A 59-year-old man visited our department with an asymptomatic skin lesion of the glans that had appeared 4 months earlier. He denied having engaged in risky sexual practices. He had no past history of phimosis or prior episodes of trauma or spontaneous bleeding.
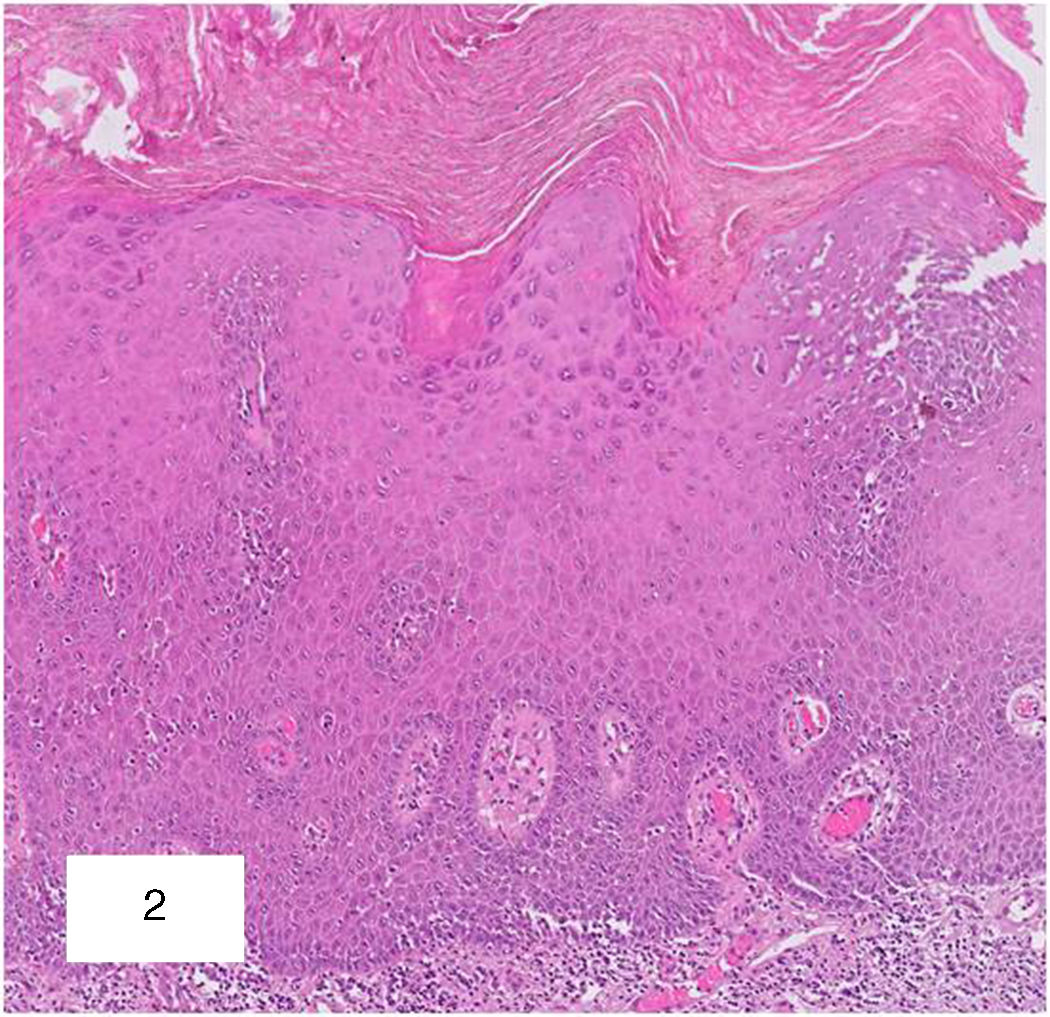
Physical ExaminationPhysical examination revealed a clearly defined, whiteish keratotic plaque with a diameter of 2cm and a papillomatous surface, close to the urinary meatus (Fig. 1). The patient had no palpable local or regional lymph nodes.
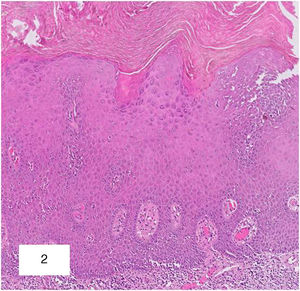
Additional TestsA complete blood count, biochemical analysis, and serology for virus and syphilis were normal. Polymerase chain reaction for human papilloma virus (HPV) was negative. Histopathology revealed epithelial hyperplasia with hyperkeratosis, parakeratosis, and considerable monocytic/lymphocytic infiltration of the dermis with some eosinophils (Fig. 2).
What Is Your Diagnosis?DiagnosisLortat-Jacob and Civatte pseudoepitheliomatous keratotic and micaceous balanitis (PKMB).
Clinical Course and TreatmentTopical treatment was instated with a combination of 0.5% 5-fluorouracil and 10% salicylic acid, applied once daily for 12 weeks. The treated area became severely irritated and treatment was suspended for 2 weeks. Subsequent examinations revealed a gradual reduction of the plaque. Persistence of the entity was confirmed in a new biopsy and treatment with ultrapulse CO2 laser was instated, with a treated area of 34% and energy density of 42.2J/cm2. The patient is currently undergoing follow-up at our department and shows no signs of local recurrence.
CommentPKMB was first described by Lortat-Jacob and Civatte in 1966.1 The disease affects the glans and manifests as keratotic lesions reminiscent of psoriasis plaques. The literature contains few references to this entity and, in epidemiological terms, most published cases are of patients of Indian ethnicity.
Its etiology is currently the subject of debate. The disease has 4 clinical stages: initial or plaque stage, late tumoral stage, warty carcinoma, and transformation into squamous cell carcinoma.
Histopathology typically reveals the following changes: hyperkeratosis, parakeratosis, acanthosis, elongated papillary crests, and mild dysplasia in the basal layers. Nonspecific inflammatory infiltration may be observed in the superficial dermis, with variable numbers of lymphocytes and eosinophils.2
Some authors have questioned the potential for this rare form of balanitis to become malignant, but an increase has been reported in the number of recorded cases of warty carcinoma and squamous cell carcinoma arising from PKMB lesions, either at the time of presentation or later.2 Careful follow-up of these patients is therefore important. To date, no link has been found between PKMB and HPV. In 1 case of warty carcinoma from PKMB, in situ hybridization and PCR were negative for HPV in the tumor and in the precancerous lesion.3
The differential diagnosis should include 3 approaches: infectious causes, with sexually transmitted diseases such as genital herpes simples, soft chancre, and primary syphilis; inflammatory causes, with diseases such as hypertrophic lichen planus and Zoon plasma cell balanitis; and oncologic causes, with penile intraepithelial neoplasia (PeIN), warty carcinoma, squamous cell carcinoma, keratoacanthoma, giant condylomatosis, and erythroplasia of Queyrat.4 The absence of atypical cells in PKMB histology may be a key finding that makes it possible to differentiate it from oncologic entities, although correlation with the clinical presentation is necessary.
Early clinical diagnosis and biopsy of the lesion are of considerable value, as the disease can be treated topically with 5-fluorouracil,1,5 which produced a good response in our patient. Other treatment options include cryotherapy, photodynamic therapy,6 and wide resection, which should be reserved for cases where histology reveals atypical cells. We report a case of PKMB treated with 5-fluorouracil in combination with salicylic acid, with a good initial response. Treatment was completed with adjuvant CO2-laser treatment, which, to date, has not been reported in this disease.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank Dr. Ainhoa Bueno Rodriguez for her support in resolving this case, and Dr. Naranjo Sintes and Dr. Aneiros Fernández for their help in resolving the histology.
Please cite this article as: Aguayo-Carreras P, Navarro-Triviño FJ, Ruiz-Villaverde R, Saenz-Guirado S. Placa hiperqueratósica asintomática en glande en un varón de mediana edad. Actas Dermosifiliogr. 2018;109:913–914.