Idiopathic facial aseptic granuloma is a typical childhood disease characterized by the presence of one or more asymptomatic nodules on the cheek. Although pathogenesis remains unclear, the disease is thought to be a type of childhood rosacea. It resolves spontaneously, yet it could be confused with other lesions that require treatment.
We present clinical and ultrasound findings and outcomes from 3 new cases. In 2 cases, the lesion presented as childhood rosacea. Ultrasound revealed a characteristic pattern, with variations depending on the stage of development.
High-frequency ultrasound can facilitate the differential diagnosis and thus obviate unnecessary biopsy or excision.
El granuloma aséptico facial idiopático es una entidad propia de la infancia que se caracteriza por la presencia de uno o varios nódulos asintomáticos en la mejilla. Aunque su patogenia no está clara, se ha sugerido que pueda pertenecer al espectro de la rosácea infantil. Resuelve espontáneamente pero puede plantear dudas diagnósticas con otras lesiones que sí requieren tratamiento.
Presentamos los hallazgos clínicos y ecográficos y la evolución, tanto clínica y ecográfica, de 3 nuevos casos. En 2 pacientes, la lesión se presentó en el contexto de una rosácea infantil. En ecografía, el granuloma aséptico facial idiopático mostró un patrón característico, con variaciones en función del momento evolutivo.
La ecografía de alta frecuencia puede facilitar el diagnóstico diferencial, evitando biopsias o extirpaciones innecesarias.
Idiopathic facial aseptic granuloma (IFAG) is a childhood disease characterized by the presence of one or more asymptomatic, red-to-violaceous nodules of soft or elastic consistency. It typically occurs on the cheek within a triangle delineated by the labial commissure, the earlobe, and the inferior orbital rim.1 Its etiology is unknown. Despite clinical similarities with abscess, infectious origin is ruled out based on the near systematic absence of a causative pathogen in culture. In the few cases in which bacteria have been isolated, the lesions had recently increased in size and the presence of pathogens was interpreted as a consequence of superinfection.1 According to some authors IFAG is a reaction to the presence of a persistent embryological remnant in the dermis. However, although lesion histology is compatible with foreign body granuloma, revealing lymphocytes, neutrophils, histiocytes, and giant cells, no embryonic remnants or other foreign bodies have been detected to support this hypothesis. One of the most widely accepted theories proposes that IFAG is a form of infantile rosacea, based on compatible histological findings and its frequent association with chalazion and other lesions of ocular rosacea.2–4 Diagnosis is established clinically, although in some cases biopsy is necessary. The differential diagnosis should include inflamed epidermoid cyst, pilomatricoma, and cutaneous Leishmania or mycobacterial infection. Unlike those entities, IFAG resolves spontaneously within several months or a year and therefore does not require treatment. Although there are few data published on IFAG ultrasound findings, high-frequency ultrasound can aid in its diagnosis.
Case DescriptionsWe present the clinical findings of 3 lesions that were clinically compatible with IFAG in 3 male patients aged 6, 9, and 12 years, as well as the corresponding findings of an ultrasound scan using a variable-frequency linear probe (maximum frequency, 18MHz).
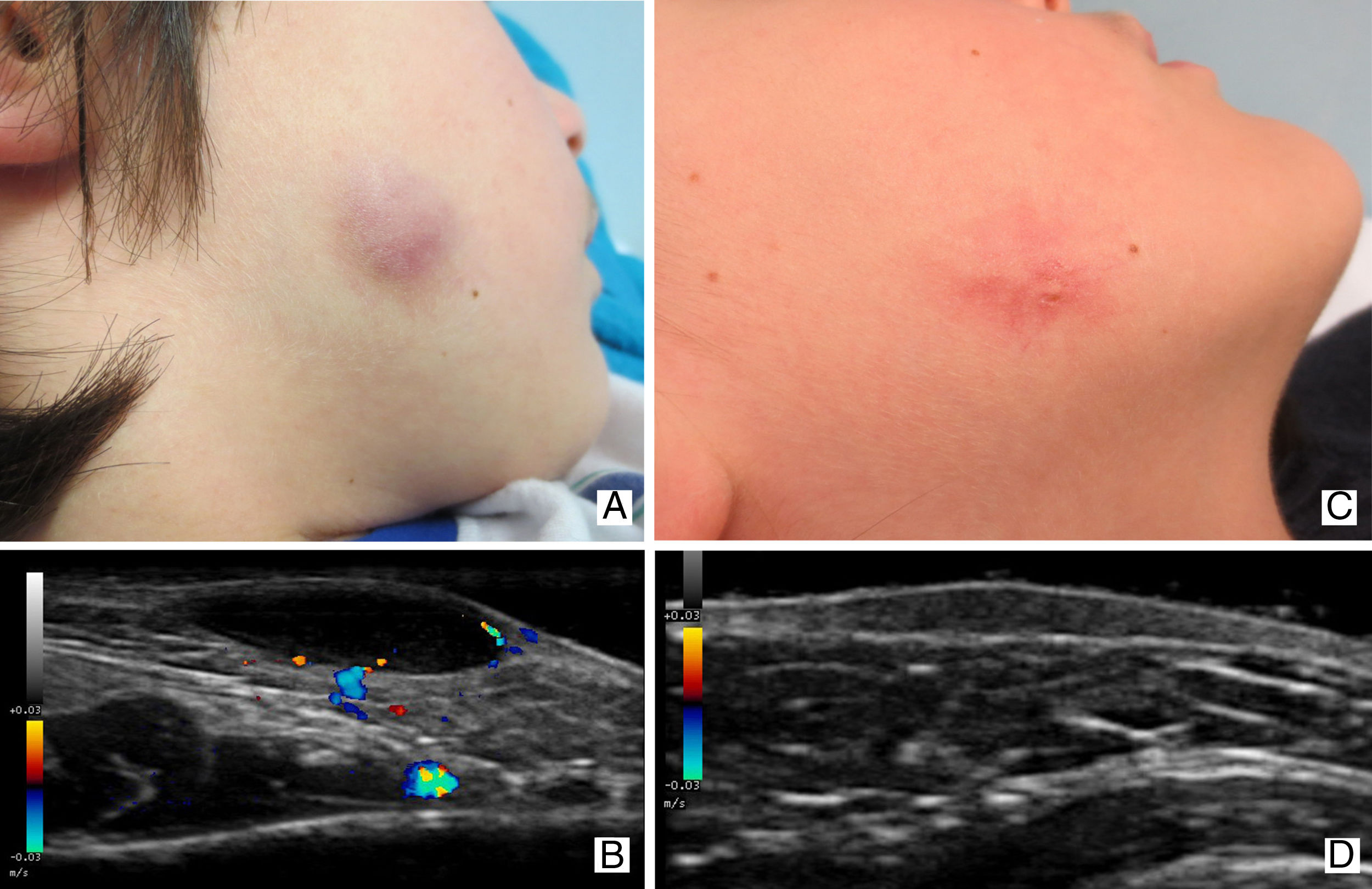
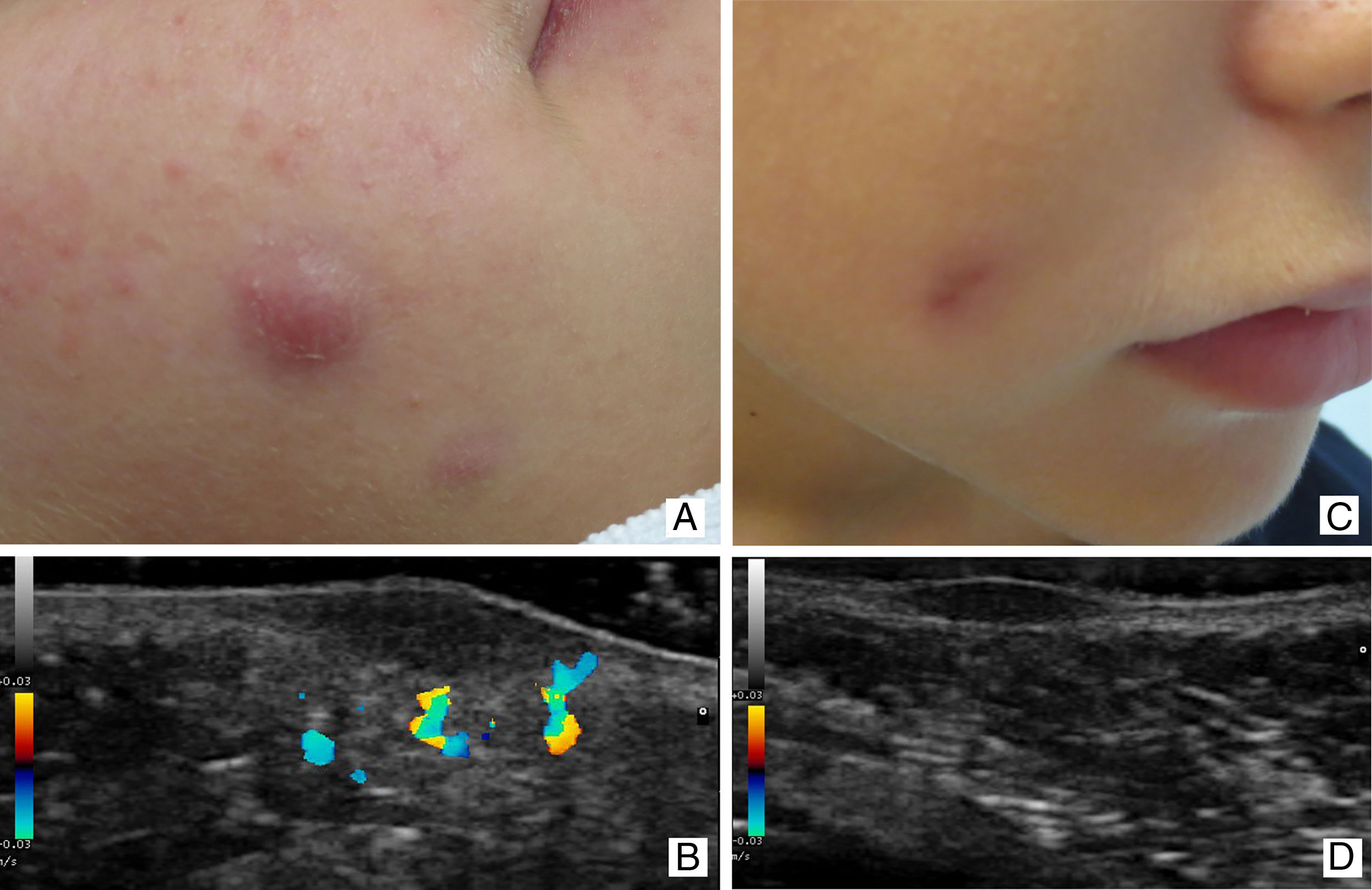
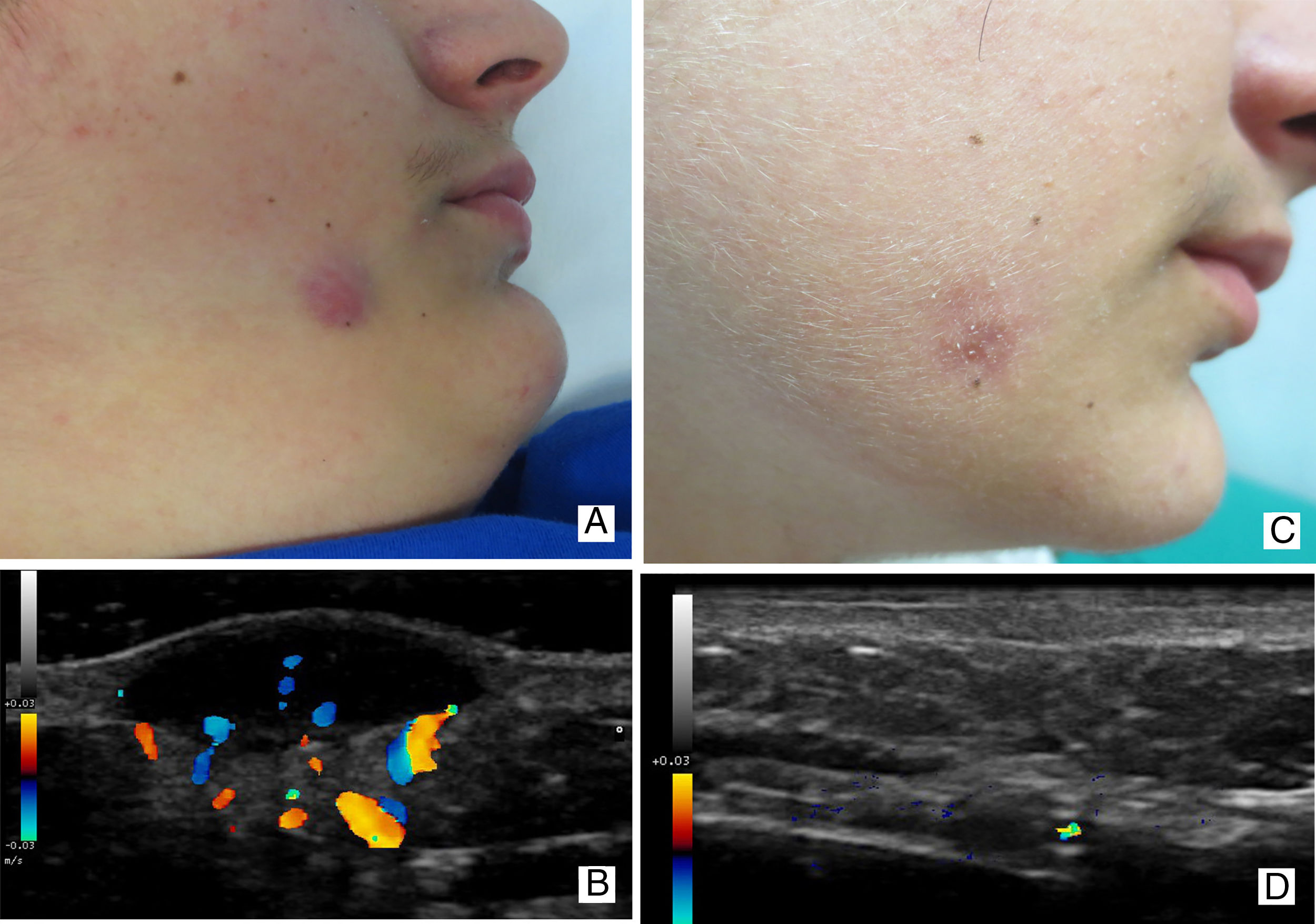
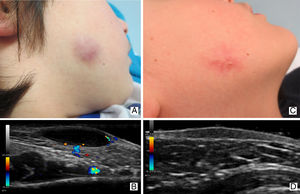
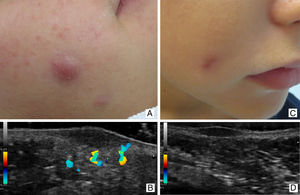
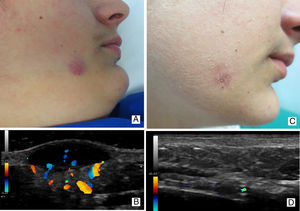
All 3 patients had a single, asymptomatic, firm erythematous-violaceous nodule on the cheek (Figs. 1A, 2A, and 3A). Papulopustular lesions were present on both cheeks of 2 of the patients (Figs. 2A and 3A), one of whom had a medical history that included recurrent chalazion and a resolved IFAG adjacent to the site of the new lesion. No comedones were observed in any of the patients.
Ultrasound revealed the following: in all 3 patients an ovoid lesion in the dermis that bulged towards the hypodermis, with a major axis parallel to the skin surface; and in 2 patients a deep, discreetly bulging or lobulated border (Figs. 2B and 3B). The 3 lesions were predominantly hypoechoic and largely heterogeneous, and contained an area of increased echogenicity at the base. No calcifications or structures compatible with foreign bodies or embryonic remnants were observed in any of the lesions. The increased echogenicity of the underlying hypodermis was not interpreted as a posterior enhancement artifact, but was considered representative of diffusely inflamed subcutaneous cellular tissue. Perilesional blood flow was observed in all cases, predominantly beneath the base of the lesion. In 2 cases, blood vessels were also observed in the deepest part of the lesion (Figs. 1B and 3B).
Clinical and ultrasound follow-up was performed at 6 months. By this time all lesions had decreased in size and the skin discoloration had resolved spontaneously (Figs. 1C, 2C, and 3C). Ultrasound revealed a marked reduction in the size of the ovoid structure in the dermis, no increase in the echogenicity of the underlying hypodermis, and an absence of blood flow in and around the lesion (Figs. 1D, 2D, and 3D).
DiscussionThe association of IFAG with papulopustular lesions in two of our patients and the history of recurrent chalazion in one patient support the hypothesis that IFAG is part of the clinical spectrum of childhood rosacea. The preexistence of more than one lesion in one of our cases also supports this view, and is in line with previous reports,1,2,5,6 including the series by Prey and coworkers,2 who reported this association in almost 16% (6/38) of patients.
Although the ultrasound features of IFAG have been described, few articles provide detailed information and images are scarce.1,4–6 In their study of 30 IFAGs, Boralevi and colleagues1 provide the corresponding image for 1 of 14 IFAGs for which ultrasound scans were performed, while Vázquez-Osorio et al,5 Zitelli et al,4 and Baroni et al6 each describe and provide ultrasound images for a single case. For all patients, ultrasound shows an ovoid hypoechoic lesion with well delineated, slightly irregular borders that is located in the dermis and the upper part of the hypodermis, with the major axis lying parallel to the skin surface. The images included in the aforementioned studies4–6 show a marked increase in the echogenicity of the hypodermis, although this is less pronounced in the image provided by Baroni et al. Zitelli and colleagues describe the presence of small lobulations in the deep margin of the lesion.
Neri et al.7 and Roul et al.8 describe the ultrasound findings for 3 and 2 IFAGs, respectively. Martínez-Díaz et al,9 Hiraldo-Gamero et al,10 and Orion et al3 each describe the ultrasound findings for a single case, but do not provide corresponding images. They describe the lesions as dermal3 or superficial,7 with a solid8–10 and/or hypoechoic3,7–10 appearance and increased perilesional echogenicity.7
No authors reported the presence of calcifications inside the lesions.1,4–10
Little information is available on Doppler ultrasound findings in IFAG. Neri and coworkers7 describe a perilesional increase in Doppler signal intensity in one case, while Vázquez-Osorio et al5 attribute the absence of Doppler signal to the involutive phase of the lesion.
We have found no reports in the literature of temporal variations in IFAG ultrasound features.
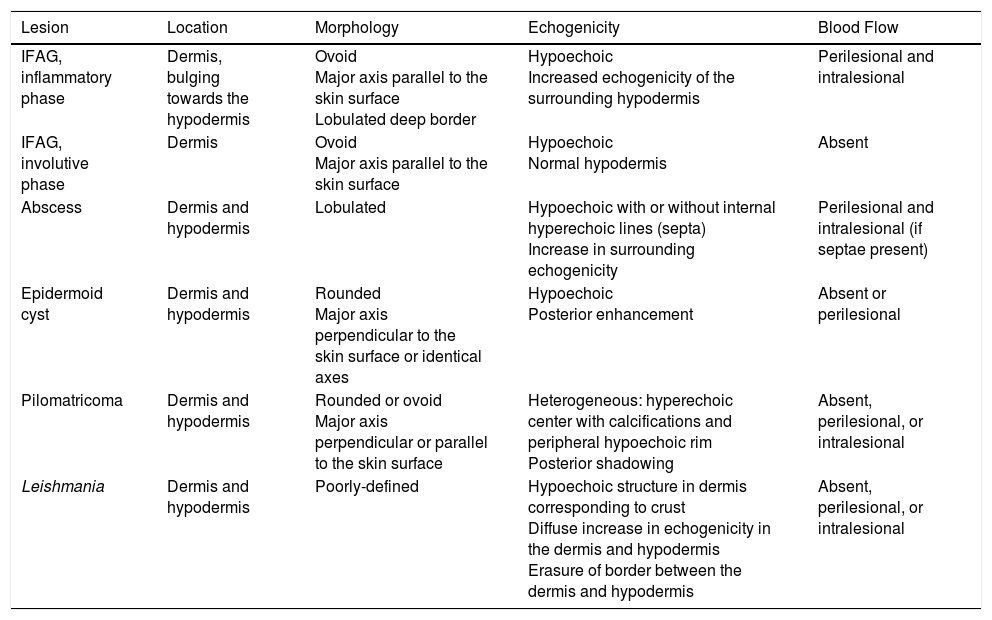
Based on our findings and those described in the literature, we believe that the characteristic ultrasound features of IFAG vary depending on the stage of development of the lesion, and that this feature allows differentiation of IFAG from other tumors included in the differential diagnosis (Table 1).
Ultrasound Features and Differential Diagnosis of Idiopathic Facial Aseptic Granuloma.
| Lesion | Location | Morphology | Echogenicity | Blood Flow |
|---|---|---|---|---|
| IFAG, inflammatory phase | Dermis, bulging towards the hypodermis | Ovoid Major axis parallel to the skin surface Lobulated deep border | Hypoechoic Increased echogenicity of the surrounding hypodermis | Perilesional and intralesional |
| IFAG, involutive phase | Dermis | Ovoid Major axis parallel to the skin surface | Hypoechoic Normal hypodermis | Absent |
| Abscess | Dermis and hypodermis | Lobulated | Hypoechoic with or without internal hyperechoic lines (septa) Increase in surrounding echogenicity | Perilesional and intralesional (if septae present) |
| Epidermoid cyst | Dermis and hypodermis | Rounded Major axis perpendicular to the skin surface or identical axes | Hypoechoic Posterior enhancement | Absent or perilesional |
| Pilomatricoma | Dermis and hypodermis | Rounded or ovoid Major axis perpendicular or parallel to the skin surface | Heterogeneous: hyperechoic center with calcifications and peripheral hypoechoic rim Posterior shadowing | Absent, perilesional, or intralesional |
| Leishmania | Dermis and hypodermis | Poorly-defined | Hypoechoic structure in dermis corresponding to crust Diffuse increase in echogenicity in the dermis and hypodermis Erasure of border between the dermis and hypodermis | Absent, perilesional, or intralesional |
Abbreviations: IFAG, idiopathic facial aseptic granuloma.
On ultrasound, IFAG appears as an ovoid, predominantly hypoechoic lesion located mainly in the dermis, with the major axis lying parallel to the skin surface. Ultrasound markers of inflammation are observed in the active or inflammatory phase. These include perilesional and intralesional blood flow, especially in the deepest part of the lesion, and an increase in the echogenicity of the underlying hypodermis (Figs. 1B, 2B, and 3B). Contrary to the proposals of some authors, we believe that the increase in echogenicity in the hypodermis should not be interpreted as a posterior enhancement artifact. The echogenicity is distributed diffusely throughout the hypodermis surrounding the IFAG. The echogenic area includes locations that the ultrasound reaches without first passing through the lesion and thereby undergoing the sudden impedance changes characteristic of an artifact. Furthermore, the observed increase in echogenicity is smooth and homogeneous, whereas posterior enhancement artifact is usually bright with progressive attenuation.
With resolution of the lesion, the thickness of the hypoechoic structure decreases and the vascularization and increased echogenicity of the underlying subcutaneous cellular tissue disappear (Figs. 1D, 2D, and 3D). The normalization of the echogenicity of the surrounding subcutaneous cellular tissue, coinciding with a decrease in clinical signs of inflammation, supports our hypothesis that the changes in the echogenicity of the hypodermis are not artefactual but in fact reflect an inflammatory process that also involves the hypodermis.
The appearance of IFAG as an inflammatory lesion with ultrasonographic features that change over time supports the view that this lesion is a form of infantile rosacea, and contradicts other theories.
Like any granuloma, IFAG is predominantly hypoechoic. However, it is not organized around a foreign body and is therefore unlikely to be the result of a reaction to an embryonic remnant.
Fluid collection and abscess can be ruled out based on the presence of intralesional blood flow in the absence of septae. Moreover, abscesses are usually located in the hypodermis, can reach large sizes, and have varying morphologies with lobulations on any border.
The ultrasound features of IFAG differ to those of epidermoid cyst and pilomatricoma, both of which originate in the dermis but tend to occupy part or all of the hypodermis.
Epidermoid cysts typically present as a rounded tumor and therefore usually lacks a major axis lying parallel to the skin surface. It is generally accompanied by posterior enhancement and lacks intralesional vascularization. Abundant perilesional blood flow and a diffuse increase in the echogenicity of subcutaneous cellular tissue can be observed when the cyst is either inflamed or ruptured.11
Pilomatricoma can present with diverse morphologies and is characterized on ultrasound by bright hyperechoic structures that represent calcifications, a peripheral hypoechoic rim, and posterior shadowing.12 Posterior acoustic reinforcement has occasionally been described in pilomatricoma, but a diffuse increase in the echogenicity of the underlying hypodermis is uncommon. Intralesional vascularization may be observed in pilomatricoma.13
We have found no descriptions of the ultrasound findings of cutaneous Leishmania infection. However, in our experience Leishmania infection is characterized by a diffuse increase in the echogenicity of the dermis and hypodermis and erasure of the border between the dermis and hypodermis. On ultrasound the clinically evident crust appears as a hypoechoic triangular structure located in the dermis, with the apex facing downwards.
Clinical and ultrasound findings in our 3 patients support the hypothesis that IFAG is a manifestation of childhood rosacea. We believe that ultrasound is a useful tool to support clinical suspicion of IFAG, estimate the stage of lesion development, and obviate unnecessary biopsy or excision of a lesion that resolves spontaneously.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez-Bandera AI, Feito-Rodríguez M, Maseda-Pedrero R, de Lucas-Laguna R. Granuloma aséptico facial idiopático: hallazgos clínicos y ecográficos de 3 casos. Actas Dermosifiliogr. 2018;109:e1–e5.