Dermatologists are regularly consulted in their place of work by patients without an official appointment (individuals accompanying other patients, doctors from other specialties, hospital workers, etc).
ObjectivesTo describe the characteristics of consulting patients, reasons for consultation, severity of complaint, diagnostic and therapeutic approach taken, and level of care provided by the consulted professionals.
ResultsThe typical patient would be a middle-aged female nurse consulting for the first time for a benign melanocytic lesion. In general, the dermatologist will take an empirical or informative therapeutic approach and consider the care provided to be similar to that offered to patients with an official appointment.
ConclusionsUnofficial appointments, although commonly for trivial complaints, represent an additional workload in daily clinical practice.
Los dermatólogos somos demandados a diario, en nuestro centro de trabajo, por pacientes sin cita reglada (acompañantes de pacientes, médicos de otras especialidades, trabajadores del centro, etc.).
ObjetivosDescripción de los pacientes demandantes, los motivos de consulta, la gravedad de la patología consultada, la actitud diagnóstico-terapéutica y asistencial de los profesionales demandados.
ResultadosEl paciente modelo sería una mujer enfermera de mediana edad que consulta por primera vez por una lesión tumoral melanocítica benigna. En general el dermatólogo tomará una actitud terapéutica empírica o informadora y considera que la atención prestada es similar a un paciente con cita reglada.
ConclusionesLas consultas no regladas, aunque suelen ser por patología banal, suponen una carga asistencial en la práctica diaria.
Throughout their career and even as early as medical school, physicians are often consulted outside the appointments system. Medical professionals, but particularly dermatologists, can easily recall a situation in which medical advice was informally requested in a street, elevator, corridor, and even in the surgery.
Dermatologists are possibly more likely than other specialists to be asked for informal medical advice, given that the skin is immediately accessible and easily explored. It is this very accessibility, in fact, that leads people to expect the dermatologist to be able to resolve their query immediately.
With a view to better understanding informal consultations in a hospital setting, we documented 270 consultations between October 2008 and July 2009 in order to profile the individuals who request medical advice, their reasons for consulting, the severity of their complaints, and the dermatologists’ responses.
ObjectivesThe objectives of the study were to describe the following: (1) the profiles of the consulting individuals, (2) the reasons for consultation, (3) the dermatologist's diagnosis and treatment, (4) the dermatologist's assessment of the severity of the complaint, and (5) the dermatologist's assessment of the care given.
Material and MethodsThe data for the study were recorded by dermatologists and resident dermatologists at Hospital Clínico San Cecilio de Granada, Spain. Given the lack of similar studies, the dermatologists applied criteria based on their professional experience.
Inclusion criteria for consulting individuals were as follows: they did not have a formal appointment on the day of the consultation; they had not used the emergency service on the day of the consultation (for whatever reason); they made the consultation within the hospital; and the consultation was about a skin complaint.
Data were collected between October 2008 and July 2009 and analyzed using SSPS statistical software, version 17.0.
Age and sex were recorded, and the consulting individuals were classified in 5 categories, as follows: persons accompanying patients, physicians in other disciplines, hospital workers (excluding physicians), dermatologist's family or friends, and medical representatives. The hospital workers were further subdivided into the following groups: administrative workers, nursing auxiliaries, hospital porters, cooks, nurses, cleaners, technical staff, security staff, and others. Information was also collected on whether this was the individual's first consultation regarding the skin complaint, whether the person had previously consulted for another reason, and whether the person was consulting on their own behalf or on someone else's.
The reasons for consultation were classified in 13 broad diagnostic groups: dermatitis, eczemas, esthetic/cosmetic complaints, infections, lichens, nail disorders, psoriasis, burns, benign tumors, malignant tumors, skin discoloration, surgery-related complaints (secondary to surgery or lesions), and undiagnosed complaints. These reasons were further subclassified according to the definitive diagnosis, with the exception of skin complaints that remained undiagnosed due to the need for further tests.
Diagnostic and therapeutic responses were classified as follows: empirical treatment, biopsy for histology study, referral to the family physician or for a formal visit, patient reassurance and information, microbiology study or blood testing, surgical treatment, and other responses.
The dermatologists scored severity on a scale of 1 to 9, with 1 representing a mild complaint, and 9 representing a complaint needing urgent medical attention. The consulting individuals were divided into those whose complaint could or could not be postponed to a formal visit (implying an average wait of 1 month).
The dermatologists’ own assessment of the care provided to these individuals in comparison with their care of formal patients was classified as follows: less care; standard care; or better care, ie, the dermatologist had performed nursing or administrative procedures, or had personally consulted other professionals, and in doing so, had disregarded standard protocols and routine procedures.
ResultsProfiles of the Consulting IndividualsA total of 270 informal consultations were documented. More consultations were made by women than by men (63% vs 37%), and the mean age was 40.13 years (range, 1-92 years).
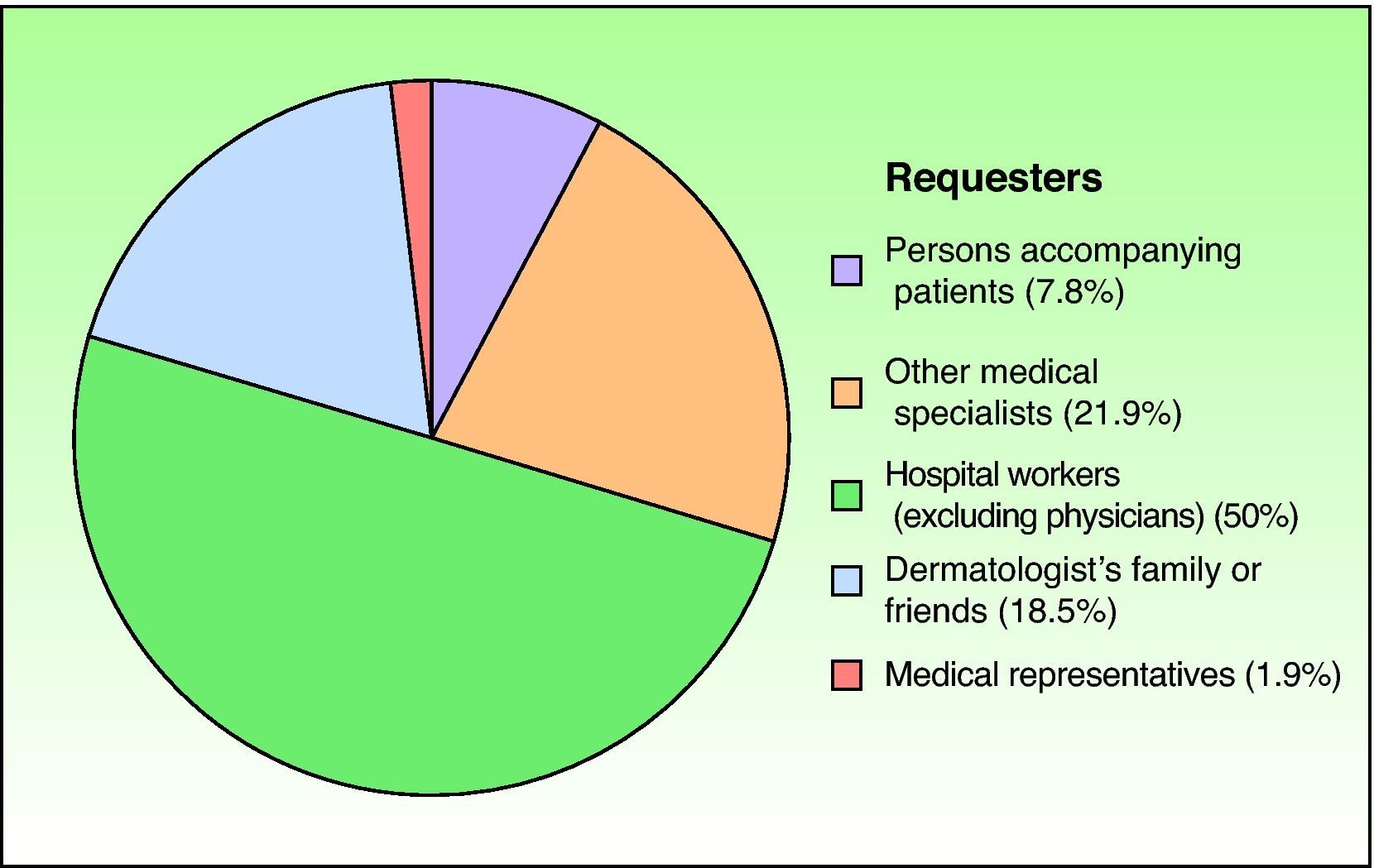
Most consultations (50%) were made by hospital workers, followed by other medical specialists (21.9%), the dermatologist's family or friends (18.5%), persons accompanying patients (7.8%), and medical representatives (1.9%) (Fig. 1).
The consultations by hospital workers (excluding physicians) were classified according to the following subtypes: nurses (40.7%), nursing auxiliaries (27.4%), cleaners (9.6%), administrative staff (5.9%), hospital porters (5.9%), nonidentified occupations (3.7%), technical staff (3.0%), security staff (2.2%), and cooks (1.5%).
Most consulting women were nurses, followed by nursing auxiliaries; and most consulting men were other medical specialists, followed by the dermatologist's family or friends.
For 74.4% of the individuals, this was their first consultation regarding the complaint in question; for the remaining 25.6%, the consultations referred to treatment failures, follow-ups, diagnostic test results, etc. The dermatologist had previously been consulted for a different reason by 39.3% of the individuals; for the remaining 60.7%, this was their first dermatology consultation.
An interesting finding was the number of individuals consulting the dermatologist on behalf of someone else. This was a feature of all the groups with the exception of the group composed of persons accompanying patients; excluding this group, a third (36.1%) of the informal consultations were made on behalf of someone else.
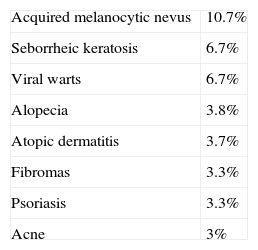
Reasons for ConsultationThe highest number of consultations corresponded to the benign tumors group (40.4%), broken down as follows: acquired melanocytic nevi (10.7%), seborrheic keratosis (6.7%), viral warts (6.7%), and fibromas (3.3%) (Table 1). Dermatitis was the second largest group (17%), with atopic dermatitis (3.7%) and seborrheic dermatitis (2.6%) heading the list. The third largest group referred to esthetic/cosmetic complaints (8.9%), with alopecia (all subtypes) accounting for 3.8% of the consultations.
The remaining groups, in descending order of importance, were as follows: infections (8.5%), eczemas (5.6%), malignant tumors (4.4%), skin discoloration (4.1%), nail disorders (4.1%), psoriasis (3.3%), surgery-related complaints (1.9%), and lichens, burns, and undiagnosed skin complaints (under 1% each).
The 6 most frequent diagnoses were acquired melanocytic nevi (10.7%), seborrheic keratosis (6.7%), viral warts (6.7%), alopecia (6.7%), atopic dermatitis (3.7%), and fibromas and psoriasis (3.3% each).
Diagnostic and Therapeutic ResponsesThe most frequent dermatologist responses to consultations were as follows: empirical treatment (54.1%), patient reassurance and information (22.6%), surgical treatment (13%), referral for further tests (6%), referral to the family physician (2.6%), and histology studies (biopsy) to confirm diagnosis (2.6%). The remaining categories (microbiology studies, referral to another specialist, referral for an imaging study, etc) accounted for under 2% of the responses.
Severity According to the DermatologistThe dermatologists rated skin complaint severity on a scale from 1 to 9, with 9 representing the greatest severity. The results largely reflect a descending curve, with 61.1% of complaints receiving a score of 1, 18.5% a score of 2, and 10.7% a score of 3, with the remaining scores (4 to 9) assigned to 3.7%, 2.6%, 1.1%, 0.7%, 1.1%, and 0.4% of the complaints, respectively.
Most of the individuals (87%) were asked to postpone their consultation to a formal visit (an average wait of 1 month), leaving 13% who were considered to need urgent attention.
Level of Care According to the DermatologistThe dermatologists rated management and care as similar to that for patients with an appointment for 75.9% of the individuals, and as less scrupulous for 8.5% of the individuals. The remaining 15.6% of individuals were rated as having received better care, given that procedures were followed that were not standard in the dermatologists’ daily routines.
DiscussionDermatologists are often asked for a medical opinion in the workplace (in corridors, offices, surgeries, etc). Such consultations, facilitated by the accessibility of the skin, are not regulated, recorded, or scheduled. They usually imply an investment in terms of time, and occasionally require the use of health care resources. Since our study was conducted in a hospital, consultations with dermatologists outside work were not included.
The work setting defines certain characteristics of the consulting individual. In our hospital-based study, for example, the typical requester was a female, middle-aged nurse, reflecting the fact that our hospital has more female than male nurses and that its employees are largely middle-aged.
The skin complaints for which medical advice was requested were, in the opinion of the dermatologists, mainly mild. The most frequent complaints were benign tumors, specifically, melanocytic nevi (10.7%), seborrheic keratosis, and viral warts (6.7% each). Our findings partially corroborate the study by Tejera-Vaquerizo et al1 regarding the reasons for additional consultations by dermatology patients (ie, about conditions not covered by the primary care referral): melanocytic nevi (18%) was the most frequently mentioned complaint (intradermal nevi, 11.5%, and common melanocytic nevi, 6.5%), followed by eczema (11%), acne and viral warts (6.8% each), and seborrheic keratosis and cysts (6.3% each). The demographic characteristics of the patients have a bearing on the reason for consultation. Half the patients in the study by Tejera-Vaquerizo et al were aged 10 to 40 years, and acne was a frequent motive for consultation (6.8%); in our study, in contrast, where the mean age was over 40 years, acne (3%) was not among the top 5 complaints.
Informal and nonregulated patient care represents significant savings for the public health system. We used designated costs for dermatology consultations (based on the analytical accountancy system used for Andalusian hospitals and districts (COAN-HyD) and the COAN total costs module)2 to calculate that savings for the Spanish public health system amounted to around €26 000 for the initial consultations and €2000 for the follow-up consultations (74.4% and 25.6%, respectively, of the 270 consultations). Around a fifth of the informal consultations required the use of surgical, histological, laboratory resources, etc, but over half were diagnosed and treated empirically and so did not consume hospital resources. Since a small proportion of requesters (2.6%) was referred to the family physician and so deferred to the formal system, this cost should logically be deducted from the above savings.
Nonregulated informal consultations represent an increased workload for dermatologists, as do the additional consultations referred to in the study by Tejera-Vaquerizo et al.1 They also represent an important proportion of the care activities undertaken by dermatology residents on duty. Obviously, dermatologists who refuse to provide medical advice in this way, or who persuade the requesters to postpone consultation to a formal appointment, do not experience the same degree of overload. According to the dermatologists who participated in this study, additional and nonregulated consultations represent an extra workload of around 25%, to be added to formal appointments and residential duties. Particularly time-consuming are consultations made on behalf of someone else: the requester usually describes the other person's symptoms in detail, but in most cases, the dermatologist inevitably has to see the person with the skin complaint. The dermatologists agreed that it was not infrequent for them to see 4 to 6 people per day in informal consultations, in addition to 20 to 25 patients with formal appointments (bearing in mind, also, that around 18% of patients miss their appointment according to Tejera-Vaquerizo et al1). Furthermore, according to the dermatology residents participating in this study, the burden increases substantially during duty shifts.
The circumstances of informal consultations may suggest poorer medical practice due, for example, to scant attention by the dermatologist. According to the dermatologists in our study, however, care was similar (75.9%) or even better (15.6%). The advantages of this kind of informal consultation for the requesters are evident: immediacy, no waiting, no cost, etc3; the disadvantages are not so clear, since care is of a quality similar to that provided in formal settings. It would, however, be interesting to know something of the circumstances (lighting, privacy, hygiene, etc) in which such consultations take place, given that many are made in less than ideal conditions in corridors, offices, meeting rooms, etc. The characteristics of this particular kind of consultation—type of patient, place of consultation, reason for consultation, etc—led Guberman et al3 to state that individuals making informal consultations should be called requesters and not patients. From the malpractice perspective, many of these cases, and especially the consultations on behalf of others, reflect what Sanz Rubiales et al4 call the recommendation syndrome. These authors concluded that many medical errors are the outcome of an attempt to offer more painstaking care to patients to whom the specialist is recommended, with the most important errors occurring due to the patient's own attitude, inefficient use of health care resources, failure to include data in medical histories, diagnostic test misinterpretations, and changes to standard indications and to treatment. Following appropriate procedures with patients would avoid many such errors.
In conclusion, our aim was, in the absence of similar studies, to analyze the burden of informal consultations in the routine work of the dermatologist. The requester profile is that of a female middle-aged nurse, who consults for the first time for a benign melanocytic tumor. The dermatologist typically prescribes empirical treatment or reassures and informs the patient, and rates the level of care as similar to that for a patient with a formal appointment. Nonregulated informal consultations increase the workload of dermatologists, but are a particular burden for trainee resident dermatologists in their first steps in patient care, given the great number of trivial complaints.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank Hospital Clínico San Cecilio de Granada dermatologists and especially resident dermatologists, and also participants at the 2009 Dermatology Residents’ Conference in Valencia, Spain, who honored this research with an award.
Please cite this article as: Almazán-Fernández FM, et al. Estudio de las consultas extraoficiales en un hospital de tercer nivel. Actas Dermosifiliogr.2011;102:805-809.