Absorption of topical products through the epidermis is limited by the skin's barrier function. Numerous techniques and agents such as microneedling, dermabrasion, radiofrequency, and lasers have been used to increase penetration within an approach known as transdermal drug delivery. One of these techniques is laser-assisted drug delivery (LADD), which often uses ablative fractional lasers (CO2 or erbium:YAG lasers) because of their capacity to produce microscopic ablated channels. The parameters in LADD need to be adjusted to the patient, the skin condition and its location, and the drug. LADD has been used with various topical products, such as corticosteroids, photosensitizers, and immunotherapy agents (imiquimod or 5-fluorouracil) to treat numerous conditions, including scars, nonmelanoma skin cancer, and photodamage. LADD is a promising technique that enhances the absorption of topical molecules while adding the synergic effect of the laser.
La absorción de productos tópicos a través de la epidermis está limitada por la función de barrera cutánea. Existen distintas técnicas, tales como el microneedling, la dermoabrasión, la radiofrecuencia o los láseres, que se han empleado para aumentar la absorción de estas sustancias en una estrategia conocida como vehiculización transdérmica de fármacos. Entre estas técnicas destaca la vehiculización de fármacos asistida por láseres (VFAL), especialmente láseres fraccionales ablativos (CO2/Er:YAG), por su capacidad de generar canales de microablación. En la VFAL se deben ajustar los parámetros en función del tipo de paciente, la dermatosis, la localización y el fármaco empleado. Se ha estudiado la VFAL en el uso de corticoides, fotosensibilizantes o inmunoterapia tópica (imiquimod o 5-fluorouracilo), entre otros, y en múltiples indicaciones: cicatrices, cáncer cutáneo no melanoma, fotodaño, etc. La VFAL es una técnica prometedora que permite aumentar la absorción de moléculas tópicas consiguiendo, además, el efecto sinérgico del láser.
One of the most typical parts of the dermatologist's work is that of prescribing topical treatments to induce a local effect against a skin disease. However, absorption of these agents is limited by the skin's main function as a barrier to the external environment. Given its composition and location as the outermost layer, the stratum corneum is the key player in this defense function.1
It is estimated that around 1%-5% of topical preparations cross an intact epidermis.2 The epidermis can be crossed via 3 pathways: (1) the intercellular pathway, through which the most lipophilic substances are absorbed via the desmosomes in the spaces between cells; 2) the transcellular pathway, across the aqueous pores of the keratinocytes; and 3) the transappendageal pathway, which is mainly across hair follicles and, to a lesser extent, acrosyringea.3
We must also take account of the intrinsic properties of the drug that directly affect absorption. According to the Fick laws of diffusion, the flux of absorption is determined not only by differences in the concentration of drug absorbed between the external environment and the dermis, but also by the solubility and diffusion coefficient of the drug. The heaviest molecules, ie, those with the highest molecular weight, diffuse more slowly than smaller or neutral molecules. Lipophilic and hydrophobic substances make their way across the dermis more quickly.4
Topical drugs can be more easily absorbed by means of physical methods in what is known as transdermal delivery. One of the main methods involves lasers, which have led to exponential growth in the use of the technique known as laser-assisted drug delivery (LADD).1
Transdermal Drug DeliveryTransdermal drug delivery involves assisted transport of substances across the epidermis using various physical methods. This promising method of drug delivery to the body makes it possible to increase the absorption achieved with respect to topical delivery. In addition, oral delivery often entails problems of real bioavailability owing to the first-pass effect and may be limited by the greater risk of adverse effects. Studies on transdermal drug delivery have investigated scraping, dermabrasion, microneedling, pressure waves, vacuum effect, and lasers. These modalities have been used to delivery various types of drugs and substances, such as triamcinolone, methyl aminolevulinic acid (MAL), 5-fluorouracil, and methotrexate.5–11
Few studies have compared the efficacy of the various techniques available. One well-designed study compared the efficacy of topical MAL with that of photodynamic therapy (PDT) after application of MAL in addition to various physical methods, such as ablative fractional laser (AFL), nonablative fractional laser (NAFL), curettage, dermabrasion, and microneedling.12 The authors concluded that there were no differences in the formation of protoporphyrin ix after application of MAL alone or in combination with NAFL. However, the remaining techniques did prove superior with respect to formation of protoporphyrin ix. The most effective of all was AFL. These results have been confirmed, at least partially, by subsequent studies; therefore, AFLs are currently considered the most effective drug delivery technique.13,14
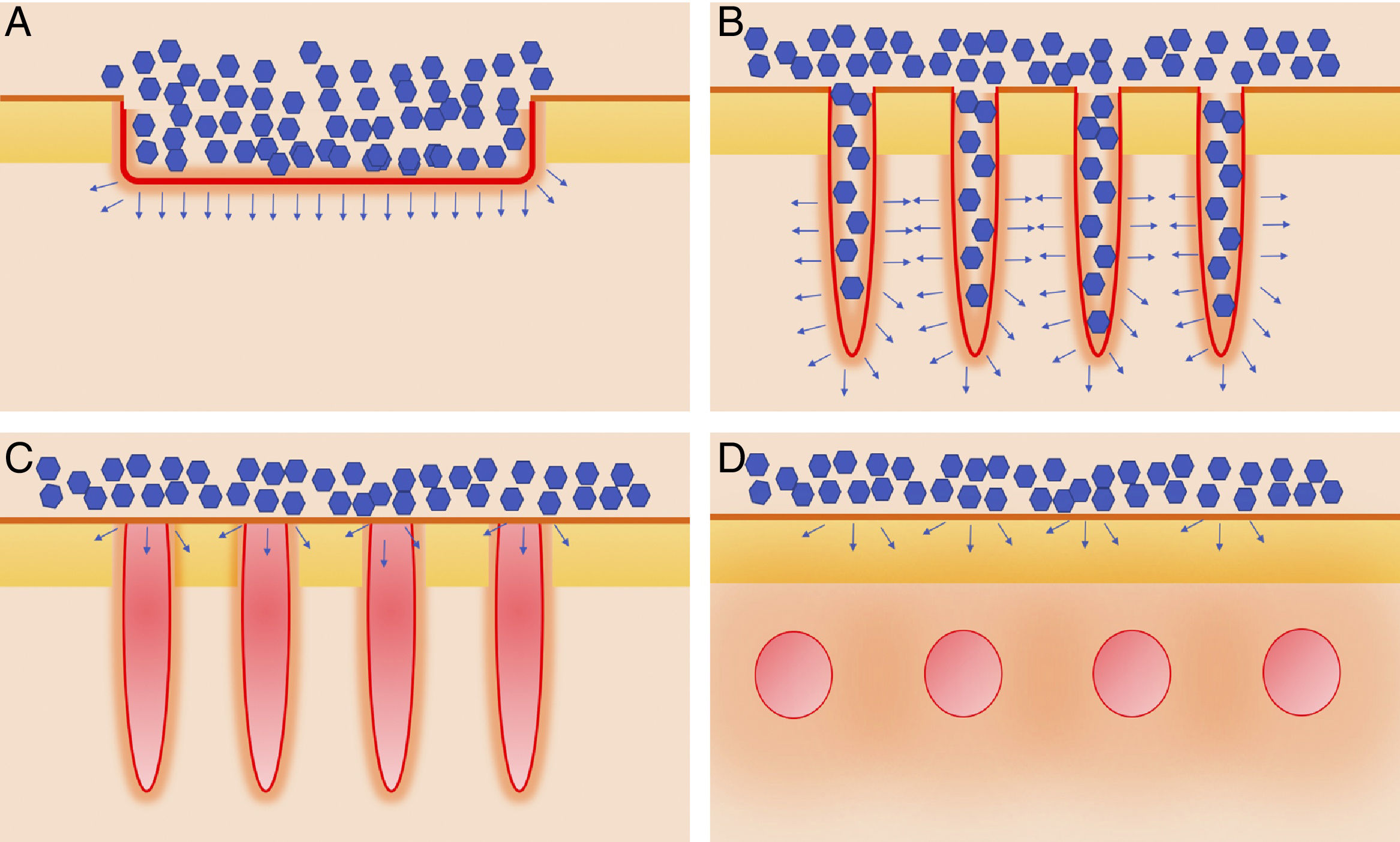
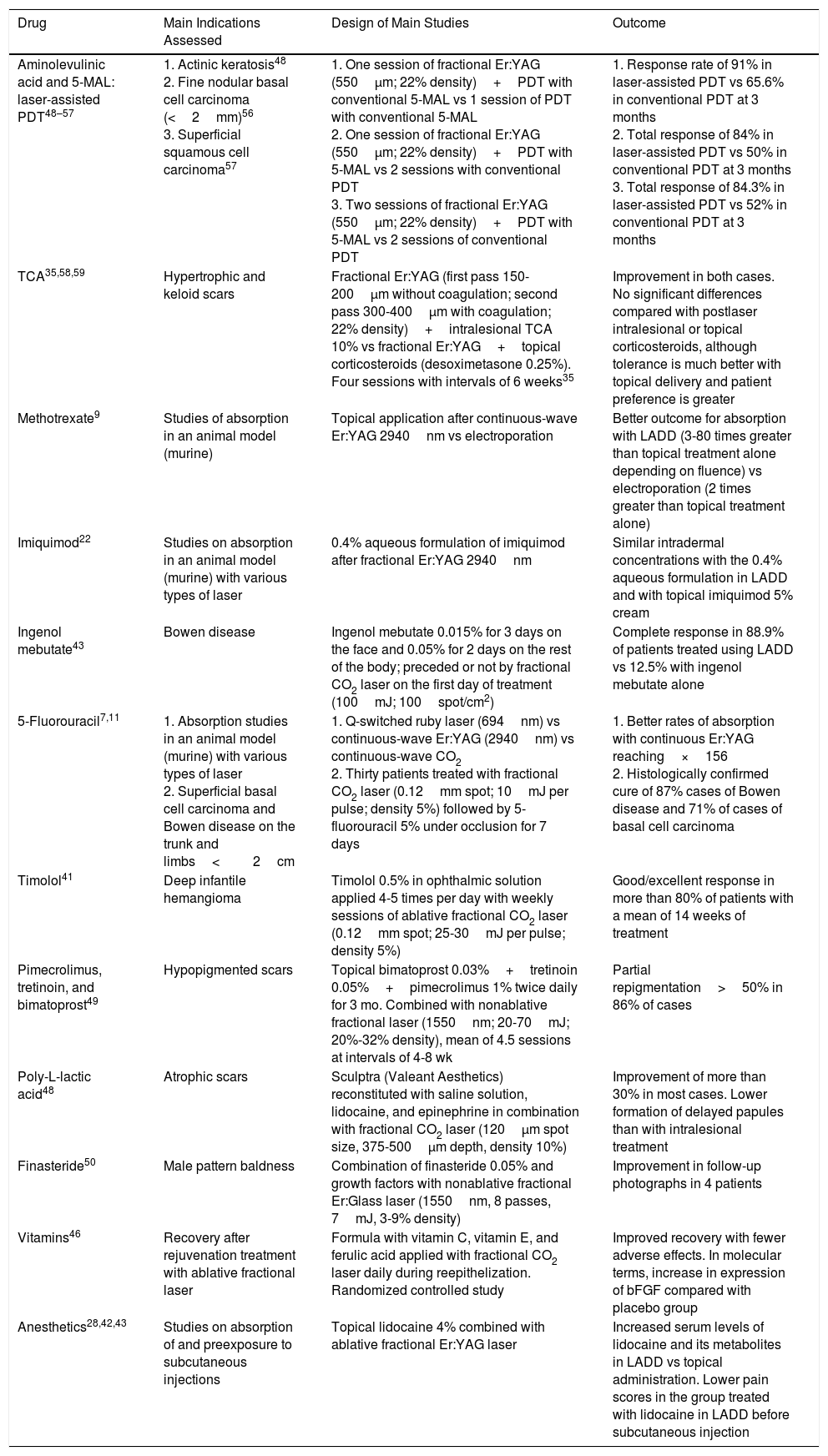
Laser-Assisted Drug Delivery: General ConsiderationsLasersDifferent types of laser have been used for LADD. Each type is more or less effective, although it is also important to know the individual safety profile. In practical terms, we can divide the lasers used in LADD into 4 groups: (1) Fully ablative lasers, such as the carbon dioxide (CO2) laser (10 600nm) or the erbium-doped yttrium aluminum garnet (Er:YAG) laser (2940nm), whose main chromophore is water and which lead to heating and total vaporization of the skin; (2) AFLs, which are the same as the previous group, although when used fractionally, they lead to columns of thermal injury, which are microscopic treatment zones (MTZs); (3) NAFL, which are similar to the previous group and include lasers such as the erbium fiber laser (1550nm). These also produce MTZs, although in the columns, only heating of the skin is observed, with no ablation of the dermal-epidermal junction; and (4) Nonablative dermal remodelling lasers. This group includes all lasers with chromophores other than water but which have been used to induce greater drug absorption. They also include lasers for the treatment of vascular anomalies, such as the 585/595-nm pulsed dye laser or the neodymium-doped YAG laser (1064nm).15 The characteristics of AFL have led it to be the most widely studied in LADD, followed by NAFL (Fig. 1).
Various types of laser used in laser-assisted drug delivery. A, Fully ablative lasers, mainly CO2 (10 600nm) and Er:YAG (2940nm). These perform full, not fractional ablation, of the epidermis, thus enabling the drug to reach the dermis. B, Ablative fractional lasers. These are a fractional version of the ablative lasers described in A. They generate microscopic ablation channels through which the drugs reach the dermis. C, Nonablative fractional lasers, such as Er:Glass 1550nm, which generate microscopic columns of coagulated tissue without ablating the epidermis. D, Nonablative dermal remodelling. This subtype includes all those lasers with chromophores other than water, which deposit energy in the area of the chromophore, generally in the dermis, as, for example, with lasers used to treat vascular anomalies, such as the 585/595-nm pulsed dye laser or Nd:YAG (1064nm). gr1.
While the risk of adverse effects such as erythema, vesiculation, crusting, or even scarring are lower with fractional lasers than with conventional ablative lasers, these effects may appear when high fluences and densities are applied.16–18 If AFLs are used for LADD, the settings must be optimized to achieve the best results possible with the minimum risk.
The density of fractional lasers refers to the amount of tissue covered by the MTZs. The total density depends on both the number of channels and on the size of the laser beam. Initial studies with MAL, which were subsequently corroborated with other agents (diclofenac, tretinoin), showed that the concentrations of the product in skin increased with increases in density up to a maximum of 5%, at which point the concentrations stabilized.19–22 Thus, densities higher than 5% in treatment with AFL carry no clear benefits but do carry a greater risk of adverse events.
Another key parameter is the depth of the channel itself, which depends directly on laser fluence. As a general rule, we should apply higher fluences in order to reach the deeper layers of the dermis if we wish to treat conditions such as alopecia or scarring. The most superficial layers of the dermis would be appropriate for treatment of photodamage, melasma, or superficial scarring. In patients with melasma, vitiligo, or superficial nonmelanoma skin cancer, ablation restricted to the epidermis could be sufficient.23
In the case of AFLs, drug absorption is affected by the coagulation zone (CZ) surrounding the channels, as well as by total ablation depth. The area of the CZ ranges from around 50mm to 150mm, depending on fluence and, in particular, laser wavelength, and is greater for CO2 lasers (10 600nm) than for Er:YAG lasers (2940nm).24,25 The greater affinity of Er:YAG for water leads to “purer” ablation, with almost no heat given off around the MTZs, whereas in the case of CO2, a wider CZ is generated owing to the reduced affinity for water. The presence of CZs implies even greater absorption of the drug delivered across the channels, thus also explaining the superiority of AFL over modalities that do not involve the generation of heat around the channels, as is the case in microneedling.12 However, it is important to remember that the presence of CZs only reflects transmission of heat to the surrounding dermis, which may be associated with undesirable local reactions.26
Drugs and Application TechniquesGiven that lipophilic substances have a greater intrinsic ability to cross an intact epidermis, the more marked effect of LADD is observed with hydrophilic substances.4 Other relevant factors that affect absorption include the vehicle used, the type of preparation, and the presence of additives or excipients. Liquid and gel formulations cross the channels produced by AFL with greater affinity than more oily formulations in the form of creams or ointments.27 This observation should be taken into account owing to the greater efficacy and the greater risk of adverse effects when these formulations are used.4
There is also some disparity between hydrophobic and hydrophilic substances and their association with penetration via the laser channels. In the case of hydrophilic substances, such as 5-fluorouracil or methotrexate, greater absorption has been detected in direct relation to AFL fluence and, therefore, the depth of the channels. However, this finding has not been confirmed in studies with hydrophobic substances such as imiquimod and lidocaine.8,9,23,28
Various considerations must be taken into account with respect to the suitability of applying topical drugs directly to the dermis. First, we must ask whether the substances and excipients we intend to use are suitable for subcutaneous application. Local hypersensitivity has been reported with the application of vitamin C serum delivered via microneedling, which led to the formation of histologically confirmed granulomas or even systemic hypersensitivity reactions.29 Under ideal conditions, we would use only highly sterile products, although not all topical products are available as such. AFL itself carries some risk of bacterial infection owing to direct exposure of the dermis, and this risk increases when we apply drugs such as 5-fluorouracil, corticosteroids, and MAL.14,17,30,31 It is important to insist on aseptic conditions for application of LADD procedures.
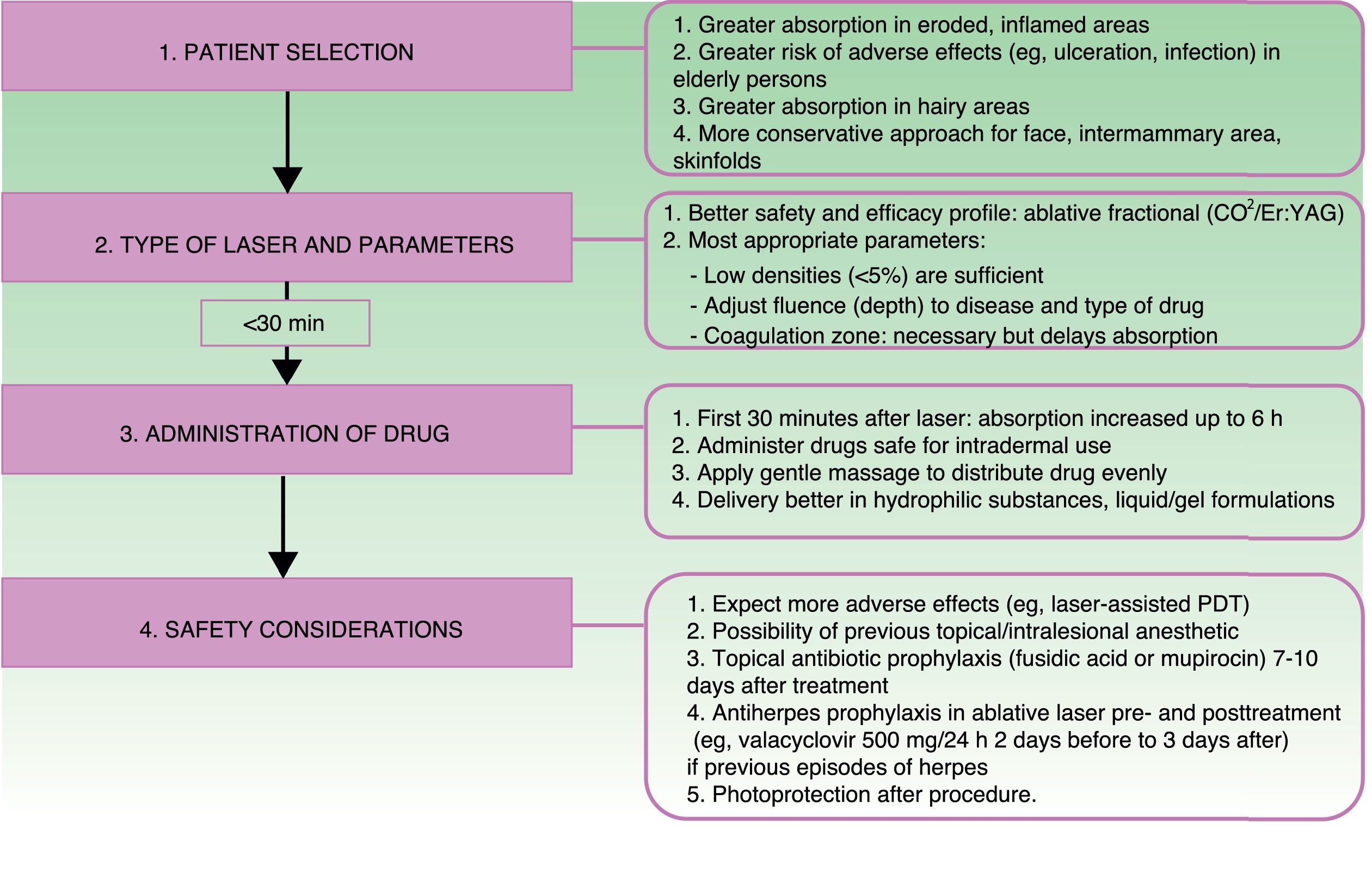
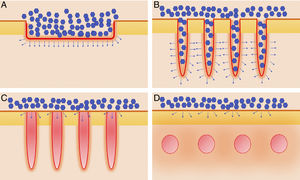
Another key factor in LADD is the interval between use of the laser and application of the product to the skin. It is important to remember that the microscopic channels close with time owing to debris such as fibrin, inflammatory mediators, and keratinocytes.32–34 One study showed that topical application 6hours after use of the laser increases absorption, which is most successful during the first 30minutes. However, no increase in absorption is observed when the product is applied after 24hours.35Figure 2 shows the appropriate steps for LADD and the considerations to be taken into account for each one.
PatientsAs is the case with topical treatments, absorption of drugs using LADD depends on many characteristics that are intrinsic to the patient, the skin disease treated, and the area affected by the disease. Thus, absorption is more potent in cases of inflamed or eroded skin. Similarly, more hydrated skin exhibits greater affinity for the absorption of oily substances. Furthermore, the patient's age is important, given that atrophy, erosion, and ulceration are more likely to affect older people, who are also at greater risk of infection and take longer to recover.36 Therefore, the ideal approach would be to make a correct evaluation of the patient's skin type, since there may be some atrophy due to solar elastosis in patients with low skin types, even younger patients. In such cases, laser fluence should be reduced, and in CO2 AFL devices that allow it, pulses with a lower heat deposit should be administered to prevent pathological scarring. As for location, the drug is absorbed mainly across the transappendageal pathway through the follicles in hairy areas; therefore, the parameters for using LADD should be applied with greater caution.
Laser-Delivered DrugsFor practical purposes, we focus on 2 of the main applications of LADD: delivery of corticosteroids for hypertrophic and keloid scars and laser-assisted PDT.6,37–40 In addition to these 2 indications, numerous drugs have been delivered in many other dermatologic indications.7–9,17,23,28,41–50 Data on these studies are shown in Table 1.
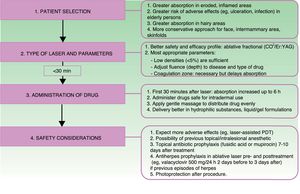
Medications Used in Laser-Assisted Drug Delivery.
| Drug | Main Indications Assessed | Design of Main Studies | Outcome |
|---|---|---|---|
| Aminolevulinic acid and 5-MAL: laser-assisted PDT48–57 | 1. Actinic keratosis48 2. Fine nodular basal cell carcinoma (<2mm)56 3. Superficial squamous cell carcinoma57 | 1. One session of fractional Er:YAG (550μm; 22% density)+PDT with conventional 5-MAL vs 1 session of PDT with conventional 5-MAL 2. One session of fractional Er:YAG (550μm; 22% density)+PDT with 5-MAL vs 2 sessions with conventional PDT 3. Two sessions of fractional Er:YAG (550μm; 22% density)+PDT with 5-MAL vs 2 sessions of conventional PDT | 1. Response rate of 91% in laser-assisted PDT vs 65.6% in conventional PDT at 3 months 2. Total response of 84% in laser-assisted PDT vs 50% in conventional PDT at 3 months 3. Total response of 84.3% in laser-assisted PDT vs 52% in conventional PDT at 3 months |
| TCA35,58,59 | Hypertrophic and keloid scars | Fractional Er:YAG (first pass 150-200μm without coagulation; second pass 300-400μm with coagulation; 22% density)+intralesional TCA 10% vs fractional Er:YAG+topical corticosteroids (desoximetasone 0.25%). Four sessions with intervals of 6 weeks35 | Improvement in both cases. No significant differences compared with postlaser intralesional or topical corticosteroids, although tolerance is much better with topical delivery and patient preference is greater |
| Methotrexate9 | Studies of absorption in an animal model (murine) | Topical application after continuous-wave Er:YAG 2940nm vs electroporation | Better outcome for absorption with LADD (3-80 times greater than topical treatment alone depending on fluence) vs electroporation (2 times greater than topical treatment alone) |
| Imiquimod22 | Studies on absorption in an animal model (murine) with various types of laser | 0.4% aqueous formulation of imiquimod after fractional Er:YAG 2940nm | Similar intradermal concentrations with the 0.4% aqueous formulation in LADD and with topical imiquimod 5% cream |
| Ingenol mebutate43 | Bowen disease | Ingenol mebutate 0.015% for 3 days on the face and 0.05% for 2 days on the rest of the body; preceded or not by fractional CO2 laser on the first day of treatment (100mJ; 100spot/cm2) | Complete response in 88.9% of patients treated using LADD vs 12.5% with ingenol mebutate alone |
| 5-Fluorouracil7,11 | 1. Absorption studies in an animal model (murine) with various types of laser 2. Superficial basal cell carcinoma and Bowen disease on the trunk and limbs<2cm | 1. Q-switched ruby laser (694nm) vs continuous-wave Er:YAG (2940nm) vs continuous-wave CO2 2. Thirty patients treated with fractional CO2 laser (0.12mm spot; 10mJ per pulse; density 5%) followed by 5-fluorouracil 5% under occlusion for 7 days | 1. Better rates of absorption with continuous Er:YAG reaching×156 2. Histologically confirmed cure of 87% cases of Bowen disease and 71% of cases of basal cell carcinoma |
| Timolol41 | Deep infantile hemangioma | Timolol 0.5% in ophthalmic solution applied 4-5 times per day with weekly sessions of ablative fractional CO2 laser (0.12mm spot; 25-30mJ per pulse; density 5%) | Good/excellent response in more than 80% of patients with a mean of 14 weeks of treatment |
| Pimecrolimus, tretinoin, and bimatoprost49 | Hypopigmented scars | Topical bimatoprost 0.03%+tretinoin 0.05%+pimecrolimus 1% twice daily for 3 mo. Combined with nonablative fractional laser (1550nm; 20-70mJ; 20%-32% density), mean of 4.5 sessions at intervals of 4-8 wk | Partial repigmentation>50% in 86% of cases |
| Poly-L-lactic acid48 | Atrophic scars | Sculptra (Valeant Aesthetics) reconstituted with saline solution, lidocaine, and epinephrine in combination with fractional CO2 laser (120μm spot size, 375-500μm depth, density 10%) | Improvement of more than 30% in most cases. Lower formation of delayed papules than with intralesional treatment |
| Finasteride50 | Male pattern baldness | Combination of finasteride 0.05% and growth factors with nonablative fractional Er:Glass laser (1550nm, 8 passes, 7mJ, 3-9% density) | Improvement in follow-up photographs in 4 patients |
| Vitamins46 | Recovery after rejuvenation treatment with ablative fractional laser | Formula with vitamin C, vitamin E, and ferulic acid applied with fractional CO2 laser daily during reepithelization. Randomized controlled study | Improved recovery with fewer adverse effects. In molecular terms, increase in expression of bFGF compared with placebo group |
| Anesthetics28,42,43 | Studies on absorption of and preexposure to subcutaneous injections | Topical lidocaine 4% combined with ablative fractional Er:YAG laser | Increased serum levels of lidocaine and its metabolites in LADD vs topical administration. Lower pain scores in the group treated with lidocaine in LADD before subcutaneous injection |
Abbreviations: bFGF, basic fibroblast growth factor; LADD, laser-assisted drug delivery; 5-MAL: methyl 5-aminolevulinate; PDT, photodynamic therapy; TCA, triamcinolone acetonide.
Some studies report enhanced absorption of aminolevulinic acid and methyl 5-aminolevulinate assisted by various types of laser, and there are even studies that use devices such as pulsed dye lasers as light sources. In the present analysis, we are interested in those studies that use lasers to deliver photosensitizers to the dermis and thus ensure greater effectiveness with PDT. Thus, studies of the usefulness of LADD in the context of PDT—both for treatment of actinic keratosis and for superficial basal cell and squamous cell carcinoma—have reported greater rates of effectiveness, but also more adverse effects (eg, crusting, pruritus, pain, and erythema).51–60 Haedersdal et al.56 demonstrated absorption rates for MAL that were 13.8 times greater with continuous-wave Er:YAG and up to 7.3 times greater with the fractional version. Similar results have been reported from animal models based on CO2 lasers.
Hypertrophic Scars: Triamcinolone AcetonideTriamcinolone acetonide (TCA) is one of the most widely used intralesional or subcutaneous corticosteroids in various skin diseases owing to its sustained release. The main adverse effects include atrophy, ecchymosis, telangiectasia, infection, and even ulceration at the injection site.30 Application of this agent using LADD has mainly been investigated in the treatment of pathologic scarring (hypertrophic and keloid scars) and in the sequelae of burns. While this drug has been investigated in several studies, that of Waibel et al.6 on hypertrophic scars causing functional restriction is noteworthy. The authors administered TCA using LADD (fractional CO2 laser), with 3-5 treatments every 2-3 months. Improvement was recorded not only in texture and thickness, but also for dyschromia and scar functionality. Several studies have reported similar results.37,38,61,62 Of particular interest is a study comparing effectiveness and tolerability in the treatment of hypertrophic scars using fractional Er:YAG followed by intralesional corticosteroid injections (TCA 10%) or topical corticosteroids (desoximetasone 0.25% under occlusion), with 4 sessions every 6 weeks. The results show the topical corticosteroid to be slightly more effective than the intralesional drug, although the difference was not statistically significant. The authors also reported much better scores for pain and patient preference.
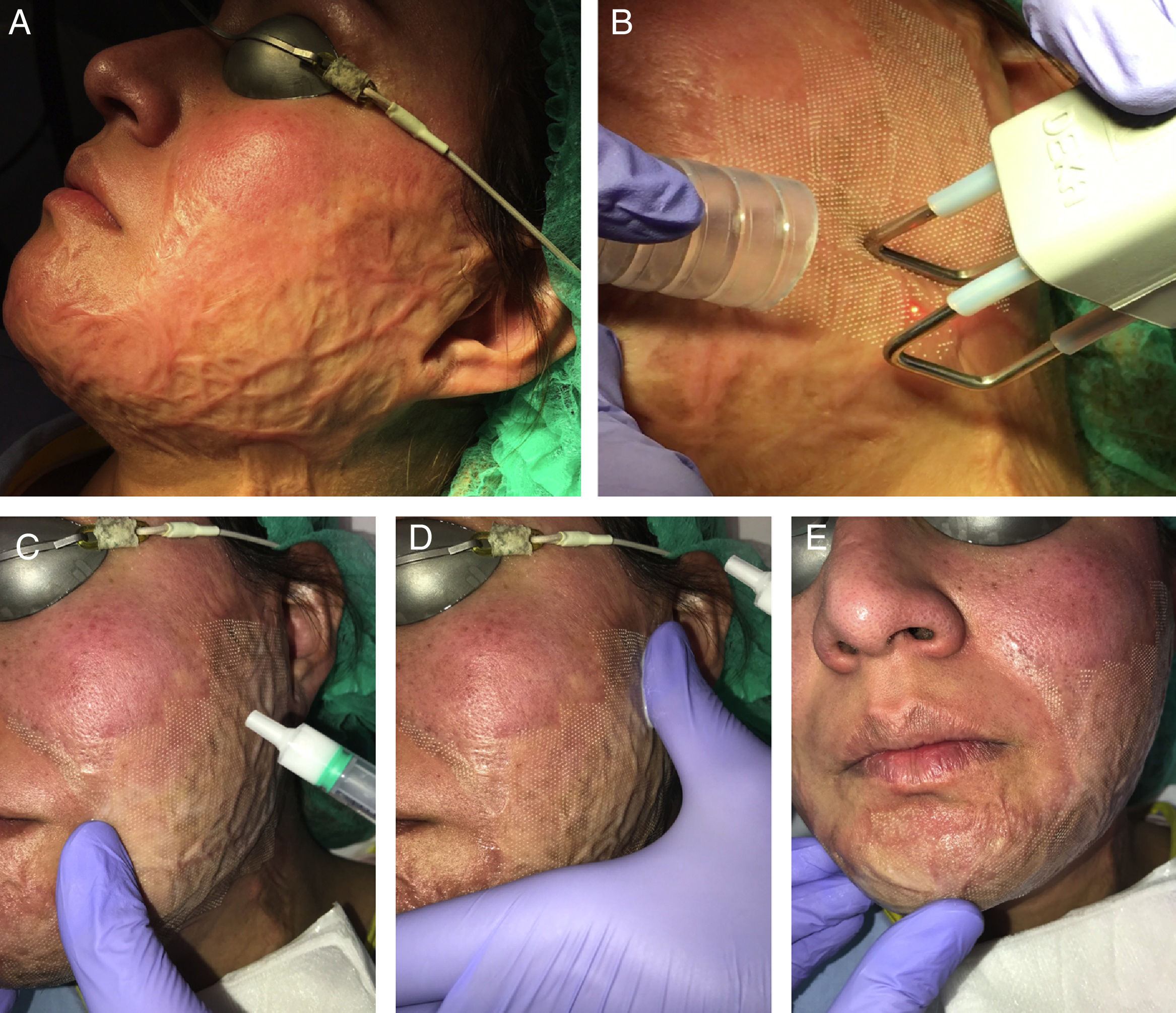
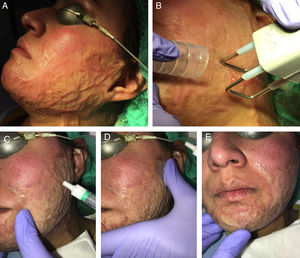
Our experience shows that the combination of CO2 laser and TCA 10% applied with smooth massage during the 15minutes following application of the laser yields very good results both for hypertrophic and keloid scars and for the sequelae of burns (Fig. 3). In addition, the simple application of topical anesthetic before laser treatment ensures better tolerance than combining laser treatment with subsequent TCA injections. In the case of very vascularized erythematous scars, this technique can be combined with a previous vascular approach based on techniques such as pulsed dye laser or intense pulsed light. For this purpose, we generally use pulsed dye laser (595nm) with pulses of 0.5-6ms and fluence of 5-7J/cm2, followed immediately by AFL.
Example of delivery of triamcinolone acetonide assisted by ablative fractional CO2 laser in a patient with sequelae of a facial burn. A, Before treatment. B, Pass of CO2 laser with a fractional scanner over the whole surface of the facial burn; a smoke extractor is used alongside the treatment. C, Application of injectable triamcinolone acetonide 10% solution: the solution is applied topically over the area treated with the laser. D, Extension of the corticosteroid over the whole area of the burn. E, Smooth massage to ensure better penetration of the product. gr3.
LADD has been used to introduce drugs and substances into the body for many and various reasons, in addition to those we have seen in dermatology. Studies in animals and humans have shown the efficacy of fully ablative and fractional lasers for introducing small interfering RNA molecules (siRNA) and antibodies.23,63 siRNA can inhibit translation of various genes, and this has proven useful in many diseases. Although the only studies on LADD with siRNA to date have been performed in mice, this pathway could be explored in the future in dermatological diseases using siRNA, as is the case with microRNA 21 in psoriasis, for example.
LADD has even proven effective for generating a favorable immune response with topical vaccines.22,64,65 Even more advanced are pilot studies with hematopoietic stem cells applied topically in combination with ablative laser in mice, thus paving the way for possible application of LADD as an alternative in hematopoietic progenitor transplant.66
ConclusionsLADD can yield better results with topical treatments by facilitating absorption and achieving a synergic effect between medical treatment (drugs) and physical treatment (lasers). Safety and the most appropriate technique remain controversial, although there is no doubt that these issues will gradually be resolved in the coming years.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alegre-Sánchez A, Jiménez-Gómez N, Boixeda P. Vehiculización de fármacos asistida por láser. Actas Dermosifiliogr. 2018;109:858–867.