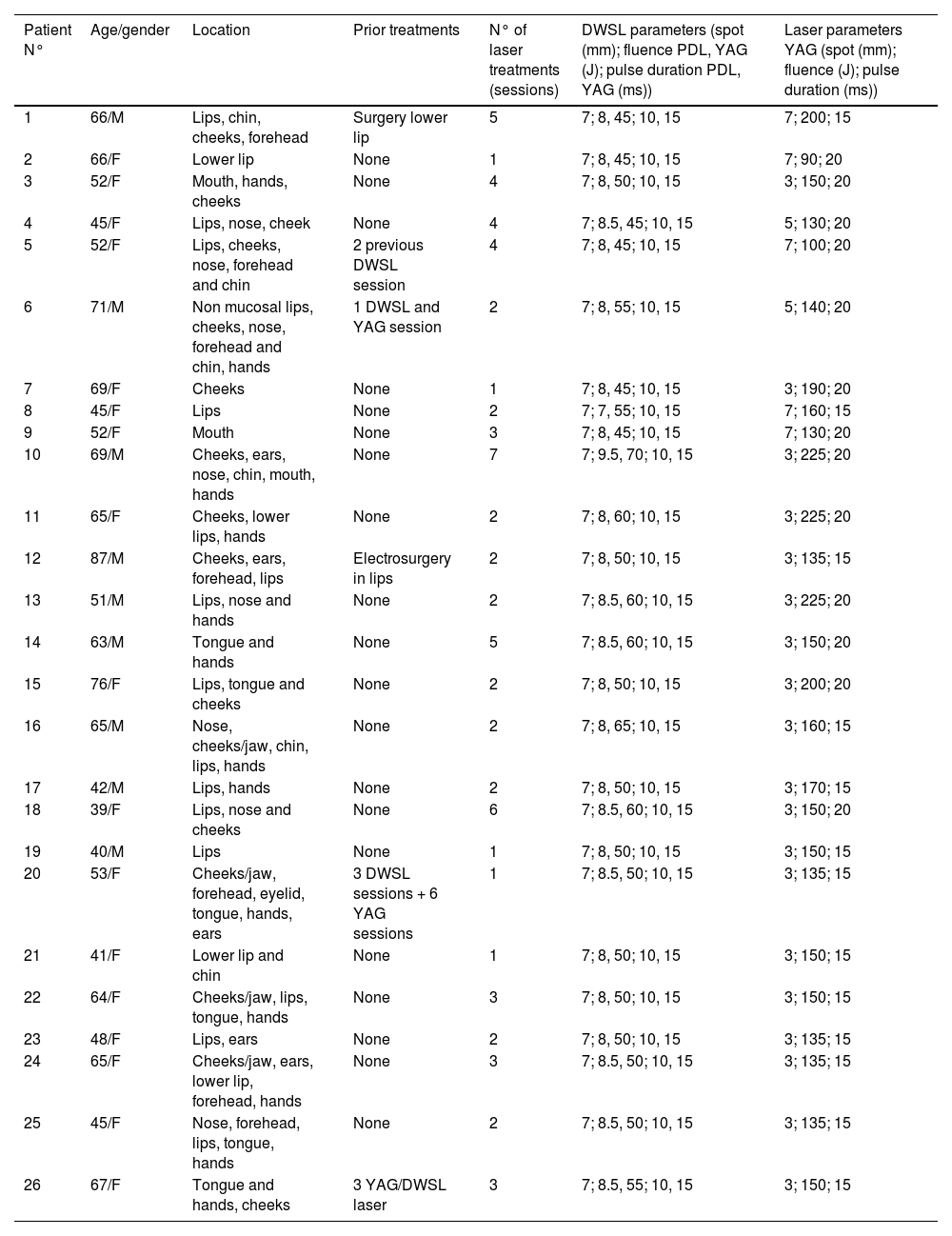
ResultsTwenty-nine clinical records were retrieved, and three patients were excluded due to loss of follow-up. Eventually, data from 26 patients (17 women and 9 men) with cutaneous and/or mucosal telangiectases were analyzed (Table 2). Their median age was 58 years (interquartile range [IQR] 45–66). Telangiectases were predominantly located on the mouth (24 patients), followed by face (20 patients) and hands (13 patients). In total, 111 treated areas (55 treated with DWSL and 56 with Nd:YAG laser) were analyzed. Laser therapy on the setting of this study was the first treatment for most (20, 76.9%) patients. Four patients had previously been treated with laser (Nd:YAG or DWSL), one with electrosurgery and one with surgery.
Demographics and treatment parameters.
| Patient N° | Age/gender | Location | Prior treatments | N° of laser treatments (sessions) | DWSL parameters (spot (mm); fluence PDL, YAG (J); pulse duration PDL, YAG (ms)) | Laser parameters YAG (spot (mm); fluence (J); pulse duration (ms)) |
|---|---|---|---|---|---|---|
| 1 | 66/M | Lips, chin, cheeks, forehead | Surgery lower lip | 5 | 7; 8, 45; 10, 15 | 7; 200; 15 |
| 2 | 66/F | Lower lip | None | 1 | 7; 8, 45; 10, 15 | 7; 90; 20 |
| 3 | 52/F | Mouth, hands, cheeks | None | 4 | 7; 8, 50; 10, 15 | 3; 150; 20 |
| 4 | 45/F | Lips, nose, cheek | None | 4 | 7; 8.5, 45; 10, 15 | 5; 130; 20 |
| 5 | 52/F | Lips, cheeks, nose, forehead and chin | 2 previous DWSL session | 4 | 7; 8, 45; 10, 15 | 7; 100; 20 |
| 6 | 71/M | Non mucosal lips, cheeks, nose, forehead and chin, hands | 1 DWSL and YAG session | 2 | 7; 8, 55; 10, 15 | 5; 140; 20 |
| 7 | 69/F | Cheeks | None | 1 | 7; 8, 45; 10, 15 | 3; 190; 20 |
| 8 | 45/F | Lips | None | 2 | 7; 7, 55; 10, 15 | 7; 160; 15 |
| 9 | 52/F | Mouth | None | 3 | 7; 8, 45; 10, 15 | 7; 130; 20 |
| 10 | 69/M | Cheeks, ears, nose, chin, mouth, hands | None | 7 | 7; 9.5, 70; 10, 15 | 3; 225; 20 |
| 11 | 65/F | Cheeks, lower lips, hands | None | 2 | 7; 8, 60; 10, 15 | 3; 225; 20 |
| 12 | 87/M | Cheeks, ears, forehead, lips | Electrosurgery in lips | 2 | 7; 8, 50; 10, 15 | 3; 135; 15 |
| 13 | 51/M | Lips, nose and hands | None | 2 | 7; 8.5, 60; 10, 15 | 3; 225; 20 |
| 14 | 63/M | Tongue and hands | None | 5 | 7; 8.5, 60; 10, 15 | 3; 150; 20 |
| 15 | 76/F | Lips, tongue and cheeks | None | 2 | 7; 8, 50; 10, 15 | 3; 200; 20 |
| 16 | 65/M | Nose, cheeks/jaw, chin, lips, hands | None | 2 | 7; 8, 65; 10, 15 | 3; 160; 15 |
| 17 | 42/M | Lips, hands | None | 2 | 7; 8, 50; 10, 15 | 3; 170; 15 |
| 18 | 39/F | Lips, nose and cheeks | None | 6 | 7; 8.5, 60; 10, 15 | 3; 150; 20 |
| 19 | 40/M | Lips | None | 1 | 7; 8, 50; 10, 15 | 3; 150; 15 |
| 20 | 53/F | Cheeks/jaw, forehead, eyelid, tongue, hands, ears | 3 DWSL sessions + 6 YAG sessions | 1 | 7; 8.5, 50; 10, 15 | 3; 135; 15 |
| 21 | 41/F | Lower lip and chin | None | 1 | 7; 8, 50; 10, 15 | 3; 150; 15 |
| 22 | 64/F | Cheeks/jaw, lips, tongue, hands | None | 3 | 7; 8, 50; 10, 15 | 3; 150; 15 |
| 23 | 48/F | Lips, ears | None | 2 | 7; 8, 50; 10, 15 | 3; 135; 15 |
| 24 | 65/F | Cheeks/jaw, ears, lower lip, forehead, hands | None | 3 | 7; 8.5, 50; 10, 15 | 3; 135; 15 |
| 25 | 45/F | Nose, forehead, lips, tongue, hands | None | 2 | 7; 8.5, 50; 10, 15 | 3; 135; 15 |
| 26 | 67/F | Tongue and hands, cheeks | 3 YAG/DWSL laser | 3 | 7; 8.5, 55; 10, 15 | 3; 150; 15 |
Abbreviations: ms: millisecond; DWSL: dual wavelength sequential PDL-Nd:YAG laser; YAG: neodymium-doped: yttrium-aluminium-garnet; PDL: pulsed dye laser; M: male; F: female.
The number of laser sessions in our study was similar for Nd:YAG and DWSL: median 2, IQR 2–4 mean 2.88 vs 2.9, respectively. The laser parameters are detailed in Table 2. The median laser parameters in DWSL treatments were spot 7mm, fluence 8J and 50J, duration 10ms and 15ms, for PDL and Nd:YAG, respectively, and spot 3mm, 150J and 17.5ms for Nd:YAG laser. There was no significant correlation between fluence and improvement for either DWSL or Nd:YAG (p=0.45 and 0.92, respectively).
The median global severity scores at baseline were 2 (IQR 2–3; mean 2.4) for DWSL and 2 (IQR 2–3; mean 2.3) for Nd:YAG laser; at the endpoint they were 1 (IQR 0–1; mean 0.74) vs 0 (IQR 0–1; mean 0.52), respectively. There was a statistical trend for correlation between patients’ age and severity at baseline (p=0.078). There were no statistical differences of severity at baseline, between DWSL and Nd:YAG treatments. However, there was a statistical tendence for differences in severity between Nd:YAG group and DWSL (p=0.067) at endpoint. The severity score data by treatment areas are provided in Table 3. The change in severity from baseline to the endpoint was significant both overall (DWSL and Nd:YAG subgroups), for each subgroup (p<0.0001), and for each location considered separately (p<0.0005).
The median improvement score, irrespective of location, was 2 (IQR 2–3; mean 2.32) in DWSL vs 3 (IQR 2–3; mean 2.61) in Nd:YAG treatment (Fig. 1). Differences in improvement between Nd:YAG subgroup and DWSL were statistically significant (p=0.03). By treatment areas, improvement rates are detailed in Table 3. There were no significant differences between areas as regards improvement (Kruskal–Wallis p=0.299). There was no correlation between number of sessions and improvement, regardless of laser modality (p=0.142), for Nd:YAG (p=0.384), or for DWSL (p=0.188).
Twenty-four out of 26 patients reported a high degree of satisfaction with laser treatment (NRS score≥8; median 10 (IQR 9–10, mean 8.9). Pain was bearable in all cases, with a median NRS value of 5 (IQR 4–7, mean 5.65) in DWSL vs 5 (IQR 3–6, mean 4.86) in the Nd:YAG treatment sides. Pain was significantly more intense in DWSL treated sides (p=0.003). By treatment areas, pain was most intense on the hands (median 6, IQR 5–7, mean 6), followed by the mouth (median 5.5, IQR 3.5–7, mean 5.38) and face (median 5, IQR 3–5, mean 4.59) regions. Differences between regions were close to statistical significance (p=0.054). No severe adverse events were recorded. Some patients reported transient oedema and mild pain during the first days, following treatment of mouth lesions (eleven patients out of 24). Patient 2 had a palpable slightly-visible scar on the lip in Nd:YAG side. Patient 4 and 11 had transient oedema and crusts on the lips, only in Nd:YAG side, while patient 13 only crusts on the hands in DWSL side. Three out of 13 patients reported crusts on hands. No other adverse events were recorded. One patient had scarring from previous treatments that persisted at the endpoint visit (patient 20).
In terms of QoL impairment, the median score of FACE-Q test was 28.5 out of 100 (IQR 0.75–47, mean 28.85) at baseline and 0 (IQR 0–13, mean 12.69) by the end of the study. On the other hand, median global skindex-29 score was 21.5 (IQR 7–42, mean 27.65) at baseline and 3.5 (IQR 2–14, mean 14.73) by the end of the study. For both FACE-Q index and Skindex-29 test, differences between baseline and final scores were statistically significant (p<0.001). Adverse events, satisfaction and quality of life evaluation results are detailed in Table 4.
Adverse events, satisfaction and quality of life evaluation results.
| Patient N° | Global pain DWSL vs YAG (NRS scale) | YAG laser complications | DWSL complications | Satisfaction | FACE-Q V0 vs VF | Global skindex 29 V0 vs VF |
|---|---|---|---|---|---|---|
| 1 | 7 vs 8 | Oedema in lip | Oedema in lip | 8 | 0 vs 0 | 12 vs 3 |
| 2 | 5 vs 3 | Transient moderate oedema and crusting in lip | Transient moderate oedema and crusting in lip | 9 | 0 vs 0 | 3 vs 0 |
| 3 | 5 vs 3 | Transitory mild to moderate oedema and pain (7) in lips and tongue | Transitory mild oedema and pain in lips and tongue | 9 | 35 vs 0 | 28 vs 3 |
| 4 | 4 vs 6 | Transitory mild oedema and crusts in lips | None | 10 | 31 vs 3 | 50 vs 14 |
| 5 | 2 vs 2 | Transitory mild oedema and crusts in lips | Transitory mild oedema and crusts in lips | 10 | 59 vs 45 | 63 vs 50 |
| 6 | 5 vs 3 | None | None | 8 | 0 vs 0 | 2 vs 0 |
| 7 | 7 vs 4 | None | None | 10 | 47 vs 39 | 50 vs 42 |
| 8 | 10 vs 10 | Transitory moderate oedema and pain (7) in lips, 1 little scar - palpable, non visible | Transitory moderate oedema and pain (7) in lips | 0 | 26 vs 26 | 15 vs 13 |
| 9 | 4 vs 7 | None | None | 7 | 47 vs 13 | 39 vs 10 |
| 10 | 5 vs 3 | None | None | 8 | 0 vs 0 | 4 vs 2 |
| 11 | 6 vs 6 | Transitory moderate oedema and pain (2/10) in lips and crust in finger | None | 10 | 0 vs 0 | 10 vs 2 |
| 12 | 5 vs 5 | None | None | 10 | 57 vs 0 | 20 vs 0 |
| 13 | 2 vs 5 | None | Mild transitory crust in hand | 10 | 0 vs 0 | 0 vs 0 |
| 14 | 8 vs 4 | Transitory moderate oedema, crust in 2nd finger | Transitory mild oedema and crust in 5th finger | 10 | 0 vs 0 | 0 vs 0 |
| 15 | 4 vs 2 | None | None | 9 | 47 vs 0 | 23 vs 0 |
| 16 | 7,5 vs 5 | None | None | 10 | 13 vs 0 | 15 vs 3 |
| 17 | 8 vs 6 | Transitory moderate oedema in lips | Transitory moderate oedema in lips | 9 | 50 vs 0 | 64 vs 47 |
| 18 | 5 vs 4 | Transitory crust and oedema in lips | Transitory crust, oedema and ulceration in lips | 10 | 73 vs 57 | 42 vs 38 |
| 19 | 7 vs 4 | None | None | 10 | 35 vs 0 | 19 vs 3 |
| 20 | 8 vs 4 | None, previous treatments scarring | None, previous treatments scarring | 10 | 64 vs 50 | 32 vs 30 |
| 21 | 6 vs 4 | None | None | 9 | 31 vs 3 | 41 vs 12 |
| 22 | 6 vs 5 | Transitory moderate oedema in lips | Transitory moderate oedema in lips | 10 | 26 vs 3 | 23 vs 9 |
| 23 | 5 vs 1 | Transitory moderate oedema in lips | Transitory moderate oedema and crust in lips | 10 | 3 vs 0 | 7 vs 4 |
| 24 | 5 vs 3 | None | None | 10 | 26 vs 13 | 52 vs 10 |
| 25 | 9 vs 7 | Transitory 1–2 days malaise | Transitory 1–2 days malaise | 6 | 77 vs 73 | 99 vs 86 |
| 26 | 5 vs 4 | None | None | 10 | 3 vs 0 | 6 vs 2 |
| pvalue | 0.0028 | NA | NA | NA | <0.001 | <0.001 |
Abbreviations: DWSL: dual wavelength sequential PDL-Nd:YAG laser; YAG: neodymium-doped: yttrium-aluminium-garnet; PDL: pulsed dye laser; V0: baseline visit; VF: endpoint visit; NRS: numerical rating scale, NA: not applicable/available.
Nd:YAG laser may be considered the gold standard of treatment for HHT mucocutaneous telangiectases, since it reaches a depth of 5–6mm, corresponding to the usual location of HHT telangiectases.8 However, despite the proven benefits of Nd:YAG laser for the treatment of HHT, with more than 50 reported patients,9–11 safety concerns limit its use. Its small therapeutic window may lead to potential tissue necrosis and scarring due to unwanted thermal damage.5 Thus, it would be convenient to find an equally effective but safer alternative.
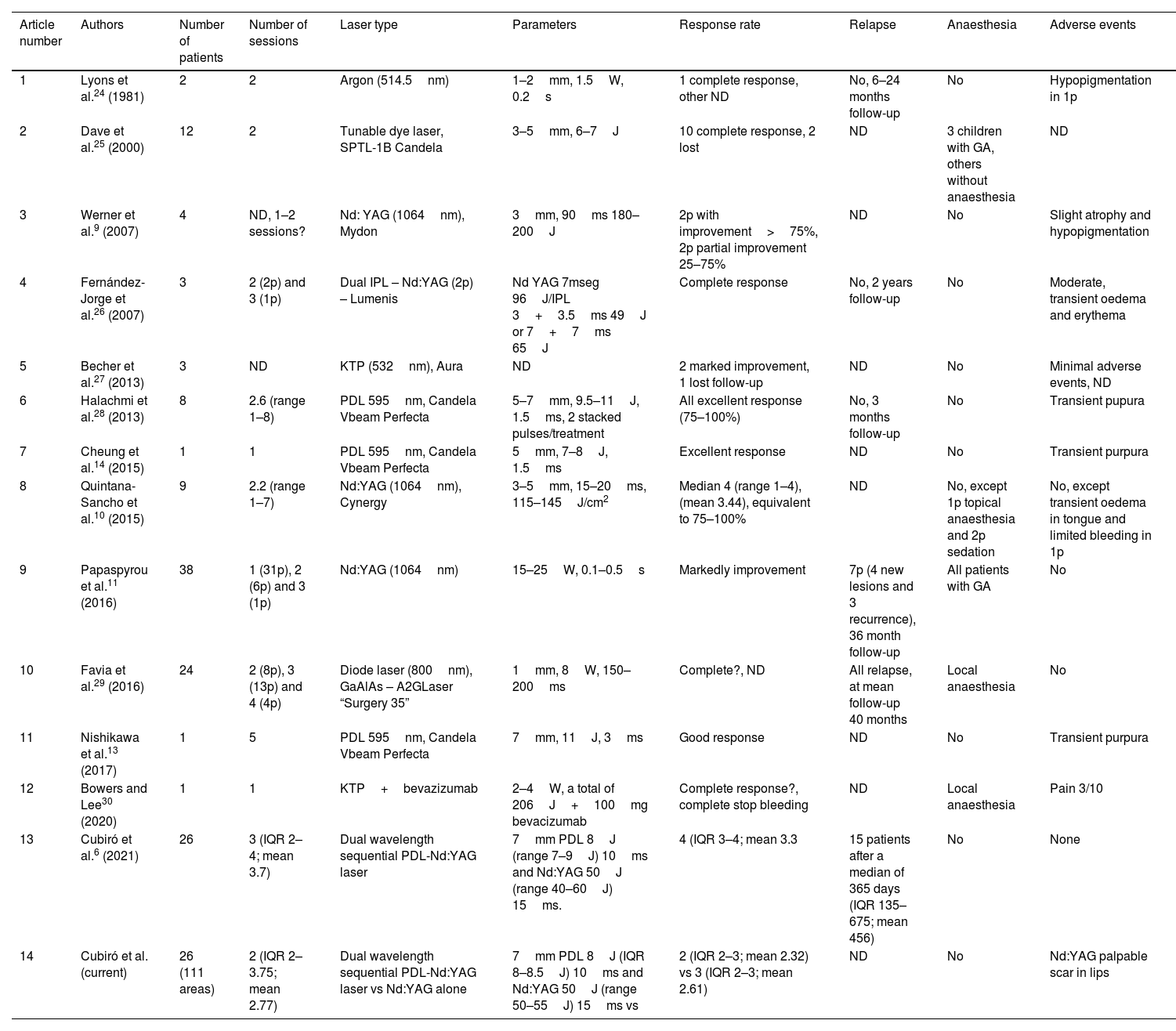
Even though DWSL seemed to be a good candidate according to the available evidence,6 in our study the Nd:YAG laser had better response rates, together with better tolerability (less pain) and slightly lower safety (more side effects as scarring, oedema, etc.). Our patients severity improved from a median of 2 in Nd:YAG subgroup to a median of 0, compared to the improvement of 2 to 1 in DWSL group respectively, after a median number of 2 sessions at the endpoint. Our responses with Nd:YAG laser may be comparable to those in available studies9–11 (Table 5), even though the evaluation criteria differ, limiting their comparison. However, the responses to DWSL in our study were lower compared to published evidence with the same evaluation criteria.6 This might be explained by the lower number of sessions, with similar fluences, in our study compared to previous publications (mean number of sessions, 2.77 vs 3.73).6 As previously reported,12 less sessions may decrease the response scores, which may explain our results. In the current study, differences in response between DWSL and Nd:YAG may be accounted on lower fluences of Nd:YAG in DWSL compared to Nd:YAG alone (52.31J vs 156.54J). Despite the theoretic proposal that methemoglobin would increase the absorbance of Nd:YAG, this effect might be insufficient to account for such a fluence difference. In our opinion, Nd:YAG would be the main player of DWSL in treating the thicker lesions of HHT patients. Published pictures from patients treated with Nd:YAG alone9–11 suggest their lesions are thicker than those of patients treated with PDL.13,14 Consequently, lower fluences of Nd:YAG in DWSL may have a lower overall efficacy, even though the responses achieved would be considered satisfactory. Comparisons with the published reports on other laser modalities (Table 5) are not possible due to different evaluation criteria.
Details of previously published series on laser treatment of cutaneous lesions in Hereditary Haemorrhagic Telangiectasia.
| Article number | Authors | Number of patients | Number of sessions | Laser type | Parameters | Response rate | Relapse | Anaesthesia | Adverse events |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Lyons et al.24 (1981) | 2 | 2 | Argon (514.5nm) | 1–2mm, 1.5W, 0.2s | 1 complete response, other ND | No, 6–24 months follow-up | No | Hypopigmentation in 1p |
| 2 | Dave et al.25 (2000) | 12 | 2 | Tunable dye laser, SPTL-1B Candela | 3–5mm, 6–7J | 10 complete response, 2 lost | ND | 3 children with GA, others without anaesthesia | ND |
| 3 | Werner et al.9 (2007) | 4 | ND, 1–2 sessions? | Nd: YAG (1064nm), Mydon | 3mm, 90ms 180–200J | 2p with improvement>75%, 2p partial improvement 25–75% | ND | No | Slight atrophy and hypopigmentation |
| 4 | Fernández-Jorge et al.26 (2007) | 3 | 2 (2p) and 3 (1p) | Dual IPL – Nd:YAG (2p) – Lumenis | Nd YAG 7mseg 96J/IPL 3+3.5ms 49J or 7+7ms 65J | Complete response | No, 2 years follow-up | No | Moderate, transient oedema and erythema |
| 5 | Becher et al.27 (2013) | 3 | ND | KTP (532nm), Aura | ND | 2 marked improvement, 1 lost follow-up | ND | No | Minimal adverse events, ND |
| 6 | Halachmi et al.28 (2013) | 8 | 2.6 (range 1–8) | PDL 595nm, Candela Vbeam Perfecta | 5–7mm, 9.5–11J, 1.5ms, 2 stacked pulses/treatment | All excellent response (75–100%) | No, 3 months follow-up | No | Transient pupura |
| 7 | Cheung et al.14 (2015) | 1 | 1 | PDL 595nm, Candela Vbeam Perfecta | 5mm, 7–8J, 1.5ms | Excellent response | ND | No | Transient purpura |
| 8 | Quintana-Sancho et al.10 (2015) | 9 | 2.2 (range 1–7) | Nd:YAG (1064nm), Cynergy | 3–5mm, 15–20ms, 115–145J/cm2 | Median 4 (range 1–4), (mean 3.44), equivalent to 75–100% | ND | No, except 1p topical anaesthesia and 2p sedation | No, except transient oedema in tongue and limited bleeding in 1p |
| 9 | Papaspyrou et al.11 (2016) | 38 | 1 (31p), 2 (6p) and 3 (1p) | Nd:YAG (1064nm) | 15–25W, 0.1–0.5s | Markedly improvement | 7p (4 new lesions and 3 recurrence), 36 month follow-up | All patients with GA | No |
| 10 | Favia et al.29 (2016) | 24 | 2 (8p), 3 (13p) and 4 (4p) | Diode laser (800nm), GaAlAs – A2GLaser “Surgery 35” | 1mm, 8W, 150–200ms | Complete?, ND | All relapse, at mean follow-up 40 months | Local anaesthesia | No |
| 11 | Nishikawa et al.13 (2017) | 1 | 5 | PDL 595nm, Candela Vbeam Perfecta | 7mm, 11J, 3ms | Good response | ND | No | Transient purpura |
| 12 | Bowers and Lee30 (2020) | 1 | 1 | KTP+bevazizumab | 2–4W, a total of 206J+100mg bevacizumab | Complete response?, complete stop bleeding | ND | Local anaesthesia | Pain 3/10 |
| 13 | Cubiró et al.6 (2021) | 26 | 3 (IQR 2–4; mean 3.7) | Dual wavelength sequential PDL-Nd:YAG laser | 7mm PDL 8J (range 7–9J) 10ms and Nd:YAG 50J (range 40–60J) 15ms. | 4 (IQR 3–4; mean 3.3 | 15 patients after a median of 365 days (IQR 135–675; mean 456) | No | None |
| 14 | Cubiró et al. (current) | 26 (111 areas) | 2 (IQR 2–3.75; mean 2.77) | Dual wavelength sequential PDL-Nd:YAG laser vs Nd:YAG alone | 7mm PDL 8J (IQR 8–8.5J) 10ms and Nd:YAG 50J (range 50–55J) 15ms vs | 2 (IQR 2–3; mean 2.32) vs 3 (IQR 2–3; mean 2.61) | ND | No | Nd:YAG palpable scar in lips |
Abbreviations: p: patient; ms: millisecond; DWSL: dual wavelength sequential PDL-Nd:YAG laser; Nd:YAG: neodymium-doped: yttrium-aluminium-garnet; PDL: pulsed dye laser; IPL: intense pulsed light; KTP: potassium-titanyl-phosphate; GA: general anaesthesia; ND: not described.
As regards tolerability, pain NSR was lower with Nd:YAG (mean 4.86 vs 5.65, p=0.046). Data from published studies is inconsistent: some authors found no differences in pain,15,16 others reported more pain with Nd:YAG17 and others more with PDL alone.18 In our experience, tolerance to DWSL may be affected by the sequential two laser shots compared with just one shot in Nd:YAG.18 By topographic regions, treatment of hand lesions was the most painful (p=0.054). Differences in referred pain may be explained by differences in nociception, since pain sensitivity is higher in glabrous skin.19
Overall, no severe adverse events were reported by our patients in either group. Crusting or oedema were less severe and frequent on the face. According to our results a lower risk of scarring might be expected with DWSL, but even in the Nd:YAG group only one patient (patient 2) had a small slightly visible palpable scar. This is consistent with a higher risk of tissue damage caused by photothermolysis when higher fluences of the Nd:YAG laser are used alone, which can lead to scar formation.
Impairment of QoL in HHT patients, in most cases related to epistaxis, is occasionally reported in the literature.16,20–22 In the current study, the effects of each laser treatment on QoL were not compared due to difficulty in discerning effects on QoL for each laser subtype (and body side). Considering the Skindex-29 cut-offs described by Prinsen et al.,23 our HHT patients would be considered as having mild to moderate QoL impairment. However, there is no currently standard approach defined to evaluate Skindex-29.23 On the other hand, FACE-Q® test obtained high values at the beginning of the study which confirm the high aesthetic impact and psychological distress that HHT patients suffer, mainly when the face is affected, as specifically assessed by FACE-Q® test. Differences from baseline to the end of the study were found to be statistically significant for tests, which proves that laser therapy can improve the QoL impairment of HHT patients. Probably, this improvement is related not just to the benefit on general aesthetics and physical appearance, but also to the decreased frequency and intensity – and even disappearance – of bleeding of mucocutaneous telangiectases, as reported by patients. This might also partially account for the high satisfaction rates in our study.
Our study has some strengths and limitations that should be mentioned. This is the first randomized double-blinded study including QoL assessment on laser therapy of telangiectases in HHT patients. The low prevalence of HHT and the concurrent COVID-19 pandemic explained the small number of patients recruited and limited their follow-up.
ConclusionsBoth DSWL and Nd:YAG are safe, effective and satisfactory treatment options for treating mucocutaneous telangiectases in HHT patients. However, Nd:YAG provided better results with better tolerability, but a slightly lower safety profile in our study. Satisfaction rates were high and improvement in QoL significant with both laser modalities.
Conflict of interestThe authors declare that they have no conflict of interest.