Clear cell papulosis (CCP) is a rare entity of unknown cause that was first described in 1987.1 It is reported more frequently in Asian countries and usually affects children under 2 years of age, with comparable prevalence in both sexes.2 It is characterized by flat, hypopigmented, asymptomatic macules and/or papules of 2 mm to 10 mm located on the lower abdomen and pubic area, and less frequently on the axillae, mammary line, groin, and extremities.3 Histology reveals the characteristic presence of round clear cells with abundant, pale cytoplasm located between the basal and suprabasal keratinocytes. On immunohistochemistry these cells are positive for antibodies against cytokeratin AE1/AE3, cytokeratin 7 (CK7), cytokeratin CAM5.2, carcinoembryonic antigen, epithelial membrane antigen, and gross cystic disease fluid protein.3 Both the origin and the role of these clear cells remain unclear.4 It is suggested that they are derived from secretory cells of the eccrine glands.5 It has also been proposed that clear cells are derived from Toker cells and may serve as precursor cells of Paget disease, although progression from CCP to Paget disease has not been demonstrated to date.2
CCP is asymptomatic, and does not require treatment. In most cases lesions disappear with time.3
Case DescriptionsA search for patients diagnosed with CCP in 3 pediatric hospitals in Peru and Argentina between 2010 and 2016 identified 8 cases: 7 females and 1 male. Lesions had appeared before 2 years of age in all cases, and were present from birth in one case (Table 1). All patients had hypopigmented lesions (2–3 mm in diameter). The majority of lesions were macules, followed by papules, and most were located on the lower abdomen and pubic area (Fig. 1). Other affected areas included the axillae, mammary line, buttocks, lumbar region, and legs.
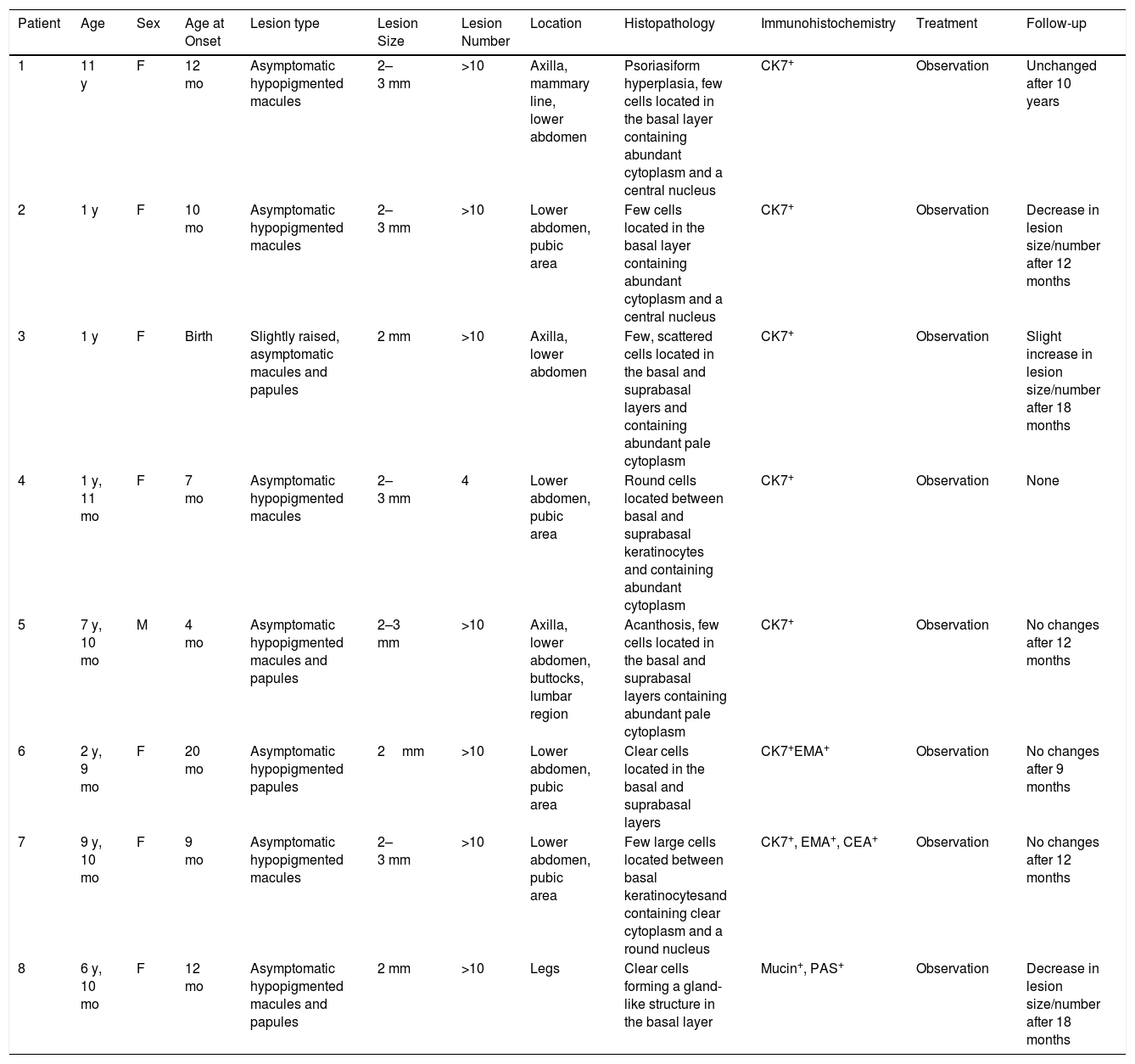
Epidemiological, Clinical, and Histopathological Characteristics and Duration of Follow-up
| Patient | Age | Sex | Age at Onset | Lesion type | Lesion Size | Lesion Number | Location | Histopathology | Immunohistochemistry | Treatment | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 11 y | F | 12 mo | Asymptomatic hypopigmented macules | 2–3 mm | >10 | Axilla, mammary line, lower abdomen | Psoriasiform hyperplasia, few cells located in the basal layer containing abundant cytoplasm and a central nucleus | CK7+ | Observation | Unchanged after 10 years |
| 2 | 1 y | F | 10 mo | Asymptomatic hypopigmented macules | 2–3 mm | >10 | Lower abdomen, pubic area | Few cells located in the basal layer containing abundant cytoplasm and a central nucleus | CK7+ | Observation | Decrease in lesion size/number after 12 months |
| 3 | 1 y | F | Birth | Slightly raised, asymptomatic macules and papules | 2 mm | >10 | Axilla, lower abdomen | Few, scattered cells located in the basal and suprabasal layers and containing abundant pale cytoplasm | CK7+ | Observation | Slight increase in lesion size/number after 18 months |
| 4 | 1 y, 11 mo | F | 7 mo | Asymptomatic hypopigmented macules | 2–3 mm | 4 | Lower abdomen, pubic area | Round cells located between basal and suprabasal keratinocytes and containing abundant cytoplasm | CK7+ | Observation | None |
| 5 | 7 y, 10 mo | M | 4 mo | Asymptomatic hypopigmented macules and papules | 2–3 mm | >10 | Axilla, lower abdomen, buttocks, lumbar region | Acanthosis, few cells located in the basal and suprabasal layers containing abundant pale cytoplasm | CK7+ | Observation | No changes after 12 months |
| 6 | 2 y, 9 mo | F | 20 mo | Asymptomatic hypopigmented papules | 2mm | >10 | Lower abdomen, pubic area | Clear cells located in the basal and suprabasal layers | CK7+EMA+ | Observation | No changes after 9 months |
| 7 | 9 y, 10 mo | F | 9 mo | Asymptomatic hypopigmented macules | 2–3 mm | >10 | Lower abdomen, pubic area | Few large cells located between basal keratinocytesand containing clear cytoplasm and a round nucleus | CK7+, EMA+, CEA+ | Observation | No changes after 12 months |
| 8 | 6 y, 10 mo | F | 12 mo | Asymptomatic hypopigmented macules and papules | 2 mm | >10 | Legs | Clear cells forming a gland-like structure in the basal layer | Mucin+, PAS+ | Observation | Decrease in lesion size/number after 18 months |
Abbreviations: CEA, carcinoembryonic antigen; CK7, cytokeratin 7; EMA, epithelial membrane antigen; F, female; M, male; PAS, periodic acid-Schiff.
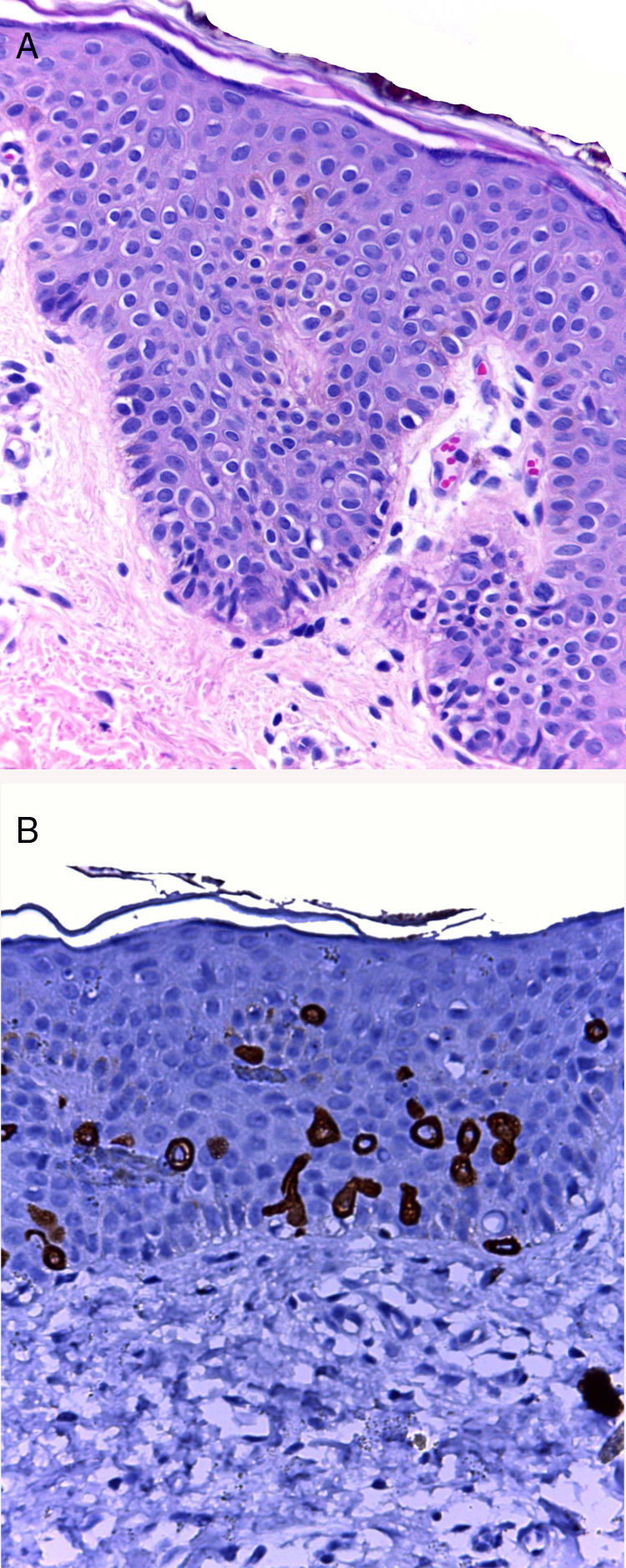
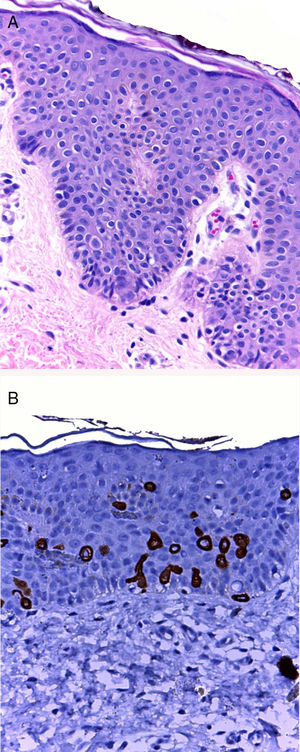
The initial clinical diagnosis was CCP in 6 patients and postinflammatory hypopigmentation in 2 patients. In all cases, histology revealed few scattered large cells with abundant clear cytoplasm located in the basal and suprabasal layers. Seven patients were positive for anti-CK7 immunostaining (Fig. 2). In 3 of these patients CK7+ cells were located next to the opening of the acrosyringium, while in Patient 8 the CK7+ cells formed a gland-like structure and were positive for periodic acid-Schiff (PAS) and Alcian blue stains.
A, Few scattered round cells with abundant clear cytoplasm in the basal layer of the epidermis (hematoxylin-eosin, original magnification ×10). No changes are evident in the dermis. B, Anti-cytokeratin 7 immunostaining reveals the presence of clear cells, located predominantly in the basal layer and also in the suprabasal layer.
None of the patients received treatment. Seven patients underwent clinical follow-up for 9 to 18 months. Information on the clinical evolution of the remaining patient (Patient 1) was provided by a family member. Lesions remained stable in 4 patients (after 9, 12, and 12 months, and 10 years of follow-up, respectively), improved in 2 patients (after 2 and 18 months), and worsened in 1 patient (after 18 months).
There are few reported cases of CCP,2 and only 5 out of 39 reported cases involve non-Asian patients.6–8 The majority of patients in our series were female and most developed lesions within the first years of life, except for one patient who was diagnosed at 11 years of age. This profile is in line with that described in previous case reports, in which all patients have been children,2 except for 1 adult case.9
All patients in our series were born to Latin American parents and presented multiple small hypochromic macules and/or papules in the lower abdomen and pubic area. Other affected areas included the axillae, mammary line, buttocks, and lumbar region. In one patient, lesions were located exclusively on the legs, which is not a commonly affected region.
Histologically, clear cells can be confused with melanocytes, Toker cells, or Langerhans cells.10 Diagnosis is primarily based on histology, although immunohistochemistry can be useful in doubtful cases. It is worth noting that in some cases the CK7+ cells were located close to the opening of the acrosyringium. Unusually, in Patient 8 these CK7+ cells formed a gland-like structure and were positive for Alcian blue and PAS, indicating the presence of mucin. These findings support the view that these cells have a glandular origin, as proposed by Kim and coworkers.5
The lesions usually increase in size and number during the first months and years of life, but gradually diminish without leaving sequelae within a mean period of 11 years after appearance.3 Although the follow-up of 7 patients was limited to 9 to 18 months, 2 patients (Patients 2 and 8) showed a decrease in lesion size and number during this time.
Familiarity with this entity is important given that hypopigmented lesions are common in pediatric patients. The main differential diagnosis is postinflammatory hypopigmentation. Other clinical diagnoses to consider include pityriasis versicolor, flat warts, and vitiligo.
This is the first reported series of CCP cases in Latin America. Identification of this rare entity in children is important to avoid erroneous diagnoses and unnecessary treatments.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Apagüeño C, Pomar R, Peceros J, Velásquez F, Ballona R, Castro R, et al. Papulosis de células claras: una serie de casos. Actas Dermosifiliogr. 2019;110:402–405.