A 77-year-old man sought care for recurrent episodes of swelling in the right malar region that in the previous 5 months had spread to the neck, the left malar region, both nasolabial folds, and the right infraorbital rim. The patient reported only a sensation of tautness in the affected areas.
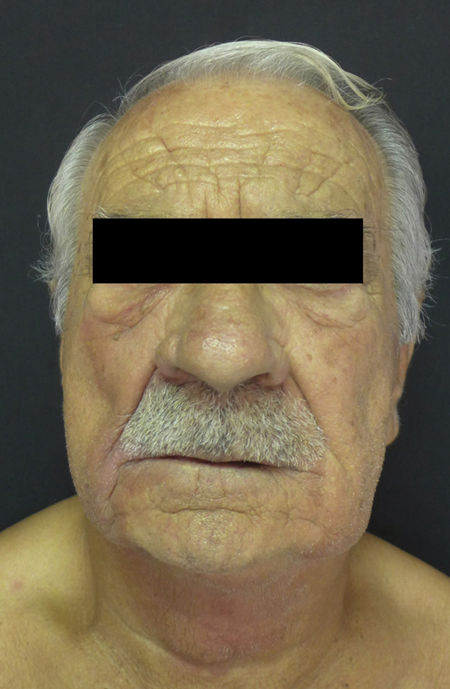
Physical ExaminationPhysical examination revealed violaceous coloring and palpable infiltration in the aforementioned regions (Fig. 1). No macroglossia or lesions in the oral cavity were observed.
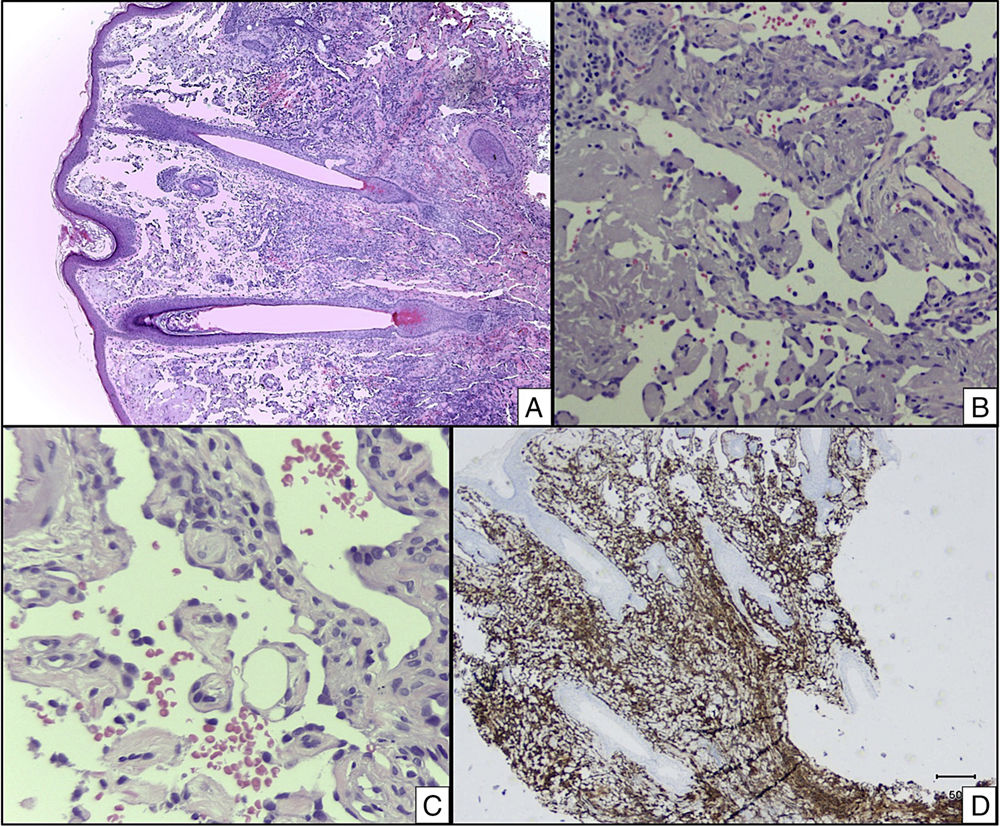
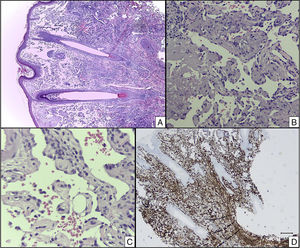
Additional ExaminationsA 4-mm punch biopsy specimen was taken from one of the lesions and histopathologic examination revealed the presence of multiple irregular dilated vascular channels joined by anastomosis, some lined with mildly atypical endothelial cells, situated among the dermal collagen bundles and around the pilosebaceous follicles. Immunohistochemistry showed CD34+and CD31+cells lining the vascular channels (Fig. 2).
What Is Your Diagnosis?
DiagnosisCutaneous angiosarcoma of the head and neck.
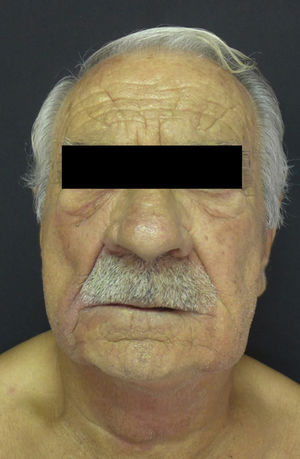
Clinical CourseComputed tomography of the neck, chest, abdomen, and pelvis was carried out to determine the extent of disease; no distant metastases were detected. Histologic mapping of the affected regions confirmed that the angiosarcoma was locally advanced. Palliative treatment was started with paclitaxel and propranolol as adjuvant therapy. Based on the local progression of the lesions (Fig. 3) with mandibular involvement despite treatment, radiation therapy was initiated. At present, the patient is waiting to begin treatment with pazopanib.
DiscussionCutaneous angiosarcoma is a rare, aggressive, malignant vascular sarcoma that occurs most frequently in elderly men, affecting the head and neck. It can also appear on the limbs of patients with chronic lymphedema or in areas exposed to radiation therapy.1
Although cutaneous angiosarcoma tends to manifest as nodules, plaques, or erythematous or violaceous macules, its great clinical variability often leads to late diagnosis. Tay and Ong2 reported a case similar to that of our patient. Their patient had an angiosarcoma of the head and neck that mimicked episodes of edema or facial swelling; diagnosis was delayed after the lesion responded partially to corticosteroid treatment. The head-tilt examination maneuver, in which the patient is asked to place his or her head below the level of the heart for 5-10seconds, can be used to increase the congestion of the neoplastic vessels, thus making the lesion more clinically apparent.3
A pathologic examination like that described in our case, plus the detection of CD34+and CD31+neoplastic cells, allow this entity to be diagnosed. Clinical differential diagnosis should include hematomas, vascular tumors such as hemangioma and Kaposi sarcoma, cutaneous lymphomas and pseudolymphomas, cutaneous metastases, lupus pernio, and other skin tumors such as melanoma, Merkel cell carcinoma, and angiomatoid fibrous histiocytoma.4
The treatment of choice for localized disease is radical surgery, which, if performed early and followed by adjuvant radiation therapy, is the only potentially curative treatment. However, when the tumor is unresectable and/or metastatic disease is present, the prognosis worsens considerably; chemotherapy is the treatment of choice in such cases.1 Radiation therapy can also be used to achieve good local tumor control in cases of metastatic or unresectable disease.5 A recent case report suggests that treatment with oral propranolol is effective for reducing the size of angiosarcomas,6 although in our case it was difficult to assess the response to this treatment because the patient had already started treatment with paclitaxel.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sabater Abad J, Lloret Ruiz C, Quecedo Estébanez E. Edema facial recurrente. Actas Dermosifiliogr. 2019;110:e3–e4.