The infraorbital region is a unique anatomic subunit, close to structures of functional and esthetic importance, such as the lower eyelid, nasal ala and oral commissure, which should be taken into consideration during reconstructive surgery. The main cause of distortion is traction secondary to closure with excessive tension or to scar contraction. The absence of folds in which to hide scars is an added difficulty.1
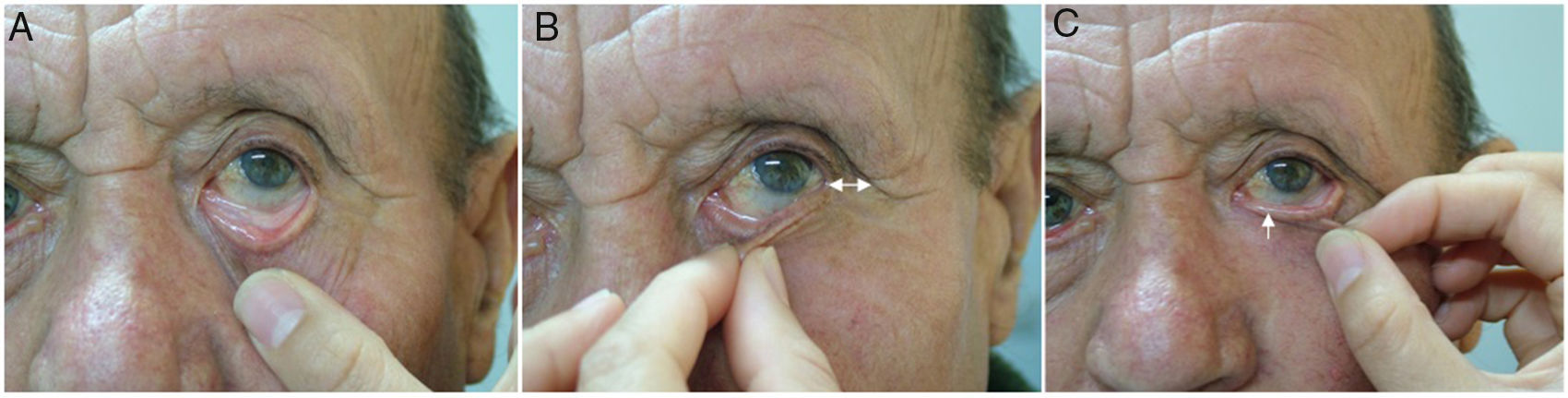
One of the principal complications when reconstructing infraorbital defects is postoperative ectropion. A thorough examination of the eyelid prior to surgery is therefore required to identify signs of excessive laxity (Fig. 1). In the event of muscle wasting that may favor ectropion, the need for an associated eyelid-suspension technique (e.g., canthopexy associated with the flap chosen to close the defect) should be considered.
The Mutaf triangular flap technique was described in 2011 by Mutaf et al.2 for the reconstruction of infraorbital defects. It is based on 2 triangular transposition flaps treated as an unequal Z-plasty.
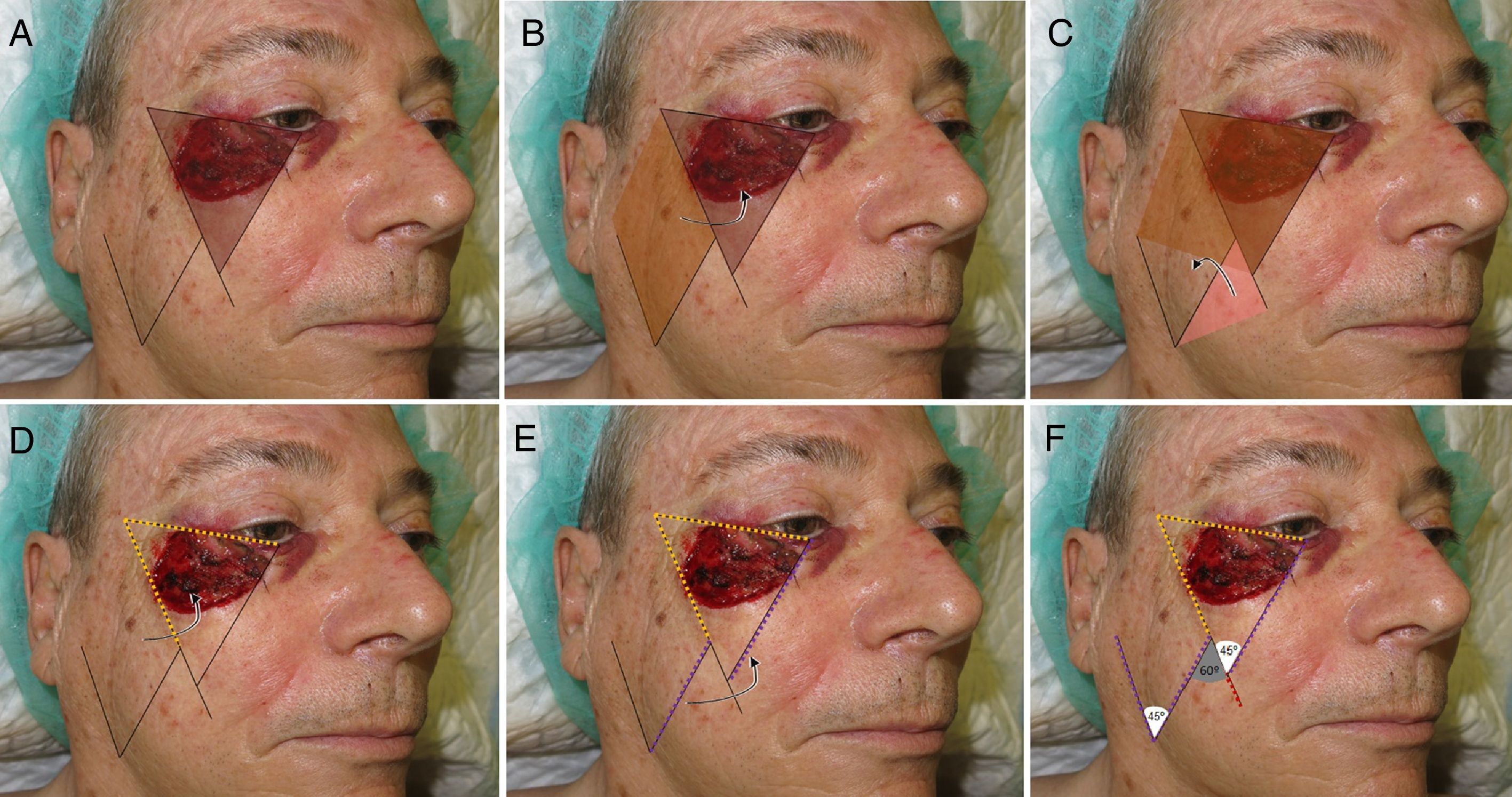
Technical DescriptionThe technique requires converting the surgical defect into an isosceles triangle with the base superior (Fig. 2A). Based on this triangle and its dimensions, 2 opposing triangles are then traced (Fig. 2D-F). One triangle is transposed to cover the original defect and the second triangle will cover the defect of the donor region (Fig. 2B and C). The suture line and, therefore, the resulting scar will follow the tension lines of the cheek.2,3
Design of the Mutaf triangular flap. A, Conversion of the primary defect into a triangle. B, Rotation of the second triangle required to cover the primary defect (arrow). C. Rotation of the third triangle required to cover the secondary defect (arrow). D, The first part of the flap is traced at the same distance as the upper line of the defect converted to a triangle (yellow dotted line). E, The length of the flap must be the same as that of the internal face of the defect (purple dotted line) it will be moved toward (arrow). F, Extension of the vertex of the defect to define the third triangle (red dotted line). Angles of the vertices of the 3 triangles.
We report our experience in performing the Mutaf flap in a patient with a large defect in the palpebromalar region following Mohs surgery for basal cell carcinoma (see video).
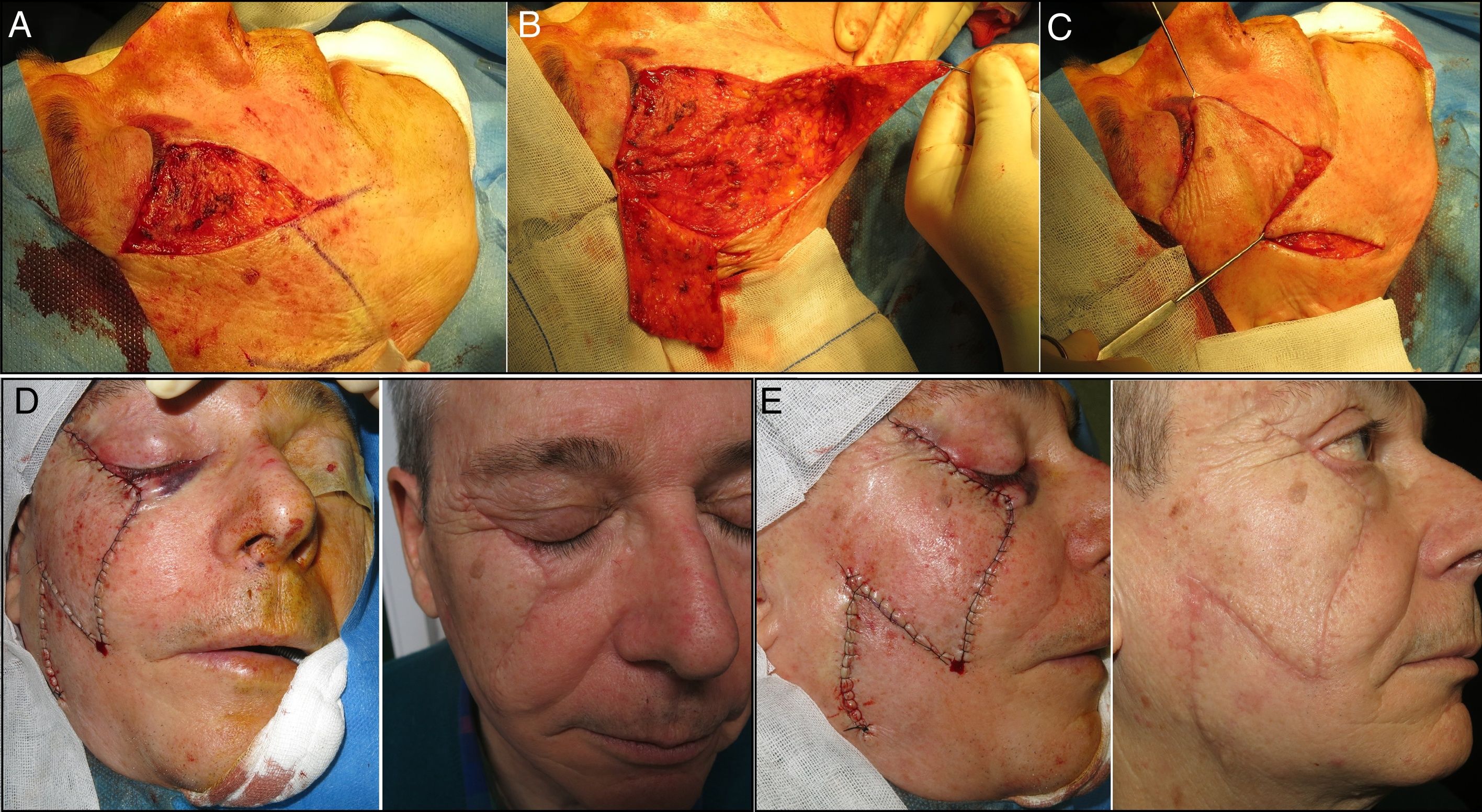
The patient was placed under general anesthesia and we began the incision and dissection of the tissue to convert the primary defect into a triangle. When this triangle had been defined, the first part of the flap was incised and the flap was dissected superficially in a subcutaneous plane. The second triangle was then raised and the final positioning of both flaps was verified (Fig. 3A-C).
Before commencing suturing, careful hemostasis was performed, the uppermost part of the flap was thinned to ensure it was as similar as possible to the palpebral skin, and the lateral orbital edge was attached by means of an anchor stitch using a 3-0 absorbable braided suture (Vicryl®) to prevent retraction. Finally, continuous suture of the flap was performed using 4-0 silk and the dog-ears at the distal end were corrected (Fig. 3D and E).
IndicationMedium and large infraorbital skin defects, for which other, simpler, reconstructive techniques are scheduled may give rise to postoperative ectropion or poor esthetic results.
ContraindicationsNo absolute contraindications are known. Abnormal coagulation and factors that predispose the patient to cutaneous ischemia (smoking, prior radiation therapy, diabetic foot, etc.), which may compromise the viability of the flap, may be considered relative contraindications.
Complications- •
Surgical wound infection.
- •
Hemorrhage, hematoma, and skin necrosis.
- •
Scarring ectropion.
- •
Temporary or permanent altered sensation owing to damage to nerve structures.
The Mutaf triangular flap technique is a good, original reconstructive option in medium and large infraorbital defects, where, owing to the risk of palpebral retraction, other flap techniques do not provide an adequate alternative and the use of grafts may compromise the esthetic results. The operation is laborious but not technically complex and, as can be seen, provides good functional and esthetic results (Figs. 3D and E). Appropriate examination of palpebral laxity is required before designing surgery of the infraorbital region.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández Canga P, Varas Meis E, Castiñeiras González J, Espasandín Arias M, Rodríguez Prieto MÁ. Reconstrucción palpebral inferior mediante «colgajo triangular de Mutaf». Actas Dermosifiliogr. 2018;109:917–919.